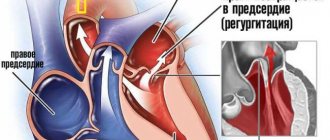
Heart valve prolapse is a disease accompanied by a malfunction of the valve located between the ventricle and the left atrium and is a common and relatively harmless anomaly, during which an unnatural protrusion of the valve leaflets appears when the heart contracts.
A heart valve is a movable valve consisting of individual elements that blocks the openings for blood circulation from one part of the heart to another. The valves' job is to control blood flow. There are four valves in the heart - mitral, tricuspid, aortic and pulmonary, which allow blood to flow in one direction and prevent it from returning back. When the heart muscle contracts, pressure is created, and blood is ejected from the heart, and the valves that regulate the movement of blood in this direction at the time of muscle contraction open. After the muscle contracts, the pressure in the heart drops, the valve closes, and blood cannot return to the heart. Among other types of prolapse, the most common is mitral valve prolapse, which is caused by congenital weakness of the connective tissue that makes up the heart valves.
Mitral valve prolapse
Mitral valve prolapse (MVP) is the most common heart problem.
According to statistics, every fifth person has this defect. Most of them (30–40%) do not even suspect the presence of pathology, but in some cases it causes complications. Literally from Latin “prolapse” is translated as “loss”. Essentially, this is the sagging of one or both valve leaflets into the atrium cavity. It can occur at any age, but mitral valve prolapse is most often diagnosed in children.
Reasons for development
With this pathology, a small part of the blood returns to the atrium, that is, it does not enter the aorta. This condition is often asymptomatic and is usually diagnosed “accidentally” during a routine preventive examination or in connection with examinations for other problems of the cardiovascular system.
In the same way, the causes of prolapse of the anterior valve leaflet are not known for certain; some experts argue that the pathology is associated with hereditary diseases of the connective tissue - for example, it could be osteogenesis imperfecta or Marfan syndrome.
Causes and degrees of mitral valve prolapse
Pathology can be primary and secondary. In the first case, the cause is connective tissue dysplasia. It causes a change in the structure and length of the chords by which the valve flaps are attached to the muscles, or contributes to the appearance of additional chords.
Secondary prolapse accompanies or complicates other pathologies. Possible reasons:
- congenital heart defects;
- endocrine disorders;
- rheumatic diseases;
- connective tissue diseases;
- genetic syndromes.
Risk factors are valvular-ventricular disproportion, infective endocarditis, insufficient blood supply to the papillary muscles, hypertrophic cardiomyopathy, inflammatory damage to the valvular structures of the heart, myocarditis, hypertrophy of the ventricular wall, pericarditis, coronary heart disease, chest trauma, etc.
The pathology is divided into 3 degrees depending on how much the valve leaflets protrude:
- 3–5 mm – I degree;
- 6–9 mm – II degree;
- ≥ 10 mm – III degree.
The course of the disease is usually benign. In most patients, the disorder does not progress throughout their lives. There are known cases of a decrease in the severity of pathology with age. Complications are rare, but they are possible.
Publications in the media
Mitral valve prolapse (MVP) is a pathological sagging (bending) of one or both mitral valve leaflets into the left atrium during left ventricular systole. Statistical data. MVP is found in 3–8% of people in the general population (apparently, the data is overestimated). Manifestations of MVP are first recorded at the age of 10–16 years; after 10 years, girls are observed 2 times more often.
Etiology. MVP can be primary or secondary • Primary MVP •• A disease inherited in an autosomal dominant manner with myxomatous deformation of the mitral valve leaflets •• MVP is also observed in patients with Marfan syndrome and other congenital connective tissue diseases, such as Ehlers-Danlos syndrome, elastic pseudoxanthoma, osteogenesis imperfecta •• In the occurrence of MVP, exposure to toxic agents on the fetus on the 35–42nd day of pregnancy may also be important • Secondary MVP can occur with: •• IHD (ischemia of the papillary muscles) •• rheumatism (post-infectious sclerotic changes) • • hypertrophic cardiomyopathy (disproportionally small left ventricle, change in the location of the papillary muscles).
Pathogenesis • Primary MVP •• Myxomatous degeneration of collagen leads to excessive accumulation of mucopolysaccharides in the middle spongy part of the mitral valve leaflets and its hyperplasia, which causes the appearance of break areas in the fibrous part of the valve. Local replacement of the elastic fibrous tissue of the valve leaflet with a weak and inelastic spongy structure leads to the fact that during systole, under the influence of blood pressure from the left ventricle, the leaflet bulges towards the left atrium (prolapses) •• In the occurrence of primary MVP in Marfan syndrome, it is also important dilatation of the annulus fibrosus of the mitral valve - it does not decrease by 30% in systole, as is normal, which leads to protrusion of one or both leaflets into the cavity of the left atrium • Secondary MVP occurs as a result of thinning and elongation of the tendon threads or their separation or dilatation of the fibrous ring. Lengthening of the tendon threads, separation of part of them lead to the fact that the leaflet is not held in place and begins to prolapse into the left atrium • If the mitral valve leaflet is excessively bowed, mitral regurgitation may occur with dilatation of the left atrium and left ventricle. It should be noted that MVP can be combined with prolapse of other valves: tricuspid valve prolapse in 40% of cases, pulmonary valve prolapse in 10%, aortic valve prolapse in 2%. In this case, in addition to mitral valve insufficiency, manifestations of insufficiency of the corresponding valve will occur. There is often a combination of MVP with other congenital anomalies of the heart - ASD, additional conduction pathways (usually left-sided).
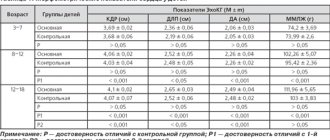
Clinical manifestations • Complaints •• In most cases, MVP is asymptomatic and is detected by chance during a preventive examination •• With more severe prolapse, patients complain of palpitations (ventricular extrasystole, paroxysmal supraventricular tachycardia, less often ventricular tachycardia) •• A common complaint is pain in the chest. It can be either atypical or typical anginal due to spasm of the coronary arteries or ischemia as a result of tension of the papillary muscles •• Shortness of breath during physical exertion, fatigue are also noted by patients with MVP •• Extremely rare manifestations are visual impairment as a result of thromboembolism of the retinal vessels, and also transient ischemic attacks as a result of cerebral thromboembolism. In the occurrence of embolic complications, importance is attached to the separation of fibrin threads located on the atrial side of the mitral valve •• Often the above-described complaints are accompanied by psycho-emotional lability • Upon examination, concomitant congenital abnormalities of the chest shape can be identified - kyphoscoliosis, funnel-shaped chest, pathologically straightened back, reduced anteroposterior chest size cells or signs of Marfan syndrome • Auscultation of the heart (a “silent” form of MVP is possible) •• The main auscultatory sign of MVP is a short mid-systolic high-frequency click (pathognomonic). It appears as a result of sagging of the mitral valve leaflets in systole into the cavity of the left atrium and their sharp tension •• The systolic click may be followed by a mid- or high-frequency late systolic murmur, better heard at the apex of the heart •• To clarify the manifestations of MVP, dynamic auscultation of the heart is used •• • Changes in left ventricular end-diastolic volume result in changes in the timing of the click and murmur. All maneuvers that contribute to a decrease in end-diastolic volume, an increase in heart rate, or a decrease in resistance to ejection from the left ventricle lead to MVP appearing earlier (the click noise approaches the first sound). All maneuvers that increase blood volume in the left ventricle, reduce myocardial contractility or increase afterload increase the time from the beginning of systole to the appearance of a click noise (moves back to the second sound) ••• In the supine position, the click occurs later, the noise is short ••• In the position standing, the click occurs earlier, and the noise is longer ••• In the squatting position, the click occurs later, and the noise is shorter (may even disappear). Instrumental data • Usually no changes are detected on the ECG in patients with MVP. Of the detected deviations, depression of the ST segment or negative T waves in leads III, aVF are most often noted. These changes may reflect ischemia of the inferior wall of the left ventricle as a result of tension in the posterior papillary muscle due to leaflet prolapse. In patients with ECG changes, cardiac arrhythmias also occur. Some patients experience prolongation of the QT interval. Recording an ECG after taking beta-blockers increases the specificity of this method • EchoCG •• In one-dimensional mode, the “hammock” symptom is detected - sagging of one or both leaflets in systole by more than 3 mm •• In two-dimensional mode, sagging of the mitral valve leaflets into the cavity of the left atrium in systole is detected left ventricle, thickening of the leaflets more than 5 mm in diastole, lengthening of the tendon filaments, lengthening of the leaflets, dilatation of the fibrous ring •• There are three degrees of MVP, determined in a four-chamber section ••• I degree (minor) - sagging of the leaflets into the cavity of the left atrium up to 5 mm ••• II degree (moderate) - sagging of the leaflets into the cavity of the left atrium 5-10 mm ••• III degree (severe) - sagging of the leaflets into the cavity of the left atrium more than 10 mm •• Doppler examination can reveal a regurgitation jet in the left atrium. With severe MVP, dilatation of the left atrium and left ventricle occurs, detected in one- and two-dimensional modes. It should be remembered that in the presence of typical auscultatory signs of MVP, its EchoCG signs may be absent in 10% of patients. When conducting the study, you should remember about other congenital heart defects (in particular, ASD). Differential diagnosis • Mitral valve insufficiency of rheumatic origin • Isolated aneurysm of the interatrial septum • Isolated tricuspid valve prolapse • VSD.
TREATMENT Management tactics • Treatment of the underlying disease in secondary MVP • Risk groups for the development of complications (patients with severe systolic murmur, thickened prolapsed mitral valve leaflets, left ventricular hypertrophy, rhythm disturbances, fainting) undergo regular ECG, echocardiography • Prevention of endocarditis is indicated for persons with severe systolic murmur. Treatment of various options • For asymptomatic MVP without signs of mitral valve insufficiency, there is no need for treatment •• The patient should be given recommendations for normalizing lifestyle, optimizing physical activity (a decrease in the tone of the sympathetic nervous system can lead to a decrease in valvular dysfunction) •• EchoCG is recommended -control once every 1–2 years •• It is necessary to avoid drinking strong tea, coffee, alcohol, as well as smoking • For severe MVP •• If there are symptoms of MVP such as tachycardia, palpitations, chest pain, is prescribed -adrenergic blockers in small doses (for example, propranolol at a dose of 30–60 mg/day) •• In case of dilatation of the left atrium and left ventricle, prolongation of the QT interval, a history of fainting, dilatation of the initial part of the aorta, physical activity is prohibited •• Prevention is recommended infective endocarditis using amoxicillin •• For symptoms of embolization, acetylsalicylic acid is prescribed at a dose of 80–325 mg/day •• With significant changes in hemodynamics, increasing symptoms of mitral valve insufficiency, mitral valve replacement or annuloplasty is performed.
Prognosis and complications . Typically, MVP is benign. Complications of MVP most often occur in patients with systolic murmur, thickened, elongated mitral leaflets, or enlarged left ventricular cavity or left atrium. Complications include: • separation of tendon threads • severe mitral valve insufficiency (0.06%) • fibrin deposition on the mitral valve leaflets • cardiac arrhythmias • cerebrovascular pathology (0.02%) • infectious myocarditis (0.02%) • sudden cardiac arrest death (0.06% of cases with severe mitral valve insufficiency). Synonyms • Systolic click-murmur syndrome • Barlow's syndrome • Inflated mitral valve syndrome. Reduction. MVP - mitral valve prolapse.
ICD-10 • I34.1 Prolapse [prolapse] of the mitral valve
Signs of mitral valve prolapse
Clinical manifestations depend on the degree of connective tissue dysplasia. The main symptom is heart rhythm disturbances - acceleration, tremors, freezing, interruptions. During physical activity, stress, and drinking coffee, extrasystole, a feeling of lack of air, shortness of breath, and tachycardia often occur. Some patients experience shortness of breath even with little activity.
Other possible signs:
- chest pain;
- dyspnea;
- hyperventilation syndrome;
- vegetative crisis;
- increased sweating;
- anxiety;
- increased fatigue;
- headache;
- dizziness;
- feeling of a lump in the throat;
- decreased performance;
- irritability;
- mood swings;
- depression;
- presyncope and fainting;
- slight increase in body temperature.
Diagnostics
The main diagnostic method is conventional auscultation of the heart (listening). When prolapse occurs, the doctor hears specific noises and clicks.
An ECG is not advisable because it does not show any abnormalities. The key test is echocardiography. If necessary, angiocardiography, left-sided ventriculography, and radionuclide testing are additionally performed.
Differential diagnosis is carried out with aneurysm of the interatrial septum, mitral valve insufficiency, acquired heart defects.
Treatment methods
Prolapse of both the anterior and posterior leaflets of the mitral valve is eliminated surgically. The conservative way is ineffective.
However, the use of medications is indicated at the stage of planning the operation and after the intervention to maintain the condition of the cardiac structures in a working position.
The main method of treatment is mitral valve replacement. Plastic surgery does not make much sense and gives a worse prognosis even with identical or even greater complexity of the intervention.
At the same time, there is no point in immediately going under the knife. And not a single doctor will prescribe radical therapy at first glance at a person. At an early stage, the process may spontaneously slow down. Surgery is indicated for stable progression within 3-6 months.
What medications are used:
- Cardioprotectors. To improve metabolic processes in the heart muscle. Mildronate will do.
- Antiarrhythmics as needed. Amiodarone. But in a minimal dosage, for a short course.
- Medicines to lower blood pressure. ACE inhibitors, beta blockers, centrally acting agents, calcium antagonists. With great caution and strictly according to indications.
Lifestyle changes are mandatory. No stress, smoking, alcohol, minimum physical activity.
A new diet is also required, but it is not necessary to prescribe and follow a strict diet. If possible, you should contact a specialized nutritionist. It is independently recommended to adhere to treatment table No. 10.
How to treat mitral valve prolapse?
Many patients do not require specific therapy. For mitral valve prolapse, medications are required for patients who experience heart palpitations and heart pain.
For moderate cases of the disease, sedative herbal remedies based on St. John's wort, valerian, hawthorn, valerian, and motherwort are prescribed.
In recent years, magnesium preparations have been increasingly used. Studies have established a beneficial effect on patients with MVP of the drug Magnerot, used for 6 months at a dose of 1000 mg three times a day.
For frequent extrasystoles and prolongation of the QT interval, the use of beta-blockers (Anaprilin or Sotalol) is indicated.
Severe mitral regurgitation requires surgical treatment.
Surgery
Surgery is prescribed in severe cases, when the disease is pronounced and reduces the quality of life, for example, tissue fibrosis develops against the background of MVP, and calcified areas appear.
The goal of the procedure is to replace the affected valve with a prosthesis that will take over the main functions. Mitral valve repair can also be performed. The operation is quite complex and is performed by a cardiac surgeon. It is preceded by a long preparatory stage, during which the patient undergoes numerous examinations, chooses a method for carrying out the procedure, and selects a prosthesis with a suitable throughput. During the procedure, the patient is connected to the artificial circulation system.
A feature of surgical intervention is a very long rehabilitation stage. It takes from 2 to 5 years. Patients with artificial limbs should regularly take anti-blood clot medications.
Among the disadvantages of surgical intervention, the limited service life of the prosthesis should be noted. After a certain period of time it will need to be replaced.
Frequently asked questions about mitral valve prolapse
What is the mitral valve?
This is a bicuspid valve that connects the left ventricle of the heart to the left atrium. It has an oval shape and consists of connective tissue cusps, which during systole prevent the reverse flow (regurgitation) of blood into the left atrium.
What is the danger of mitral valve prolapse?
Serious complications include severe arrhythmia and bacterial endocarditis.
Can mitral valve prolapse be cured?
It is impossible to cure MVP with drug therapy. A necessary condition is a change in lifestyle, eliminating stress and excessive stress.