STD aneurysm
An atrial septal aneurysm is a minor cardiac anomaly that is a protrusion (bulging) of the thinned septum between the two atria.
Pathology, as a rule, with an aneurysm of the bladder, the functioning of the heart and the circulatory process are not disrupted; it is most often discovered by chance in children at an early age. Thus, it becomes clear what an aneurysm is.
It is important to know that the bulging of the wall between the atria does not itself imply the discharge of blood from one cavity to another, that is, an aneurysm of the sac aneurysm without discharge is an ordinary aneurysm, not complicated by rupture. https://www.youtube.com/embed/ghVCy40OaEs
It can be discharged only if a defect (hole) is formed between the left and right atrium. In this case, part of the blood from the left atrium will flow into the right, creating an increased load on it.
According to the ICD 10 classification, an aneurysm of the SPP is coded I25.3.
Types of aneurysm of the interatrial septum
There are three different forms of this minor cardiac anomaly, which depend on the direction of the bulge between the atria.
- Saccular protrusion occurs in the direction from the left atrium to the right - this option is more common than others, since higher pressure in the left atrium creates the prerequisites for this.
- The bulging of the wall between the atria has the opposite direction, i.e. from right to left - this option is possible with increased pressure in the cavity of the right atrium as a result of overload of the right parts of the heart.
- S-shaped protrusion, which suggests the existence of 2 protrusions simultaneously in different directions.
Symptoms
With an aneurysm of the bladder at the initial stages, the patient most often does not feel any changes in his body, since the hemodynamic process does not change. This situation should not cause concern and does not require specialized treatment.
Later, children may experience the following signs:
- Retarded physical and mental development of the baby, lack of body weight;
- Diseases of a viral nature are more common than among peers;
- At preschool and school age, reduced tolerance (endurance) of any physical activity occurs;
- delay in the development of sexual characteristics of a teenager;
- There may be a visual bulging of the chest area in the heart area.
Among the symptoms in adults, the possibility of rupture of an aneurysm in the aneurysm comes to the fore. This is possible in the presence of provoking factors: emotional shock, physical activity, chest injuries. This condition is not dangerous and does not require surgical treatment in most cases. This condition will manifest itself with the following symptoms:
- Sudden and acute pain in the heart;
- Interruptions in the heart;
- Severe fatigue, unmotivated;
- Prolonged feeling of heaviness and discomfort in the heart;
- The ability to engage in any physical activity for a long time.
Complications
STD aneurysm can be complicated by two conditions:
- Rupture of an aneurysm with the formation of a defect in the wall between the atria and the discharge of blood.
- The formation of blood clots with their subsequent separation and the development of heart attacks and strokes.
Treatment
The treatment tactics for this pathology depend on the time of development and the presence of complications.
So, in the first stages, treatment is not a necessary measure for such a minor cardiac anomaly. The only thing to do in such cases is to perform a clinical examination with a cardiologist.
If there is a threat of rupture or immediate rupture of the aneurysm between the atria, then treatment tactics are selected individually. The question of whether surgery is necessary is being decided.
. The surgical method is used extremely rarely, since open-heart intervention entails more consequences than a defect caused by a ruptured aneurysm.
Diagnosis of the disease
STD aneurysm (type R)
As mentioned earlier, STD aneurysm is a congenital developmental anomaly. Therefore, it can be detected without difficulty even in childhood. Another situation is observed if its progressive stretching has occurred, then for the first time it can be noticed at a more mature age.
The main methods for diagnosing an aneurysm are:
- Echocardiographic study. Ultrasound of the heart can reveal protrusion of the interatrial septum.
When an aneurysm is accompanied by the existence of a patent foramen ovale, the following methods may be informative:
- ECG is the simplest method. An electrophysiological study of the heart helps to see overload of the right side of the heart. Heart rhythm disturbances are also detected. In this case, signs of atrial fibrillation can be detected.
- X-ray of the chest organs. An aneurysm with a patent foramen ovale is characterized by the presence of a specific symptom on an x-ray - “pulsation of the roots of the lungs.”
- Echocardiographic study. As in the case of non-communicating aneurysm, this method is very important in diagnosing a patent foramen ovale. Thanks to this method, you can see the turbulence of the blood flow in the area of the hole. Valvular abnormalities may also be detected.
Instrumental diagnostics can also be supplemented by the following methods:
- Transesophageal ultrasound.
- Transthoracic ultrasound.
- CT scan.
- Catheterization of the heart chambers.
Prevention
Aneurysm of the interatrial septum in children
Preventive actions to prevent aneurysm of the interatrial septum are aimed at preventing a wide range of heart diseases.
These include:
- Healthy eating. You need to eat more fresh fruits and vegetables containing vegetable fats. But on the contrary, it is recommended to reduce animal fats;
- Restoring normal sleep and rest patterns. To maintain the nervous system and normal mental health, it is necessary to give the body sufficient time to recover, in the form of proper sleep and rest;
- Sports activities. It is recommended to devote up to thirty minutes a day to training. Especially physical education or exercise therapy. This is effective because heart function improves and excess weight decreases;
- Stress resistance. Emotional stress, nervous disorders and anxiety - all this affects the increase in heart rate. They have a bad effect on the functioning of the heart. Negative factors and too strong emotional impressions should be avoided;
- An hour a day for walking. Spend up to 60 minutes a day walking outdoors.
Diagnosis and treatment of AMPP
The main, effective method for detecting aneurysm of the interatrial septum in children is ultrasound examination of the heart, which is also called echocardiography. This procedure is characterized by absolute safety and the absence of any painful sensations for the child being examined. All clinics of the medical network in Makhachkala use the most modern ultrasound machines, which are staffed by highly qualified specialists, which makes it possible to reliably diagnose even the smallest patients with hidden, asymptomatic forms of pathologies.
If mild forms of aneurysm are detected in children, no special treatment is required. Such babies need to undergo a consultation with a cardiologist once a year after undergoing ultrasound diagnostics. Young patients are recommended to undergo gentle physical activity, avoid psycho-emotional stress, walks and games in the fresh air, good, long sleep and a balanced diet rich in vitamins, protein and microelements necessary for the child. Psychotherapy sessions and auto-training are very useful for children with AMPP. To improve cardiac activity, the attending physician usually also prescribes electrophoresis procedures with magnesium.
Complications
All about atrial septal defect in newborns and adults
But in adult patients, the following health problems are possible:
- Changes in heart rate (usually arrhythmias).
- Thromboembolic complications. The likelihood of blood clots increases when there is communication between the atria, which causes the formation of blood turbulence. Blood clots are dangerous; when they are delivered to the brain, they provoke a stroke, which can be fatal.
- Arterial hypotension is a chronic decrease in pressure with large pathologies.
- Violation of the integrity of the MPP.
| Negative factor | Explanation |
Size | The larger the area of the aneurysm, the higher the likely risks of violating its integrity. |
Physical exercise | The cause of such injury is often sudden heavy or intense loads for an unprepared person. In people with regular dosed training, this happens much less frequently. |
Bad habits | Tobacco smoking, addiction to alcohol and energy drinks, and frequent consumption of food prepared in fast food restaurants (excess weight is also harmful) increase the risk of perforation of the bladder. |
Stress and increased emotional background | This is more typical for teenagers, who bear the burden of hormonal changes. Added to this is excessive emotionality, uncontrollability in active recreation (sports, discos, etc.), chronic lack of sleep and various experiences characteristic of adolescence. |
Aging | Natural processes of wear and tear of tissue structures, changes in blood pressure, and the presence of various chronic diseases (including thrombosis and cholesterol deposits) can cause rupture of the bladder in the area of the aneurysm. |
Publications in the media
A cardiac aneurysm is an area of thinned myocardial tissue with protrusion of the ventricular wall in this area. This section covers only post-infarction cardiac aneurysms due to their significant epidemiological significance.
Statistical data • Post-infarction aneurysm complicates 10–35% of transmural MI • According to pathological studies, the incidence of post-infarction aneurysm is 8.5–34% • In men, cardiac aneurysms form 5–7 times more often than in women • Under the age of 40 years, post-infarction aneurysm occurs in 13% of people, and among people over 60 years of age - in 5.5%, which is due to the higher frequency of extensive transmural MI at a relatively young age • The frequency of formation of post-infarction aneurysms has a clear dependence on the strategy of early revascularization in individual clinics • Congenital Cardiac aneurysms formed from diverticula of the right ventricle and left ventricle (LV) are isolated cases; post-traumatic aneurysms are also rare.
Etiology • Acute post-infarction aneurysm (formed during acute transmural MI) is represented by necrotic tissue, chronic (forms at least 6-8 weeks, if there is no relapse of MI) - cicatricial • The formation of aneurysms is facilitated by arterial hypertension, the use of GCs, non-compliance by the patient with the regimen in acute period of MI.
Classification. The following types of post-infarction aneurysms are distinguished: • True aneurysms: •• diffuse; •• sac-like (with a narrow base); •• dissecting • False aneurysms - formed when the myocardial wall ruptures and limited to pericardial adhesions • Functional aneurysms - zones of viable (so-called hibernating) myocardium that has lost contractility and bulges during ventricular systole.
Pathogenesis • Contractile dysfunction in the area of the aneurysm is represented by akinesia (lack of contractile activity) and dyskinesia (bulging of the ventricular wall in systole and its retraction in diastole) • Hemodynamic disturbances are caused by the following mechanisms •• Decreased systolic function (when switched off from contraction more than 20–22 % LV area) •• Impaired diastolic function (impaired pressure-volume relationship leads to a disproportionate increase in end-diastolic pressure [EDP]) •• Mitral regurgitation (due to dilatation of the annulus fibrosus or damage to the papillary muscles) •• Thrombosis of the ventricular cavity ( observed in 40% of cases) • Compensatory mechanisms in the form of myocardial hypertrophy, changes in the configuration of the LV cavity and its dilatation (remodeling) lead to the progression of heart failure • Thromboembolism develops in 2–5% of patients, and in most patients, certain ventricular arrhythmias.
Clinical manifestations • Complaints •• Signs of heart failure - shortness of breath, episodes of pulmonary edema (20%) •• Rhythm disturbances - syncope episodes and a feeling of interruptions in the heart (35%) •• Thromboembolism, usually occurring in the femoropopliteal or iliac segments, less often - in the brachiocephalic trunk, and ischemia of the viable myocardium, for example angina pectoris (60%) • Objective examination data •• Signs of circulatory failure - tachypnea, moist rales in the basal parts of the lungs, later - edema, ascites, hepatomegaly •• Symptoms of mitral regurgitation - see Mitral valve insufficiency •• Signs of previous embolisms are focal neurological defects, absence of pulsation in the arteries of the lower extremities.
Instrumental diagnostics
• ECG •• There are no pathognomonic signs •• Signs of previous MI •• There is no dynamics of ST segment displacement, characteristic of an uncomplicated course of MI (“frozen” MI) •• In 85% of cases, post-infarction changes are localized in the anterolateral region.
• EchoCG •• Visualization of the aneurysm cavity, measurement of its size, assessment of the configuration of the aneurysm and diagnosis of thrombosis of the LV cavity •• Calculation of the index of local contractility disorders •• Stress test to identify viable myocardium in the area of the aneurysm •• Differentiation of true and false aneurysms (highly specific method) •• Identification and functional assessment of mitral regurgitation (see Mitral valve insufficiency).
• X-ray of the chest organs •• Cardiomegaly due to bulging of the LV arch or local bulging along the left contour of the heart shadow •• When performing kymography - paradoxical pulsation in the area of the aneurysm •• Symptoms of congestion in the pulmonary circulation (increased pulmonary pattern, expansion and lack of structure of the roots of the lungs , Kerley lines type B).
• Radioisotope ventriculography •• Determination of the location and size of the aneurysm, thrombosis of its cavity •• Calculation of volumetric indicators of the LV and assessment of its contractile function at rest and during pharmacological testing.
• MRI allows you to obtain the same information as radiopaque ventriculography •• Performed when radiopaque ventriculography is contraindicated •• A highly specific method for detecting LV thrombosis •• Three-dimensional reconstruction of the LV cavity is possible (important information for determining surgical tactics).
• Perfusion scintigraphy or single photon emission CT of the myocardium: detection of perfusion defects in the aneurysm and other areas at rest and during pharmacological testing.
• Positron emission tomography of the myocardium: identification of viable myocardium in the area of the aneurysm and other areas.
• X-ray contrast left ventriculography •• Determination of the location and size of the aneurysm, thrombosis of its cavity •• Calculation of volumetric indicators of the LV and assessment of its contractile function •• Calculation of the area of the aneurysm (using the central angle method or graphic integration) and the contractile part of the LV.
• Catheterization of the left atrium and LV: increased EDP, systolic blood pressure, diastolic blood pressure.
• Coronary angiography •• Performed in all candidates for surgical treatment and in patients in whom noninvasive testing reveals ischemic viable myocardium.
• Electrophysiological study is performed in patients with ventricular arrhythmias in the presence of clinical manifestations.
TREATMENT
Drug therapy - see Ischemic heart disease, Chronic systolic cardiac failure, Mitral valve insufficiency.
Surgery
• Indications •• Large size of the aneurysm (more than 22% of the LV wall area) in the presence of the following clinical indications: ••• anginal pain ••• clinically significant heart failure ••• ventricular arrhythmias ••• LV wall rupture ••• pseudoaneurysm • •• congenital aneurysm ••• thromboembolism ••• asymptomatic aneurysms with a progressive increase in their size •• Severe mitral regurgitation.
• Relative contraindications •• Asymptomatic aneurysms of stable size, even if these patients are scheduled for coronary bypass surgery •• High anesthetic risk •• Inability to restore myocardial function outside the aneurysm area, cardiac index <2.0 l/min/m2 •• Confirmed non-transmural perfusion defect ( the presence of hibernating myocardium in the area of the aneurysm) •• Progressive mitral regurgitation.
• Methods of surgical treatment •• Palliative interventions - support-ring mitral anuloplasty according to Carpentier •• Radical interventions ••• Resection of aneurysm ••• In the presence of an aneurysm of the interventricular septum - septoplasty according to Cooley ••• For large aneurysms - resection followed by reconstruction of the LV with a patch according to Jatin-Dor ••• In case of rupture of the free wall of the LV, post-traumatic and false aneurysms - suturing of the rupture of the LV wall ••• If it is necessary to perform revascularization interventions, preference is given to coronary bypass surgery, performed in one stage with surgery for the aneurysm.
Specific postoperative complications • Small output syndrome - 22-39% • Rhythm disturbances - 9-19% • Respiratory failure - 4-11% • Bleeding - 4-7% • Acute vascular insufficiency with the need for dialysis - 4% • Acute cerebrovascular accident - 3–4%.
Prognosis • In the absence of clinical symptoms, the prognosis is favorable: more than 2/3 of patients do not develop symptoms within 10 years • 10-year survival rate in the absence of clinical manifestations is 90%, in patients with symptoms of the disease - 46% • Despite the fact that Early studies demonstrated low survival rates in patients receiving drug treatment (12% at 5 years), the use of angiotensin-converting enzyme (ACE) inhibitors, control of thrombus formation and arrhythmias, according to recent studies, increases 5-year survival to 47– 70% • Among the causes of death, 44% are rhythm disturbances, 33% are heart failure, 11% are recurrent MI, 22% are noncardiac causes • Factors influencing the prognosis in patients receiving drug therapy - age, cardiac class insufficiency according to NYHA (USA), the presence of anginal episodes, mitral regurgitation, ventricular arrhythmias, aneurysm volume, ejection fraction • In patients with thrombosis of the LV cavity identified by echocardiography, the risk of thromboembolism is 19% within 24 months • The risk of thromboembolism against the background of a short course of anticoagulant therapy is 0.35% per year; Long-term treatment with anticoagulants in these patients does not improve the prognosis • Factors influencing the risk of thromboembolism are aneurysm volume and atrial fibrillation • With surgical treatment, in-hospital mortality is 2-19% (average 9.9%), in more recent reports - 3- 7% • Factors that increase in-hospital mortality are age, incomplete revascularization, high class of heart failure, female gender, urgency of intervention, left ventricular ejection fraction less than 20–30%, the need for simultaneous mitral valve replacement, refusal to use the internal mammary artery • Distant results vary among patient populations •• 5-year survival - 58-80% •• 10-year overall survival - 34% •• 10-year cardiovascular event-specific survival - 57% • Cause of most cardiovascular events deaths becomes recurrent MI • Preoperative factors that increase long-term mortality are age, class of heart failure, ejection fraction less than 35%, cardiomegaly according to radiography, CDP >20 mm Hg, mitral regurgitation.
Abbreviations • LV - left ventricle • EDP - end diastolic pressure.
ICD-10 • I25.2 Past MI • I25.3 Cardiac aneurysm
Causes of development of aneurysm of the sacral tract
An aneurysm forms in the place where the oval window functioned during fetal life. This is the hole through which the blood moved directly into the left atrium, starting a large circle. There was no need to pump it into the lungs, since the respiratory organs were not working. After birth, the first breath of the newborn and the intersection of the umbilical cord, the pulmonary circulation begins its work. The hole between the atria closes almost immediately, but sometimes this process can take up to a year, which is not considered a pathology.
If the connective tissue, which, together with the muscle fibers, tightens the oval window, is not strong enough, under pressure it begins to stretch and prolapse in one direction or another.
Reliable reasons for the intrauterine development of an aneurysm of the sac have not yet been established, but it is believed that infections suffered by the mother during pregnancy, stress, the use of certain medications, smoking and alcohol consumption can significantly affect the formation of the cardiovascular system of the unborn child. Factors such as unfavorable environmental conditions, lack of microelements and vitamins in the pregnant woman’s diet, as well as genetic disorders that can lead to connective tissue dysfunction are taken into account.
Often, with hereditary dysplasia, not only the heart suffers, but also the joints, bones and even the lens of the eye. With such pathologies, the structure or properties of connective tissue change. The interatrial septum becomes flaccid, does not resist the pressure inside the chambers of the heart and stretches.
The same mechanism occurs when scarring occurs in the area of the myocardium in which the infarction occurred. Despite the fact that MI most often affects the interventricular septum, aneurysm in adults affects the prognosis of survival and can be complicated by ruptures and thromboembolism of cerebral vessels, which, in turn, is the direct cause of ischemic stroke.
There are three types of SST aneurysms:
- With a deflection into the right atrium.
- With a deflection into the left atrium.
- S-shaped aneurysm.
The direction of the deflection does not matter, since the symptoms are the same, but when combined with other heart defects and the occurrence of hemodynamic disorders, the manifestations become more pronounced.
If the prolapse of the interatrial septum occupies a large area or reaches pathological values, this may lead to the organization of blood clots due to turbulent flow in the aneurysm, heart rhythm disturbances due to additional stimulation of the conduction system, circulatory dysfunction due to the lack of normal emptying of the atrium during contraction. Severe bulging can interfere with valve function. If there is a shunt (discharge) of blood from left to right due to an unclosed oval window or rupture of an aneurysm, pulmonary hypertension develops due to overload of the small circle.
Symptoms and manifestations
In newborns and children of preschool and younger age, an aneurysm of the interatrial septum most often does not manifest itself in any way. However, due to growth spurts in adolescence, during physical and stressful activities and during pregnancy, it can manifest itself with symptoms that vary in the degree of manifestation in each individual case:
- Heart rhythm disturbances;
- Reduced resistance to stress;
- Interruptions in heart function;
- Chest pain;
- Dizziness;
- Nausea;
- Blueness of the tip of the nose and nasolabial triangle during exercise and when breastfeeding a newborn;
- Headache;
- Tachycardia;
- Anxiety;
- Sleep disorders;
- Psychological discomfort in children and adolescents.
In combination with other heart defects, more serious manifestations come to the fore:
- Frequent viral infections of the upper respiratory tract;
- Chronic bronchitis;
- Dyspnea;
- Edema.
In patients who have survived acute myocardial infarction and have developed an adult atrial septal aneurysm larger than 10 mm according to ultrasound, there is some risk of rupture. Mortality is high, but this condition occurs very rarely.
Clinical manifestations develop acutely and at high speed:
- Paleness, turning into bluishness of the skin of the face and palms;
- Loss of consciousness;
- Noisy breathing;
- Cold clammy sweat;
- Dyspnea.
How is atrial aneurysm treated?
Aneurysm of the membranous part of the interventricular septum is treated with the same methods as other types of similar pathologies. Once the disease is identified, drug treatment is usually prescribed, during which the doctor monitors the growth of the aneurysm. The following drugs are used:
- Medicines that stimulate the production of collagen are needed to strengthen the walls of blood vessels;
- B vitamins;
- Microelements including zinc and copper;
- Medicines to relieve blood pressure if the patient is prone to hypertension;
- Drugs that resolve blood clots;
- Medicines to regulate heart rate.
The medicinal method is used for small pathologies, but if accelerated growth is observed, surgical intervention cannot be avoided. During the operation, the doctor’s task is to strengthen the walls of the aneurysm. The following methods are used:
- A synthetic patch is installed;
- Sutures are placed through a small hole;
- The oval window is closed using an endoscope.
Surgical treatment does not exclude the use of medications during the rehabilitation period. You will also have to take medications that strengthen blood vessels, vitamins and minerals. It is required to comply with all recommendations and prescriptions of the doctor for the treatment to be successful.
Symptoms of pathology
With growing up, growth retardation becomes more noticeable; the child cannot tolerate physical activity on a par with peers, often gets tired and feels pain in the heart area. A medical examination reveals pallor of the skin, structural changes in the chest in the area of pathology (protrusion), tachycardia and increased blood pressure.
After an accurate diagnosis has been established, patients need to regularly visit a cardiologist to identify changes in pathology through specific examinations. Such actions are aimed at preventing aneurysm rupture, which is most often observed in adolescent children.
In adults, the signs of an aneurysm are varied, which is associated with both the location and size of the tumor. Since the development of cardiac aneurysm is observed quite often in the post-infarction period, the patient needs to monitor changes in well-being and not miss examinations by a cardiologist.
The main symptoms of cardiac aneurysm in adulthood:
- pain in the heart area;
- regular weakness;
- rhythm disturbances, feeling of increased heartbeat;
- shortness of breath after minor physical exertion;
- pale skin;
- cough without the appearance of other signs of colds.
In early childhood, the course is usually asymptomatic. However, the reason for a thorough examination, incl. cardiological, where an aneurysm is usually detected - should be a child’s lagging behind in psychophysical development, insufficient body weight, frequent acute respiratory viral infections;
The severity of this symptom complex varies widely - from severe to insignificant, not significantly affecting the quality of life and overall development. The greatest danger is rupture of an aneurysm with the formation of an interatrial defect (message), as a result of which the normal, natural hemodynamics of the myocardium are disrupted.
However, it is no coincidence that this development of events is called unpredictable above: in some cases, the acquired defect allows you to lead a completely normal lifestyle for decades, in others it creates the threat of a stroke or the so-called.
sudden cardiac death. After 40 years of age, a patient with a defect in the bladder, formed as a result of a rupture of an aneurysm, often has to be disabled due to increasing hemodynamic disturbances and risks.
In diagnosis, in addition to anamnesis, the results of clinical examination and observation, ultrasound echocardiography (EchoCG) is of greatest importance, which has virtually no contraindications, allows repeated studies over time and allows for visualization of the aneurysm with an accurate assessment of its characteristics.
At the very beginning of the disease, there are no certain signs; the presence of the disease can only be determined during an examination. A hole appears where the aneurysm is located. Because of this, circulatory disorders occur.
As a result, compensatory hypertrophy of the right atrium occurs, and then the ventricle. In addition, an increased amount of blood enters the lungs, increasing the load on the vessels and causing symptoms of pulmonary hypertension. In children, development occurs more slowly.
In adults, the risk of aneurysm rupture is much higher. This can occur due to a constant state of stress, heart injury, or increased physical activity. When an aneurysm ruptures, the patient experiences the following symptoms:
- heartache;
- increased body fatigue;
- inability to carry out prolonged physical activity;
- feeling of discomfort in the heart area;
- disruptions in the functioning of the heart.
Aneurysm of the interatrial septum (interatrial septum) is classified as a so-called minor cardiac anomaly that does not cause significant circulatory disorders or changes in heart function. This is a rare defect of newborns, occurring in no more than 1% of cases and usually asymptomatic.
Young mothers who are faced with such an anomaly in their child should not panic - an aneurysm of the sac is not life-threatening, children develop correctly, and as the aneurysm grows, it may spontaneously disappear.
An MPP aneurysm can be isolated, but much more often it is combined with other heart defects and a patent foramen ovale, so the symptoms can be varied, but are not always associated specifically with the aneurysm.
Atrial septal defect
Atrial septal defect (ASD) is the second most common congenital heart defect.
With this defect, there is a hole in the septum that separates the right and left atria into two separate chambers. The fetus, as we said above, not only has this hole (open oval window), but is also necessary for normal blood circulation. Immediately after birth it closes in the vast majority of people. In some cases, however, it remains open without people being aware of it. The discharge through it is so insignificant that a person not only does not feel that “there is something wrong with the heart,” but he can calmly live to a ripe old age. (It is interesting that, thanks to the capabilities of ultrasound, this defect in the interatrial septum is clearly visible, and in recent years, articles have appeared that show that among such adults and healthy people who cannot be classified as patients with congenital heart disease, there is a significantly higher number of people suffering from migraines - severe headaches. These data, however, have yet to be proven).
Unlike patent foramen ovale, true atrial septal defects can be very large. They are located in different parts of the septum itself, and then they speak of a “central defect” or “a defect without an upper or lower edge,” “primary” or “secondary.” (We mention this because the type and location of the hole may depend on choice of treatment type).
If there is a hole in the septum, a shunt occurs with blood discharge from left to right. With an ASD, blood from the left atrium partially flows into the right atrium with each contraction. Accordingly, the right chambers of the heart and lungs become overfilled, because they have to pass through themselves a larger, extra volume of blood, and one more time that has already passed through the lungs. Therefore, the pulmonary vessels are filled with blood. Hence the tendency to pneumonia. The pressure in the atria, however, is low, and the right atrium is the most “distensible” chamber of the heart. Therefore, while increasing in size, it copes with the load for the time being (usually up to 12-15 years, and sometimes more) quite easily. High pulmonary hypertension, which causes irreversible changes in the pulmonary vessels, never occurs in patients with ASD.
The vast majority of newborns, infants, and young children grow and develop absolutely normally. Parents may notice their tendency to frequent colds, sometimes resulting in pneumonia, which should be alarming. Often these children, in 2/3 of cases girls, grow up pale, thin and somewhat different from their healthy peers. They try to avoid physical activity as much as possible, which in the family can be explained by their natural laziness and reluctance to tire themselves out.
Heart complaints can and, as a rule, appear in adolescence, and often after 20 years. Usually these are complaints about “interruptions” in the heart rhythm that a person feels. Over time, they become more frequent, and sometimes lead to the patient becoming incapable of normal, ordinary physical activity. This does not always happen: G.E. Falkowski once had to operate on a patient aged 60, a professional driver, with a huge atrial septal defect, but this is an exception to the rule.
To avoid such a “natural” course of the defect, it is recommended to close the hole surgically. Unlike a VSD, an interatrial defect will never heal on its own.
Surgery for ASD is performed under artificial circulation, on an open heart, and consists of suturing the hole or closing it with a patch. This patch is cut out from the heart sac - the pericardium - the sac surrounding the heart. The size of the patch depends on the size of the hole. It must be said that the closure of an ASD was the first open-heart surgery, and it was performed more than half a century ago.
Sometimes an atrial septal defect can be combined with an irregular, anomalous entry of one or two pulmonary veins into the right atrium instead of the left. Clinically, this does not manifest itself in any way, and is a finding when examining a child with a large defect. This does not complicate the operation: the patch is simply larger and is made in the form of a tunnel in the cavity of the right atrium, directing blood oxidized in the lungs to the left parts of the heart.
Today, in addition to surgery, in some cases it is possible to safely close the defect using X-ray surgery
technology. Instead of suturing the defect or sewing in a patch, it is closed with a special umbrella-shaped device - an occluder, which is passed along the catheter in a folded form and opened, passing through the defect.
This is done in the X-ray surgery room, and we described everything related to such a procedure above when we touched on probing and angiography. Closing a defect with such a “non-surgical” method is not always possible and requires certain conditions: anatomical location of the hole, sufficient age of the child, etc. Of course, if they are present, this method is less traumatic than open-heart surgery. The patient is discharged after 2-3 days. However, it is not always feasible: for example, in the presence of abnormal vein drainage.
Today, both methods are widely used, and the results are excellent. In any case, the intervention is elective and not urgent. But it needs to be done in early childhood, although it can be done earlier if the frequency of colds and, especially, pneumonia becomes frightening and threatens bronchial asthma, and the size of the heart increases. In general, the sooner the operation is performed, the sooner the child and you will forget about it, but this does not mean that you should be in a particular hurry with this defect.
How to get treatment at the Scientific Center named after. A.N. Bakuleva?
Online consultations
Symptoms
Like any other disease, atrial septal aneurysm in young children has its own symptoms. Usually, babies under one year old do not feel any symptoms. And even if they are present, it will be extremely difficult for parents to find out about them, because a child under about 2 years of age will not be able to clearly explain what is happening to him and what is bothering him.
- Cough. If a child has a strong barking cough, but there are no other signs of acute respiratory infections, then in this case parents should take note of this symptom;
- Dyspnea. If the baby does not suffer from excess weight, but is still bothered by shortness of breath, then this only indicates one thing: that there are malfunctions in the functioning of the heart;
- Snore. Of course, such a harmless symptom cannot indicate an aneurysm of the bladder, but if it is accompanied by the above symptoms in total, then most likely the child should be shown to a cardiologist.
Older children, starting from about 3 years old, can already explain to the parent what is bothering him; with an aneurysm, the child will complain of pain in the chest or back, as well as when swallowing.
In addition to the symptoms that indicate the presence of a septal aneurysm in a child, there are symptoms that indicate a ruptured aneurysm. In this case, no detail should be missed; you must act quickly, otherwise this situation can lead to death.
- Symptoms of a ruptured aneurysm:
- A sharp and significant decrease in pressure. When an aneurysm ruptures, blood flows freely from the vessel, causing the pressure on the walls to drop sharply;
- The occurrence of very sharp and severe pain in the area of the heart or shoulder blades;
- Labored breathing;
- Tachycardia;
- The appearance of pale skin;
- The child stops responding to various stimuli;
- The child does not move or speak.
MPP does not have specific symptoms, so the disease is difficult to detect. The signs differ for different age groups:
- Up to 3 years. Slow development, underweight, poor immunity, general malaise. Sometimes you can observe an increase in the volume of the right ventricle and overload of the pulmonary circulation.
- Up to 7 years old. Stunted growth, fatigue, weakness, increased first tone when listening, rarely arrhythmia.
- Teenage years. Strengthening of the second tone when listening, pallor of the skin, enlargement of the pulmonary trunk and right atrium, protrusion in the heart area, decreased pulse and blood pressure.
- In adults, shortness of breath, heart failure, dizziness, and fatigue are observed.
At any age, MPP is characterized by chest pain. The pain can vary in strength and nature, usually sharp and aching.
Signs of an aneurysmal condition vary between children and adults. The intensity of the symptomatic picture also depends on the degree of the pathological process. In adults, MPP may not have any clinical manifestations.
Often an acquired minor defect is discovered by chance during a comprehensive examination. Symptoms such as shortness of breath, rapid heartbeat, and increased fatigue may appear.
Aneurysm of the interatrial septum in children has various manifestations and depends on the age of the child:
- Infants up to 3 months: slow weight gain, retardation in physical and mental development.
- From 3 to 7 years: rapid fatigue, arrhythmia, when listening to the heart, an increase in the first tone is noted.
Aneurysmal protrusion in adolescents has the following common manifestations:
- increased heart rate;
- increased fatigue that occurs after minor physical activity;
- pathological nature of the heart rhythm;
- discomfort in the sternum;
- attacks of dizziness;
- increased sweating;
- nausea;
- fainting conditions;
- the occurrence of frequent abdominal pain;
- prolonged headache;
- severe drowsiness.
Diagnostics
An aneurysm of the bladder is determined by ultrasound diagnostics.
Knowing what an atrial septal aneurysm is, you can predict possible complications. To detect them, advanced diagnostics are performed - ECG, CT.
Brain aneurysms
Department of Emergency Neurosurgery > Diseases
Content:
1. Structure of an aneurysm 2. Classification of aneurysms 3. Causes of cerebral aneurysms 4. Clinical picture of aneurysm rupture 5. Instrumental diagnosis 6. Complications of non-traumatic subarachnoid hemorrhage 7. Assessment of the severity of the patient’s condition 8. Surgical treatment of aneurysms 9. Postoperative management 10. Outcomes
A cerebral aneurysm (cerebral aneurysm, intracranial aneurysm) is a protrusion of the wall of an artery. Aneurysms are characterized by the absence of a normal, three-layer structure of the vascular wall. The wall of the aneurysm is represented only by connective tissue; the muscle layer and elastic membrane are absent. Rupture of a cerebral aneurysm is the most common cause of non-traumatic subarachnoid hemorrhage (more than 50%), in which blood enters the subarachnoid space of the brain.
Non-traumatic subarachnoid hemorrhage (NSAH) is one of the most severe and common forms of cerebrovascular accident. In the Russian Federation, the incidence of NSAC is about 13:100,000 population per year.
Most often, aneurysm rupture occurs in patients aged 40 to 60 years.
For the first time, a cerebral aneurysm was described in section by the Italian JB Morgagni in 1725. The first cerebral angiography for NSAC was performed in 1927 by the Portuguese E. Moniz, and in 1937 the American WE Dandy performed the first microsurgical intervention for the rupture of a cerebral aneurysm with its exclusion from the bloodstream using a silver clip.
At the Research Institute of SP named after. N.V. Sklifosovsky, the first operations for ruptured cerebral aneurysms began in 1979 under the leadership of Professor V.V. Lebedev.
Patients with cerebral aneurysms are admitted to our clinic mainly for emergency reasons.
Over the course of a year, the institute’s staff carries out more than 2,000 on-site consultations in hospitals in Moscow, of which about 40% are for patients with NSAC. At the Research Institute of SP named after N. During the year, V. Sklifosovsky’s visiting advisory team transfers more than 250 patients with ruptured cerebral aneurysms.
1. Structure of the aneurysm
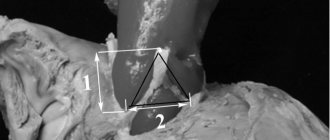
An aneurysm is divided into a neck, body and dome. The neck of the aneurysm retains the three-layer structure of the vascular wall, therefore it is the most durable part of the aneurysm, while the dome is represented by only one layer of connective tissue, therefore the aneurysm wall in this part is the thinnest and most often susceptible to rupture (Fig. 1).
Rice. 1. The structure of the aneurysm during cerebral angiography: 1 - dome, 2 - body, 3 - neck, marked with a dotted line.
2. Classification of aneurysms
By form:
- saccular (Fig. 2)
- fusiform
- Fusiformes.
A)
b)
Fig. 2. Macroscopic specimens of cerebral aneurysms: a) giant saccular aneurysm of the anterior communicating artery; b) saccular aneurysm of the fork of the middle cerebral artery. Aneurysms are indicated by arrows.
By size:
- milliary (diameter up to 3 mm)
- regular size (4-15 mm)
- large (16-25mm)
- gigantic (more than 25 mm).
By the number of chambers in the aneurysm:
- single-chamber
- multi-chamber.
By localization:
- on the anterior cerebral - anterior communicating arteries (45%)
- on the internal carotid artery (26%)
- on the middle cerebral artery (25%)
- on the arteries of the vertebrobasilar system (4%)
- multiple aneurysms – on two or more arteries (15%).
3. Causes of cerebral aneurysms
Currently, there is no single theory of the origin of aneurysms. Most authors agree that the origin of aneurysms is multifactorial. There are so-called predisposing and producing factors.
Predisposing factors include those factors that result in changes in the normal vascular wall:
- hereditary factor - congenital defects in the muscular layer of the cerebral arteries (type III collagen deficiency), most often observed in places where the arteries bend, bifurcate or branch off from the artery of large branches. As a result, cerebral aneurysms are often combined with other developmental pathologies: polycystic kidney disease, hypoplasia of the renal arteries, coarctation of the aorta, etc.
- arterial injury
- bacterial, mycotic, tumor embolism
- exposure to radiation
- atherosclerosis, hyalinosis of the vascular wall.
Producing factors are those that directly result in the formation and rupture of an aneurysm.
The main producing factor is hemodynamic - an increase in blood pressure, a change from laminar blood flow to turbulent one. Its effect is most pronounced in places of arterial bifurcation, when an already altered vascular wall is subject to constant or periodic exposure to impaired blood flow. This leads to thinning of the vascular wall, the formation of an aneurysm and its rupture. 4. Clinical picture of aneurysm rupture
The symptoms of aneurysm rupture depend on the anatomical form of the hemorrhage, the location of the aneurysm, and the presence of complications of intracranial hemorrhage.
The typical clinical picture of aneurysm rupture develops in 75% of patients and has both general signs of non-traumatic subarachnoid hemorrhage and a number of features.
The disease most often begins suddenly with a severe headache of the “blow” type, which can be accompanied by nausea and vomiting, often against the background of physical activity, psycho-emotional stress, and increased blood pressure. The resulting headache is of a “burning”, “bursting” nature. Short-term and sometimes long-term disturbances of consciousness of varying degrees of severity (from moderate stupor to atonic coma), hyperthermia, and psychomotor agitation may occur.
Meningeal symptoms are observed in almost all cases of NSAH: the patient has a stiff neck, photophobia, increased sensitivity to noise, Kernig's, Brudzinsky's symptoms, etc.
Depending on the location of the aneurysm, various focal symptoms may occur:
- Aneurysms of the internal carotid artery are characterized by headache localization in the frontal or paraorbital region; Visual disturbances, paresis of the oculomotor nerve, contralateral hemiparesis, and sensory disturbances in the area of innervation of the I-II branches of the trigeminal nerve may occur.
- Rupture of an anterior cerebral - anterior communicating artery aneurysm is often accompanied by mental changes (emotional lability, psychotic disorders, decreased intelligence, memory impairment, concentration disorders, etc.). Electrolyte disturbances, diabetes insipidus, and contralateral hemiparesis, more pronounced in the leg, may be observed.
- rupture of an aneurysm of the middle cerebral artery is characterized by the development of contralateral hemiparesis, more pronounced in the arm, or hemiplegia, contralateral hemihypesthesia, motor and/or sensory aphasia (with damage to the dominant hemisphere), visual impairment such as homonymous hemianopia, and convulsive seizures.
- with aneurysms of the basilar artery, unilateral or bilateral paresis of the oculomotor nerve, Parinaud's symptom, vertical or rotatory nystagmus, and ophthalmoplegia often occur. Alternating syndromes, homonymous hemianopsia or cortical blindness, and the development of tetraparesis are possible. With massive hemorrhage, the level of consciousness is depressed to the point of coma, the patient has wide pupils without a photoreaction, and breathing problems occur.
- Aneurysms of the vertebral artery are characterized by the occurrence of dysphagia, dysarthria, hemiatrophy of the tongue, impairment or loss of vibration sensitivity, decreased pain and temperature sensitivity, and dysesthesia in the legs. With massive hemorrhage - coma, respiratory failure.
In approximately every 4 patients (about 25%), atypical variants of the course of aneurysm rupture are observed, when the hemorrhage is “masked” as other diseases.
Such patients may be diagnosed with “hypertensive crisis”, “migraine”, “acute food poisoning”, “acute psychosis”, “sciatica”, “meningitis”, etc., which leads to hospitalization of patients in non-core institutions and untimely provision of necessary medical care . When cerebral aneurysms rupture, both subarachnoid hemorrhage itself and intracerebral and/or intraventricular hemorrhage can occur.
With all anatomical forms of hemorrhage, occlusion of the cerebrospinal fluid pathways may occur with the development of acute occlusive hydrocephalus and brain dislocation.
5. Instrumental diagnostics
To identify non-traumatic subarachnoid hemorrhage due to rupture of aneurysms, determine the prognosis of the disease, the likelihood of complications, and develop treatment tactics, a number of instrumental diagnostic methods are used.
Lumbar puncture – makes it possible to detect subarachnoid hemorrhage with a high degree of probability. On the first day after hemorrhage, the cerebrospinal fluid is intensely and evenly colored with blood; after a few days it becomes xanthochromic. Puncture is contraindicated if the patient has an intracranial space-occupying process (hematoma, massive ischemic focus), since even a small removal of cerebrospinal fluid can lead to the development of acute dislocation of the brain stem. In order to avoid this, patients with clinical manifestations of an intracranial space-occupying process should undergo echoencephaloscopy or computed tomography of the brain before lumbar puncture.
Computed tomography of the brain (CT) is the leading method for diagnosing NSAH, especially in the first day of the disease. Using CT, not only the presence of hemorrhage is determined, but also its intensity, prevalence, the presence and volume of intracerebral hematoma and intraventricular hemorrhage, foci of ischemia, the severity and nature of hydrocephalus, and dislocation syndrome.
In addition, with the help of CT of the brain, it is sometimes possible to establish the true cause of hemorrhage, topographic-anatomical relationships, especially if the study is supplemented with contrast enhancement and 3D reconstruction.
The detection rate of NSAC in the first 12 hours after hemorrhage using CT reaches 95.2%, within 48 hours - 80-87%, on days 3-5 - 75%, on days 6-21 - only 29%. Severe basal SAH is almost always prognostically unfavorable, since in almost all patients it is accompanied by the development of vasospasm, leading to the development of ischemia. The high information content of brain CT and the prognostic significance of the results obtained, as well as the speed of the study, make this method mandatory when examining patients with ruptured cerebral aneurysms (Fig. 3).
A)
b)
V)
Rice. 3. a) Computed tomography of the brain. Massive basal subarachnoid hemorrhage due to rupture of an aneurysm of the anterior communicating artery (indicated by arrows); b) CT angiography of intracranial arteries (2D reformation). Fusiform aneurysm of the right internal carotid and anterior cerebral arteries. c) CT angiography of intracranial arteries (3D reformation). Saccular aneurysm of the bifurcation of the left internal carotid artery. Aneurysms are indicated by arrows.
Magnetic resonance imaging (MRI) - this diagnostic method has high sensitivity and specificity. If CT of the brain has excellent detection of SAH and aneurysms in the acute period of hemorrhage, then MRI is indispensable in detecting hemorrhages in the subacute and chronic periods. Verification of aneurysms with magnetic resonance angiography (MR-AG) reaches 80-100%, which allows in some cases to abandon traditional invasive cerebral angiography (CAG) when for some reason it is contraindicated (for example, with individual intolerance to iodine preparations) (Fig. . 4).
A)
b)
Rice. 4. a) Magnetic resonance imaging. Partially thrombosed aneurysm of the right internal carotid artery. b) MR angiography of intracranial arteries. Saccular aneurysm of the anterior communicating artery. Aneurysms are indicated by arrows.
During an MRI examination, the hemorrhage appears as hyperintense (bright) or hypointense (dark) on the resulting images, depending on the duration of the hemorrhage.
Also, MRI of the brain with a high degree of reliability allows you to verify ischemia and determine its nature.
Digital subtraction cerebral angiography is the “gold standard” for the most accurate identification of the cause of hemorrhage. It is mandatory to study two carotid and two vertebral basins in direct, lateral and oblique projections.
Cerebral angiography can not only detect an aneurysm (Fig. 5), but also vascular spasm (Fig. 9b).
A)
b)
Rice. 5. Cerebral angiography. a) Cerebral angiogram in direct projection. Aneurysm of the left internal carotid artery. b) Cerebral angiogram in lateral projection. Aneurysm of the anterior communicating artery. Aneurysms are indicated by arrows.
Electroencephalography (EEG) is an instrumental diagnostic method that allows you to identify disturbances in the electrical activity of the brain. When recording the electrical activity of the brain in SAH, the type of EEG is determined. Determining the type of disturbance in the electrical activity of the brain allows us to clarify the timing of the operation.
So, with EEG types I and II, surgical interventions for ruptured aneurysms have a favorable prognosis. In type III, surgical intervention is not advisable, although it is possible with a high risk of re-rupture of the aneurysm. Type IV is the most unfavorable prognostically. There are pronounced disturbances in the electrical activity of the brain. Surgery with this type of EEG can only be performed for health reasons (for example, in case of acute compression of the brain by a hematoma) (Fig. 6).
a) b)
Rice. 6. EEG in case of rupture of a cerebral aneurysm: a) type I; b) IV type.
An electroencephalographic study in a situation where there are multiple aneurysms and it is unclear which of them is the cause of the hemorrhage, makes it possible to identify a ruptured aneurysm (usually by the predominance of changes in electrical activity in a particular area of the brain).
Transcranial Dopplerography (TDCG) is a method that can significantly expand the diagnosis of vasospasm. With TDCG, it is possible to determine the linear blood flow velocity (LBV) in the main arteries of the brain, the severity of spasm (the degree of narrowing of the artery lumen), the localization of spasm and the dynamics of its development. When the linear speed of blood flow through the arteries of the base of the brain increases above 120 cm/s, vascular spasm is considered moderate; when the blood flow speed exceeds 200 cm/s, it is pronounced. Angiospasm is assessed as non-widespread if it covers 1-2 arteries of the circle of Willis, and widespread when there is spasm of 3 or more arteries (Fig. 7).
a) b)
Rice. 7. a) TCD, norm: average blood flow velocity in the middle cerebral artery – 90 cm/s; b) TCD, vasospasm: the average blood flow velocity in the middle cerebral artery is 260 cm/s.
With increasing vascular spasm and the presence of clinical manifestations, surgical intervention is possible only with increasing dislocation of the brain due to intracranial hematoma or ischemia causing mass effect.
6. Complications of non-traumatic subarachnoid hemorrhage
The most common complications of subarachnoid hemorrhage due to aneurysm rupture include the following:
- Recurrent rupture of the aneurysm (Fig. 8).
A)
b)
V)Rice. 8. a) CT scan of the brain. First rupture of anterior communicating artery aneurysm. b) Cerebral angiography, lateral projection, aneurysm of the anterior communicating artery is indicated by an arrow. c) CT scan of the finished brain. Repeated rupture (after 3 days) of the anterior communicating artery aneurysm (hemorrhage is indicated by an arrow).
- Cerebral vasospasm (peak development 3-14 days after aneurysm rupture).
- Cerebral ischemia develops in more than 60% of patients with SAH, and in 15-17% of patients it is the main cause of death after aneurysm rupture (Fig. 9).
A)
b)
V)Rice. 9. a) CT scan of the brain. Massive basal subarachnoid hemorrhage (indicated by arrows). b) Cerebral angiogram, oblique projection, a ruptured aneurysm of the anterior communicating artery is indicated by a thick arrow, spasm of the anterior cerebral artery is indicated by two thin arrows. c) CT scan of the brain. Foci of ischemia as a result of widespread decompensated cerebral vasospasm are indicated by arrows.
- Internal hydrocephalus, caused by occlusion of the cerebrospinal fluid ducts, occurs in 25-27% of patients (Fig. 10).
Rice. 10. Massive basal SAH with intraventricular hemorrhage and the development of internal hydrocephalus.
7. Assessment of the severity of the patient’s condition
With all the diversity of the clinical picture of the course and complications of subarachnoid hemorrhage, only a few classifications of the severity of the patient’s condition are used in practice (Tables 1 and 2).
Table 1.
Assessment of level of consciousness using the Glasgow Coma Scale (recommended for ages 4 years and older).
| Points (3-15) | Opening your eyes | Voice contact | Physical activity |
| 6 | — | — | Executing commands |
| 5 | — | Orientation | Localization of pain (targeted) |
| 4 | Spontaneous | Confusion | Withdrawal of a limb (non-targeted) |
| 3 | To appeal | Inadequate (unintelligible words) | Limb flexion (decortication) |
| 2 | For pain* | Inappropriate (inarticulate sounds) | Limb extension (decerebration) |
| 1 | No | No | No# |
* when checking eye opening for pain, peripheral stimulation should be used (a painful grimace during central pain stimulation leads to squinting of the eyes) # in the absence of a motor response, it is necessary to exclude damage to the spinal cord.
Table 2.
Assessment of the severity of patients’ condition using the W. Hunt – R. Hess scale, 1968.
| Degree | Description |
| I | Asymptomatic, or mild headache and mild neck stiffness. |
| II | Moderate or severe headache, stiff neck, paresis of the cranial nerve (oculomotor). |
| III | Stupefaction, drowsiness, confusion. Moderate neurological deficit. |
| IV | Stupor, moderate or severe hemiparesis, early decerebrate rigidity. |
| V | Coma of varying depth, decerebrate rigidity. |
- in the presence of a serious general disease (hypertension, diabetes mellitus, severe atherosclerosis, chronic obstructive pulmonary disease) or severe vasospasm, the assessment of the severity of the patient’s condition is increased by one degree
- the original work did not take into account the age of the patients, the location of the aneurysms, or the time since the hemorrhage; The severity of the patients was assessed upon admission and before surgery.
The creation of such scales for assessing the severity of the condition is due to the need to standardize data on the study of examination results, conservative and surgical treatment of patients with NSAH, and prognosis of the outcome of the disease.
8. Surgical treatment of aneurysms
The choice of treatment tactics is determined by the location of the aneurysm, the presence or absence of its rupture, the time period from the moment of hemorrhage, the clinical condition of the patient, and the presence of complications.
Surgical treatment is indicated for all patients with aneurysms.
For patients with unruptured aneurysms, the timing of surgery is usually not of great importance, since the probability of aneurysm rupture is 1-2% per year. It is important that the operation is performed in a vascular center that has experience in such operations, minimal rates of mortality, disability, and complications.
Patients with ruptured aneurysms should strive to perform surgical treatment to exclude the aneurysm from the bloodstream as early as possible, since the risk of re-hemorrhage in the first two weeks from a ruptured aneurysm is 15-25%.
In the acute (up to 3 days) and acute period of NSAH (up to 14 days), due to rupture of an aneurysm, surgical treatment is performed for patients with an uncomplicated course of the disease (I-II, III degree of severity according to HH), a compensated condition of the patient, as well as for patients those at risk of recurrent bleeding from the aneurysm or the development of clinically significant vasospasm.
Also, according to vital indications, patients with IV-V severity of H-H are operated on, who have acute compression of the brain by a hematoma, severe occlusive hydrocephalus with dislocation of the brain stem, and extensive foci of ischemia. In such patients, surgery is considered as a stage of resuscitation.
In the delayed period of SAH (after 14 days), surgical treatment of patients is performed in case of a complicated course of the disease due to vasospasm with a severe condition (HH IV, V degree of severity according to HH) after improvement of the patient’s condition, as well as in the presence of an aneurysm of a hard-to-reach localization.
The presence of such serious complications in the patient as re-rupture of the aneurysm and the development of vasospasm significantly influence the choice of successful surgical tactics.
If the aneurysm ruptures again, in the case of a compensated condition of the patient, emergency surgery is indicated to exclude the aneurysm from the bloodstream. If it is impossible to carry it out due to the severity of the condition, stay in the neurointensive care unit and perform palliative operations: installation of intracranial pressure sensors, drainage of the ventricular system of the brain, installation of microdialysis and tissue oxygen tension sensors.
The tactics of surgical treatment of ruptured aneurysms in the acute period of hemorrhage with the development of cerebral vasospasm is one of the most difficult issues in aneurysm surgery.
The form of development of cerebral ischemia is decisive: with a compensated form of cerebral ischemia, patients can be operated on immediately after identifying an aneurysm; with a subcompensated form of cerebral ischemia, a wait-and-see approach is advisable in patients in accordance with the dynamics of ischemia; with decompensated cerebral ischemia, surgical intervention must be postponed and treated patients in neuroreanimation.
Currently, two main methods are used to exclude aneurysms from the bloodstream:
- open microsurgery
- endovascular intervention.
In some cases, in patients in serious condition, combined treatment is used - first, endovasal embolization of the aneurysm (to prevent re-hemorrhage), then, after the patient’s condition improves, open intervention.
An open microsurgical operation is performed under general anesthesia, with the obligatory use of an operating microscope and microsurgical equipment (Fig. 11).
a B C D E)
Rice. 11. Operating room equipment for microsurgical operations: a) operating table and rigid head fixation bracket (Mayfield-Kiss); b) operating microscope OPMI Neuro on the NC 4 platform; c) “Cellsaver” blood reinfusion apparatus and Karl Storz endoscopic stand; d) electrotrephine Aesculap; e) Stryker electric trepan.
Open surgery includes several stages:
- Trepanation of the skull
- Opening the dura mater
- Arachnoid dissection with isolation of the great vessels of the base of the brain and aneurysm
- Switching off the aneurysm from the bloodstream by clipping (Fig. 12)
- Closure of the surgical wound.
Rice. 12. Intraoperative photo. Pterional anterolateral subfrontal approach on the left. A ruptured aneurysm of the anterior communicating artery was clipped. The aneurysm dome and clip are indicated by arrows.
The rate of exclusion of aneurysms from the bloodstream during open operations reaches 98% (Fig. 13).
a) b)
Rice. 13. Clipping of an aneurysm of the left internal carotid artery: a) cerebral angiography before surgery, an aneurysm (arrow) of the supraclinoid section of the left internal carotid artery was detected; b) cerebral angiography after surgery, the aneurysm is not contrasted, the arrow indicates the clips on the neck of the aneurysm.
To control the radicality of aneurysm clipping and preserve blood flow along the functionally significant branches of the main arteries of the base of the brain, intraoperative Doppler sonography is used (Fig. 14).
a B C)
Rice. 14. Use of intraoperative Dopplerography when clipping an aneurysm of the left middle cerebral artery: a) intraoperative photograph: aneurysm (arrow) of the fork of the left middle cerebral artery with turbulent blood flow according to intraoperative Dopplerography; b) intraoperative photograph: the aneurysm of the bifurcation of the left middle cerebral artery is clipped, a microsensor (arrow) is installed on the M1 segment of the middle cerebral artery to record blood flow in it; c) intraoperative photograph: in the clipped aneurysm (arrow), blood flow is not recorded according to intraoperative Dopplerography; normal blood flow is preserved along the M2 segment of the left middle cerebral artery.
Endovasal intervention is performed when it is impossible to clip the aneurysm during open intervention, in case of aneurysms of difficult-to-reach localization (aneurysms of the vessels of the vertebrobasilar region, aneurysms of the internal carotid artery proximal to the ophthalmic segment), in elderly patients (over 75 years old). Endovasal surgery involves inserting a detachable Serbinenko balloon-catheter or electrically detachable Guglielmi platinum microspirals into the aneurysm cavity. Thanks to microcoils, thrombus formation occurs in the cavity of the aneurysm, as a result of which it is switched off from the bloodstream.
The rate of exclusion of aneurysms from the bloodstream during endovasal interventions is more than 85% (Fig. 15, 16).
Rice. 15. Diagram of aneurysm occlusion with microcoils.
A)
b)
Rice. 16. Embolization of basilar artery aneurysm. a) Cerebral angiogram, lateral projection, the arrow indicates the aneurysm of the basilar artery. b) Cerebral angiogram, lateral projection, the arrow indicates the aneurysm after embolization with microcoils.
9. Postoperative management
From the operating room, regardless of the severity of the condition, the patient is transferred to the neurointensive care unit. This department monitors the patient’s condition and prevents complications. If within 24 hours the patient’s condition is assessed as satisfactory or moderate, he is transferred to the neurosurgical department. If there is a deterioration in the condition, then an emergency CT scan of the brain, TDCG, is performed. Based on the results of these examinations, further tactics for patient management are determined.
10. Outcomes
Surgical activity for ruptured aneurysms in our clinic is 82–90%. For most patients, exclusion of aneurysms from the bloodstream is performed openly (92%), endovascularly – 8%. The overall postoperative mortality rate is 10-12%.
Clinical picture by age
In newborns, the course of an aneurysm without blood discharge is hidden. Symptoms in the presence of a pathological shunt:
- Tearfulness;
- Refusal to feed;
- Cry;
- Underweight;
- Frequent shallow breathing;
- Blue discoloration of the skin (the face may be red from crying);
- Fever (reflects the general reaction of the baby’s body to being unwell).
In children and adolescents, the disease, which is not accompanied by bleeding, is asymptomatic. In the presence of a shunt, the following manifestations are characteristic:
- Slow physical development;
- Dyspnea;
- Exercise intolerance;
- Complaints of stabbing pain in the heart, a feeling of irregularities and palpitations;
- Episodes of loss of consciousness;
- Insomnia;
- Cyanosis of lips, tip of nose, fingers.
Often, even with a shunt, children have no symptoms or complaints.
In adults, the clinical picture is determined by cardiopulmonary failure, which develops over many years, often in combination with other heart diseases. Symptoms:
- Dyspnea;
- Fast fatiguability;
- Chest pain;
- Exercise intolerance;
- Pain in the right hypochondrium;
- Swelling of the legs;
- Dilatation of superficial veins.
Adults are also characterized by an asymptomatic course, despite the presence of blood discharge, since the defect in the septum can be minor (2-3 mm).
Characteristics of the pathology
The main reason for the development of atrial aneurysm is a weakening of the heart wall, which has a clear localization and appears as a result of structural or functional disorders. In the first case, the layers of the septum are affected, followed by the death of healthy tissues or their replacement by foreign formations. Functional disorders are characterized by the inability of a local area of the myocardium to contract on a par with the entire heart muscle.
As a result of exposure to high pressure inside the hollow organ, the weakened area begins to bulge, eventually turning into an aneurysm. Most often, pathology is diagnosed on the walls of the ventricles, less often in the atria. Despite the long process of formation, its development can rapidly accelerate due to increased physical activity, during which the heart muscle has to pump a larger volume of blood.
The following types of aneurysms are distinguished:
- True. All layers of the vascular walls are subject to stretching. In most cases, the pathology does not manifest itself in any way until tissue rupture occurs. Advanced cases are fraught with the development of thrombosis, vascular dissection, embolism, and stroke.
- False. Develops after injury to the vascular walls. As a result, blood begins to leak through the thinned area, which accumulates in the septum as a pulsating hematoma. The main difference from a true aneurysm is that one layer of tissue is stretched. The greatest danger is posed by pathology that affects vital vessels.
- Delaminate. It is characterized by the leakage of blood into the space between the walls of the aorta, which under certain conditions leads to rupture of the outer septum. This type of aneurysm has a high risk of death if tissue ruptures.
Enter your pressure
130 /100
How is it formed?
Depending on the origin, congenital and acquired aneurysm of the septum between the atria is distinguished. A congenital anomaly is formed in childhood, and an acquired one develops as a result of exposure to provoking factors in an adult.
Congenital
The formation of an aneurysm in the fetus has certain characteristics. It can be combined with a violation of the fusion of the oval window (communication in the interatrial septum), which ensures the discharge of blood from the right circulation to the left. This is due to the fact that the lungs do not yet perform their function.
After the first inhalation, the right circle of blood circulation is turned on. During the first few days or weeks after birth, the diameter of the oval window decreases, fusion occurs (the duration of the period of fusion of the oval window is individual for each person), in the place of which a small depression remains. When exposed to various reasons, the healing process is disrupted, as a result of which the connective tissue has less strength, where a protrusion forms over time.
The exact cause of the development of an aneurysm remains unclear today.
There are several provoking factors, which include:
- hereditary predisposition;
- bad habits of parents;
- past infectious diseases during pregnancy (toxoplasmosis), exposure to adverse environmental factors (ionizing radiation, toxins).
Congenital aneurysm may have an isolated origin. In this case, the localization of the fossa ovale and the protrusion in the septum often do not coincide. The mechanism of development is usually associated with a primary hemodynamic disorder in the heart, which results in the formation of a protrusion in the area of high blood pressure.
Acquired
The mechanism of development of acquired septal aneurysm involves weakening of the septal tissue with subsequent formation of a bulge. It is a consequence of the influence of provoking factors (previous myocardial infarction, myocarditis, cardiomyopathy).
Development mechanism in the form of a table:
| Origin | Pathogenesis |
| Isolated congenital anomaly | Protrusion is formed due to hemodynamic disturbances in childhood |
| Anomaly combined with malformations of the oval window | Violation of the fusion of the oval window provokes the formation of a protrusion |
| Acquired aneurysm | Develops in adults due to weakening of the septal tissue, which provokes myocardial infarction, myocarditis, cardiomyopathy |
Since acquired aneurysm of the septum between the atria in most cases is the result of a myocardial infarction, it is divided into several types:
- Acute aneurysm - formation forms within 14 days after a heart attack. It is accompanied by a deterioration in the person’s condition with fever, arrhythmia (disturbance in the rhythm of contractions), and an increase in the number of leukocytes per unit volume of blood.
- Subacute aneurysm - the anomaly develops over 3-6 weeks, the protrusion is a consequence of a disruption in the formation of a connective tissue scar in the area of dead myocardiocytes. It is characterized by the gradual development of heart failure with shortness of breath, increased fatigue, swelling of soft tissues with a predominant localization on the legs.
- Chronic aneurysm - the formation of a protrusion in the septum between the atria occurs over a period of time exceeding 6 weeks and is accompanied by a gradual increase in the symptoms of congestive heart failure.
Division into types makes it possible to predict the further course of the pathology, as well as select the most adequate therapy.