Most often, heart disease is the result of inflammation, tumor or vascular damage. In many cases, when the cause of cardiac pathology is too vague or cannot be established, a diagnosis of cardiomyopathy is made. We are talking about a whole group of diseases that affect people regardless of age and gender, which was classified and sufficiently studied only in 2006. Effective methods for diagnosing and treating various types of cardiomyopathy have now been developed. The CBCP Center for Pathology of the Circulatory Organs also uses the latest technologies in this area.
What is cardiac cardiomyopathy?
This is a group of diseases affecting the myocardium with unclear causes. To make a diagnosis, it is necessary to ensure the absence of congenital heart defects, valves, blood vessels, arterial hypertension, pericarditis, etc. Depending on the type of damage to the heart muscle, dilated, hypertrophic, restrictive and arrhythmogenic forms of this disease are classified. The classification depends on the characteristics of the circulatory disorder in the heart. Using high-quality equipment, all types of cardiomyopathy are diagnosed at an early stage.
Cardiomyopathy: how to detect?
The key guarantee of cure for the patient is timely diagnosis. It allows you to detect pathology in time and receive effective treatment. With a routine examination, it is impossible to determine the presence of changes in the heart muscle. An increase in heart size is easily determined by echocardiography and electrocardiography. The attending cardiologist may additionally prescribe magnetic resonance imaging or radiocontrast ventriculography.
Request a call
Causes of primary and secondary cardiomyopathies
Depending on the causes, primary and secondary cardiomyopathy are distinguished. The causes of the primary disease are divided into 3 groups.
- Congenital ones develop even at the stage of formation of myocardial tissue in the embryo due to the bad habits of the mother, nutritional disorders, and stress.
- Acquired are the result of exposure to viruses, metabolic disorders, and toxic substances.
- Mixed ones combine one or more of the above reasons.
Primary cardiomyopathy is common in children. It can be not only congenital, but also acquired under the influence of reasons leading to disruption of the development of myocardial cells.
A secondary disease develops as a result of exposure to internal or external factors or other pathology. These include:
- accumulation of various pathological inclusions by cells;
- medications, in particular certain antitumor drugs;
- alcohol in large quantities and with prolonged use;
- metabolic disorders in the myocardium as a result of endocrine pathologies;
- unhealthy diet, obesity, diabetes, gastrointestinal diseases;
- long-term diets that cause a lack of vitamins and nutrients.
In Russia, mortality due to secondary cardiomyopathy is an extremely common phenomenon. And since the reasons themselves are very diverse, a high-quality and professional examination is necessary in each individual case.
Cardiomyopathy: symptoms
You may not notice the symptoms of this disease, since they are often not clearly expressed, and in some cases complications become noticeable. However, if cardiac cardiomyopathy has already manifested itself, it is difficult not to notice it.
- During intense physical activity, you feel short of breath and short of air.
- Long-term aching pain in the chest appears.
- Weakness and dizziness are noticeable.
- Constant swelling of the legs, sleep disorders, frequent fainting conditions.
These symptoms indicate disturbances in the contraction of the heart and problems with its blood supply. Contact your cardiologist immediately when they first appear!
Classification of cardiomyopathies and prognosis
As mentioned above, there are 2 main types of cardiomyopathy – primary and secondary. In turn, primary pathology is classified as follows:
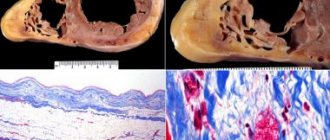
- With a dilated cavity, the hearts expand, systolic function and cardiac output are impaired, and heart failure develops. This type is also called “ischemic cardiomyopathy”.
- With hypertrophic , the wall of the ventricles thickens by 1.5 cm or more. Depending on the nature of the lesion, there are symmetrical and asymmetrical, obstructive and non-obstructive forms.
- Restrictive cardiomyopathy can be obliterative or diffuse. The form depends on the nature of the disturbances in the contractile function of the heart muscle, which lead to a lack of blood volume in the chambers of the organ.
- Arrhythmogenic dysplasia is an uncommon phenomenon and is caused by large deposits of fat that lead to arrhythmia. This pathology is also called Fontan's disease.
Secondary cardiomyopathy of the heart is classified depending on the causes that caused it:
- alcoholic;
- diabetic;
- thyrotoxic;
- stressful.
As is clear from the names themselves, the causes of these forms of the disease are alcohol, diabetes or obesity, thyroid pathologies or stress.
Attention to the heart muscle! How to detect cardiomyopathy?
The heart muscle is the main muscle of the human body and the basis of its vital activity. One of the diseases accompanied by disruption of its functioning is cardiomyopathy. We talked about this pathology, which occurs in both adults and children, with Marina Kazbekovna Tsogoeva, a cardiologist at the Expert Clinic Vladikavkaz.
— Marina Kazbekovna, tell us about cardiomyopathy. What is this pathology and how does it affect the functioning of the heart?
— Translated from Latin, cardiomyopathy means “disease of the heart muscle” (cardio - heart, myos - muscles, pathos - lesion/disease). This is a unifying name for completely different diseases, with different causes, sometimes different clinical manifestations, course and prognosis. What unites these diseases is only the localization of the lesion, that is, in each of them the myocardium is involved in the pathological process.
This pathology can affect the shape of the heart, its size, the thickness of the muscle wall, and the electrical transmission of signals through the cardiac chambers. As a result of these changes, the ability of the heart to pump blood is impaired, the relaxation of the heart (i.e., its diastolic function) is impaired, and cardiac arrhythmias occur.
— How does cardiomyopathy manifest?
— The most common symptoms are shortness of breath, increased fatigue, swelling, heart pain, interruptions in heart function, fainting, dizziness. Unfortunately, sometimes the only manifestation of cardiomyopathy can be sudden death as a result of cardiac arrhythmias.
Read materials on the topic:
Shortness of breath: when does the body ask for help? Swelling in the legs: why do they appear? Fainting and fainting are different. Let's figure out the reasons Spinning until you drop! Recognizing a heart enemy. What is arrhythmia?
— What types of cardiomyopathy are there and what are the reasons for their development?
— Cardiomyopathy is divided into several types. I'll tell you about the main ones. The most common among the adult population is dilated cardiomyopathy. In 30% of cases this is a hereditary disease. In addition, a significant role in its development is played by various infections (both viral and bacterial), toxins, hormonal disorders (against the background of thyroid pathology - for example, hyperthyroidism. What happens? The walls of the left ventricle of the heart stretch, become thinner and weaker. As a result the left ventricle no longer pumps blood so well, and heart failure develops, i.e., the heart’s ability to contract is significantly reduced.
The next type is hypertrophic cardiomyopathy. According to statistics, out of 500 examined in the general population, one patient with such a diagnosis is identified. For the development of this type of cardiomyopathy, only the hereditary factor matters, i.e. it is a genetically determined disease. Morphologically, the following happens. The ventricular muscle thickens (hypertrophies), making the chamber cavity (left ventricular cavity) significantly smaller. In addition to the occurrence of a mechanical obstacle to the outflow of blood from the cavity of the left ventricle, the hypertrophied myocardium becomes a source of dangerous cardiac arrhythmias, unfortunately, often fatal.
The reasons why restrictive cardiomyopathy occurs have not yet been precisely established. Recently, this cardiomyopathy is more often attributed to hereditary diseases. In restrictive cardiomyopathy, the heart muscle becomes stiff for a variety of reasons. Myocardial fibrosis is possible when connective tissue grows in the thickness of the myocardium. With the so-called storage diseases - amyloidosis, or with sarcoidosis of the heart, pathological protein is deposited or granulomas are formed in the thickness of the myocardium. As a result of such heterogeneity of the myocardium, its diastolic function (or, more simply put, relaxation) is impaired, and in the long term this leads to heart failure, which is difficult to compensate for with medication. Also, heterogeneous myocardium often becomes a source of life-threatening cardiac arrhythmias.
There are other types of cardiomyopathy, but they are less common.
— How to determine cardiomyopathy? What is its diagnosis?
— Firstly, the disease is often hereditary. And when diagnosing, we must definitely take this into account. As a rule, if cardiomyopathy is suspected, the doctor always focuses on family history, i.e., facts of early cardiac death of immediate relatives.
Secondly, symptoms. It is necessary to take into account manifestations of heart failure, cardiac arrhythmias, fainting, etc.
Thirdly, to detect cardiomyopathy, traditional methods for diagnosing heart diseases are used - echocardiography, electrocardiogram, Holter monitoring, magnetic resonance imaging. Molecular genetic analysis allows us to identify mutations in genes responsible for the development of the disease.
Read materials on the topic:
What will a heart ultrasound tell you? What does an electrocardiogram reveal? Holter (24-hour) ECG monitoring - complete instructions for the patient
— Marina Kazbekovna, how can you help the patient? What is the treatment for cardiomyopathy?
— Depending on its type and course, treatment is selected individually. There are, of course, general principles. We treat heart failure with medication, in accordance with national recommendations. If a patient with diagnosed cardiomyopathy experiences life-threatening cardiac arrhythmias or episodes of loss of consciousness, then radiofrequency ablation of the myocardial areas that are the source of these arrhythmias is considered. Or a cardioverter-defibrillator is implanted - a device that, having detected an arrhythmia, sends a series of electrical discharges to the heart, and thus restores the normal rhythm.
— What is the prognosis for cardiomyopathy?
- Again, everything is individual. The prognosis is determined by the nature and degree of progression of the disease. The patient’s adherence to treatment, a responsible attitude to taking medications, and compliance with all recommendations of the cardiologist are important. And, of course, optimal drug therapy, and, if necessary, timely surgical care can affect not only the quality, but also the life expectancy of a patient with cardiomyopathy.
You can make an appointment with a cardiologist here. ATTENTION: the service is not available in all cities
Interviewed by Marina Volovik
The editors recommend:
Fall asleep and not wake up. Why do tragedies happen in dreams? Coronary heart disease: diagnosis and treatment Serious question: what happens to the heart during an attack of angina? How to prevent myocardial infarction? Help your heart beat. How did the history of the pacemaker begin?
For reference:
Tsogoeva Marina Kazbekovna
Graduate of the medical faculty of the North Ossetian State Medical Academy in 2002.
From 2004 to 2006, she completed a residency in the specialty “Cardiology” at the Russian Medical Academy of Postgraduate Education (RMAPO), Moscow.
Until 2021, she worked as a cardiologist in the department of x-ray surgical methods of diagnosis and treatment at the North Caucasus Multidisciplinary Center, the city of Beslan (Republic of North Ossetia-Alania).
Currently, he is a cardiologist, functional diagnostics doctor at the Expert Clinic, Vladikavkaz.
Dilated cardiomyopathy (ischemic)
This type of cardiomyopathy is also called “congestive” or “ischemic” - due to a significant deterioration in blood circulation in the dilated chambers of the heart. A common cause (up to 20% of cases) of the development of pathology are:
- changes at the genetic level;
- various immune system failures;
- intoxication and infection.
In some cases, it is believed to be a familial disease. And it can appear by the age of 30.
The symptoms of dilated (ischemic) cardiomyopathy coincide with the general symptoms of heart failure. If you experience shortness of breath during exercise, you quickly get tired, notice swelling, pale skin, blue fingertips - you should immediately go for an ultrasound of the heart (echocardiography). This method is the most informative in this case. The examination also reveals atrial fibrillation.
With advanced disease, the prognosis is disappointing: mortality in ischemic cardiomyopathy reaches 70% in the first 5 years after the onset of pathology. Only timely intervention by cardiologists, a well-designed treatment program, and high-quality drug therapy (ACE inhibitors, beta blockers, etc.) can significantly prolong life.
In the future, your lifestyle will have to be adjusted. In particular, women with dilated ischemic cardiomyopathy are strictly not recommended to become pregnant, as this is one of the most common causes of a sharp deterioration in health.
Cardiomyopathy: treatment and drugs
At the first stage, a comprehensive diagnosis is carried out, the patient undergoes echocardiography and Holter ECG monitoring. After determining the type of disease and root causes, the cardiologist selects appropriate therapy and prescribes a course of treatment. Tactics will depend on many factors, including the anatomical features of the heart muscle.
How is cardiomyopathy treated:
- limiting and developing a personal plan for physical activity;
- following the regimen and lifestyle prescribed by the doctor;
- drug therapy and taking medications prescribed by a cardiologist;
- if necessary, surgical methods of intervention.
For the treatment of cardiomyopathy in our country, ACE inhibitors, diuretics, beta blockers, digoxin, anticoagulants and antiarrhythmic drugs are traditionally used.
Hypertrophic cardiomyopathy
This type of pathology is manifested by enlargement and hypertrophy of cardiac tissue in the left ventricle (enlargement of the right ventricle can also occur, but is extremely rare).
- In this case, a clear asymmetry develops in the heart: for example, the ventricular cavity is significantly reduced, and the left atrium expands.
- Diastolic filling of the ventricle occurs with disturbances and diastolic function is insufficient.
- Part of the ventricle, as well as the interventricular septum, may hypertrophy.
- Due to an increase in diastolic pressure in the pulmonary veins, gas exchange in the lungs is disrupted.
The disease also very often manifests itself in 30-year-old patients. The later stages are characterized by shortness of breath (in 90% of cases), arrhythmia and angina pectoris, and the pressure at the outlet of the left ventricle can rise to 185 mm Hg. Therefore, the main diagnostic methods for this type of cardiomyopathy are various types of ECG and ultrasound of the heart.
Characteristic symptoms include prolonged chest pain, which is typical of angina. During physical exertion, the patient may faint. Blood circulation in the brain also suffers, which is manifested by brief deterioration in attention, memory, and speech.
The prognosis of cardiomyopathy is quite negative if the stage of the disease no longer allows for positive changes in the functioning of the heart. If the diagnosis is made on time and treatment is started in the early stages, then through drug therapy (beta-blockers, diuretics, etc.) it is possible to prolong the patient’s life for a sufficiently long period.
Disability due to cardiomyopathy. Disability due to cardiomyopathy
Hello, Siberian
.
Quote
How serious is this?
Since our site is called “Medical and Social Expertise”, the following should be said regarding the prospects for a possible determination of disability.
In accordance with current legislation:
“A citizen is referred for a medical and social examination by an organization that provides medical and preventive care in accordance with clause 16 of the “Rules for recognizing a person as disabled” AFTER
the necessary diagnostic, therapeutic and rehabilitation measures have been carried out
. incl. high-tech medical care, in the presence of data confirming persistent impairment of body functions caused by diseases, consequences of injuries or defects.”
Simply put - FIRST - the patient must be treated for a certain period (for each pathology this period is different), and only AFTER the treatment - based on its results, the question of the presence (or absence) of signs of disability is decided.
Quote
The diagnosis was made a week ago. first.
Considering the short period of time from the start of treatment for a newly diagnosed pathology, it is still too early (premature) to talk about the presence (or absence) of signs of disability in the patient.
Quote
What should she do first?
Carefully follow the recommendations of your treating physicians.
In the case of pathology of the cardiovascular system, the decisive criterion for establishing a specific disability group is the degree of NC (circulatory insufficiency), which is assessed ONLY after treatment for the identified pathology (i.e., in situations where NC is PERSISTENT - untreatable).
Typically, the ratios of NK degrees and disability groups are as follows:
With NK 0, NK 0-1 and NK 1st. - disability is usually not established.
With NC 2Ast. - usually - 3rd disability group.
With NK 2Bst. - usually - 2nd disability group.
Restrictive cardiomyopathy
This species is quite rare in medical practice and has therefore been little studied. In this case, the walls of the myocardium become too rigid, do not stretch and lose the ability to enter the relaxation stage. In this case, there is no thickening of the myocardial walls or enlargement of the ventricle, as with other types of cardiac cardiomyopathy.
The elasticity of the heart muscles decreases. The body begins to retain excess fluid. As a result, oxygen, along with the blood, flows worse and in insufficient quantities into the left ventricle. Pathology leads to disruption of general blood circulation and poor blood supply to various organs.
It occurs in young people and children, often in combination with other diseases caused by metabolic disorders. Diagnosis is difficult, since the pathology manifests itself already at the stage when heart failure develops with its typical symptoms. It is for this reason that treatment does not always begin on time, so the prognosis in some cases may not be too optimistic.
For diagnosis, the most valuable information is obtained during cardiac ultrasound (echocardiography). Laboratory tests may reveal eosinophils (white cells) and deposits of amyloid (a complex of protein and carbohydrate) in the internal organs.
What factors cause the primary form?
Primary cardiomyopathy can occur due to a viral infection, an autoimmune disorder, or idiopathic myocardial fibrosis. The cause may also be certain types of changes in the human genome. The influence of a genetic factor on the appearance of cardiac cardiomyopathy cannot be determined due to the fact that a huge number of proteins are involved in the metabolism of cardiomyocytes. In this case, pathology develops when changes appear in just one or several of them.
Symptoms characteristic of cardiomyopathy are caused by viral causes of the development of myopathies. This theory can be confirmed by antibodies that are detected in relation to the penetration of viruses . For example, the immune system reacts to cytomegalovirus, the causative agent of hepatitis C, as well as the Coxsackie virus. All these pathogens are capable of influencing DNA, with the subsequent development of pathology of the heart muscle.
The theory of the development of cardiomyopathy according to clinical recommendations as a result of the appearance of autoimmune changes in the body is not without foundation. The development mechanism is associated with the acceptance of myocardial cells as foreign by the human immune system. In this case, the body produces antibodies directed against cardiomyocytes. This opposite effect of immunity can be caused by viruses, bacteria, and various pathologies.
The restrictive form is characterized by myocardial rigidity with limited filling of the heart chambers with blood. A decrease in blood flow volumes leads to the development of diastolic dysfunction, against which heart failure appears with the manifestation of acute restrictive cardiomyopathy.
The cause may be idiopathic myocardial fibrosis, cardiosclerosis , in which cardiomyopathy appears, the diagnosis shows the replacement of the characteristic muscle fibers of the heart with connective tissue. They lose elasticity, are unable to contract, and disrupt the heart rhythm. The cause may be inflammatory processes in the myocardium or a previous heart attack. secondary cardiomyopathy occurs .
Arrhythmogenic cardiomyopathy
This cardiomyopathy is also called right ventricular - due to the specific location of the pathological changes. It develops mainly against the background of bradycardia, tachycardia or other types of chronic arrhythmia. The disease is quite rare, its frequency is 1:5000 of all cases of cardiac cardiomyopathy, and the causes are not completely clear to medicine.
The pathology is that the myocardium of the right ventricle is gradually replaced by fat or connective tissue. In rare cases, the left ventricle may also be partially affected, while the interventricular septum remains healthy.
This type of pathology is also often familial in nature, can be inherited by close relatives and manifests itself already in adolescence. There is a classification of arrhythmogenic cardiomyopathy:
- disease in its pure form;
- Naxos disease, accompanied by malignant ventricular arrhythmia;
- Venetian form with involvement of the left ventricle and manifestation in childhood;
- Pokkuri disease with ECG changes;
- benign right ventricular extrasystoles;
- Uhl's anomaly with a complete absence of muscle fibers in the myocardium;
- biventricular dysplasia affecting both ventricles;
- dysplasia with complications in the form of myocarditis.
Most patients, if treatment is started in a timely manner, will undergo lifelong monitoring by a cardiologist with drug therapy.
Secondary cardiomyopathies of the heart
This group includes pathologies whose causes lie in physical and chemical disorders in the body that provoke changes in the heart muscle.
- Alcoholic cardiomyopathy is a consequence of the effect on the myocardium of ethanol, which forms the basis of alcoholic beverages. As a result, adipose tissue appears in the myocardium.
- Thyrotoxic is caused by dysfunction of the endocrine system, lack of treatment for thyrotoxicosis. One of the common manifestations is dyshormonal cardiomyopathy during puberty or during hormonal therapy.
- Toxic is another type of secondary cardiomyopathy associated with the effects of various toxic substances on the heart tissue: lithium, cobalt, etc. They cause inflammation and microinfarctions.
- Stress is accompanied by a decrease in myocardial contractions and weakness due to emotional, mental influences, and shocks.
- Diabetic appears when diagnosed with diabetes mellitus and leads to biochemical changes in the myocardium and the accumulation of various polysaccharides.
The prognosis for each type of secondary cardiomyopathy depends on the success of treatment not only of the pathology itself, but also of the diseases that caused it: diabetes mellitus, thyrotoxicosis, alcohol addiction, etc. These are extremely difficult cases, but with a professional approach, the patient’s life expectancy can be maximized.
Types of cardiomyopathy
Modern cardiology divides myocardial pathologies, united under the concept of cardiomyopathies, into different types.
Main types of disease:
- Disturbances of the heart chambers and their expansion are referred to as dilated cardiomyopathy. It is the most common and is very difficult. Gradually the heart begins to fail to cope with its function.
- Pathological enlargement of the heart is called hypertrophic cardiomyopathy. But it often causes the death of young people.
- The disease associated with the restriction of blood flow into the aorta from the left ventricle is classified as an obstructive type of cardiomyopathy.
- Postpartum peripartum cardiomyopathy, characteristic of women, etc.
Complications
- The main ones are heart failure and arrhythmias in their obvious clinical manifestations.
- When the walls of the ventricle expand, the heart valves stop working normally.
- Due to the large accumulation of fluid in the tissues and internal organs (lungs), edema appears.
- Embolism (formation of blood clots and blood clots) is an extremely dangerous complication that leads to heart attack and stroke.
- Sudden cardiac arrest is the most complex consequence of cardiomyopathy, which, in the absence of timely resuscitation, is fatal.
In order for the forecast to be as optimistic as possible, monitor your lifestyle and diet. And to avoid negative consequences, visit a qualified cardiologist as often as possible and undergo diagnostics using modern equipment.