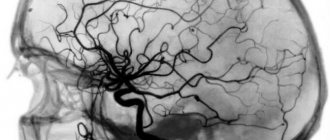
In a healthy body, blood circulates freely. The arterial and venous systems, which are found throughout the body, including the central nervous system (CNS), are responsible for this. To ensure proper functioning of the central nervous system, both sufficient arterial inflow, which ensures the delivery of oxygen and nutrients necessary for the proper functioning of the brain, and venous outflow, which removes metabolic products from the central nervous system, are important. Metabolism in the nervous system is much faster than in most tissues of the body. Therefore, ensuring proper and sufficient blood flow is important for health.
Signs of violation
When venous outflow is impaired in children, the following signs appear:
- worsening sleep;
- anxiety;
- decreased attention;
- delayed psycho-speech development;
- pronounced venous network on the head
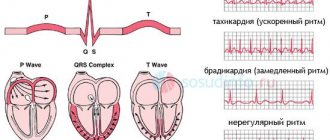
A child with such disorders gets tired quickly and cannot concentrate. Attention is scattered, activity drops. In an adult, disturbances in venous outflow also have a negative impact on sleep, well-being, and activity.
As a child with such problems ages, other symptoms may appear: lack of coordination, emotional instability, convulsions, tremors of the limbs, dizziness, darkening of the eyes, noise and ringing in the ears.
Causes of the disease
The causes of impaired venous outflow are different. The disease can be associated with injuries, including birth injuries, which is the most common cause in children with impaired vascular tone, muscle disorders, for example, congenital or installation torticollis. Problems are noted with inflammation of the veins, the formation of hernias, and osteochondrosis of the vertebral region. Such disorders in children can be caused by prolonged stay in an uncomfortable position, physical inactivity, overexertion, colds accompanied by cough, uncomfortable clothes with tight collars.
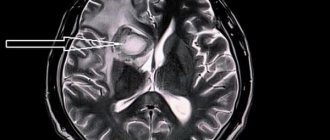
To accurately determine the cause of the disorders, it is worth contacting a neurologist and undergoing examinations as prescribed by the doctor. To identify the disease, it is enough to do an ultrasound of the vessels of the head and neck. The procedure allows an accurate diagnosis to be made at any stage of the disorder. In total, there are three stages of disease development: early (latent), stagnant and chronic. At the third stage, the child develops severe congestion leading to encephalopathy (disturbances in the structure of the brain matter).
Encephalopathy is treatable, but it is advisable to identify the disease at earlier stages. In this case, the likelihood of more severe violations is minimal.
Physiology of venous outflow
During the normal functioning of the blood supply system, the process of blood outflow from the lower extremities is ensured by three interconnected systems that clearly interact with each other. This system includes superficial and deep veins, as well as communicating veins that connect them to each other.
The outflow of 85-90% of venous blood passes through the deep venous system. About 10-15% of the total blood flow is carried out by the superficial veins. Blood is collected from suprafascial tissues by the saphenous veins, and then through a large number of perforating veins it goes into the deep lines. Pushing forces:
Residual pressure gradient. A positive pressure of 12–15 mm Hg is transmitted to the venous bed through a network of capillaries. Art. Venous vessels have little resistance, so at this pressure at rest the necessary blood flow to the heart will be ensured even without any additional factors.
Passive component of emptying. If transmural intravascular, extravascular) pressure begins to change, this leads to the fact that the capacity of the venous bed also changes. This occurs because the venous wall is elastic and resilient. If the muscle wall is in a relaxed state (for example, if a person is in a horizontal position, then the pressure in the venous system is 8-10 mm Hg), then the vein in cross section has an ellipsoidal shape with folded intima. Because of this, the capacity of the veins decreases several times, and venous return increases.
Venous tone , which is the active component. There is a distinction between intrinsic tone, which arises due to spontaneous depolarization of smooth muscle cells, and tone, which arises under the influence of sympathetic influences.
Sympathetic tone. If the sympathetic chain is stimulated, then as a result the veins begin to actively contract, which leads to an increase in the tone of their walls. In addition, observations have shown that veins are more sensitive to irritation of sympathetic nerves than arteries. The constrictor nerve fibers of the veins are activated by baroreceptors located in the kinocaroid zone, as well as by the reflexogenic zones of the heart and lungs. Here, a special role must be played by receptors located in the right atrium, through which the feedback necessary to ensure adequate venous return occurs. The extent to which constrictor influences are exerted on the venous wall largely depends on its initial distension. When a person is in an upright position, venous intramural pressure makes them round in cross section, so during sympathetic impulses the lumen of the veins can narrow and blood can move towards the heart. If the vessel wall is in a relaxed state and has the shape of an ellipse in cross section, then sympathetic impulses have virtually no effect on the capacitive characteristics of the veins. In addition, because of them, the capacity of the veins can increase due to the fact that the configuration of the vessel changes. The question of how passive and active changes in the capacity of the venous bed influence blood flow to the heart is quite complex. It is believed that constant central venous pressure is maintained due to the initial inclusion of a passive mechanism for changing the process of blood filling of the veins, and then a change in blood volume, which occurs due to the fact that the smooth muscles of the venous wall begin to actively contract. In the splanchnic circulation department, a particularly important role belongs to the passive regulation of vein capacity. This is explained by the fact that the vessels located in this area, in their relation to the hydrostatic factor, are in a “privileged” position and are less filled with blood. That is why they have less sensitivity to nervous constrictor effects. It must also be remembered that the parenchymal vascular bed, being at rest, includes about 20% of the total blood volume, and also has a significant impact on the regulation of the central blood volume. It was previously believed that active sympathetic vasoconstriction affected only the superficial veins located in the extremities and did not extend to the deep veins. More recent studies have shown that the deep veins of the extremities and, in particular, the muscular veins have adrenergic innervation. The capacitive vessels of the muscles have the ability to actively contract, although this process is much worse than that of the superficial veins. Deposition of blood in the venous bed of the lower extremities, which can stretch, is not compensated by nervous influences. Meanwhile, if the neurogenic tone of the veins is disturbed, it affects the course of hemorrhagic shock, operational and orthostatic collapse, hypertension, congestive heart failure, etc.
Systole-diastolic movement of adjacent arteries.
Activity of the muscular-venous pump. When a person is in an upright position, the skeletal muscles experience muscle tension. In this case, intramuscular pressure increases by 50-60 mm. Hg This pressure limits the degree of stretching of the veins and prevents orthostatic disorders.
The muscle pump of the lower extremities includes a system of functional units that operate both sequentially and in parallel. Each of these units includes separate myofascial formations, a part of the deep vein that has valves and is connected through the communicating vein to the corresponding segment of the superficial vein. When the muscles are in a relaxed state, the valves are open and do not interfere with the formation of a hydrostatic column between the heart and foot. In this case, both in the deep and superficial veins of the lower extremities, the pressure at the same level is the same. Due to muscle contraction, mechanical compression occurs, as a result of which intramural pressure increases in both deep and superficial veins, and due to the valves, centripetal movement of blood occurs. When the muscles relax, the level of intramural pressure in the veins decreases. At a certain stage of relaxation, the pressure level in the deep vein decreases more than in the superficial vein, which is why blood begins to flow into this part of the deep vein not only from the segment that is located slightly lower, but also from the superficial veins using the communicating veins.
The muscular-venous pump, according to its location, is divided into the following types: foot pump, lower leg pump, thigh pump, abdominal wall pump. When a person walks, the muscles of the lower leg, which are covered with dense fascia, take on the main work. When the calf muscle contracts, the average pressure in it reaches 70-100 mmHg. in case of maximum tension of the calf muscle, the pressure can reach 200 mmHg. The thigh muscles do not have a dense fascial covering, so during contraction, the pressure in them increases to 20-30 mm Hg. The peculiarity of the plantar pump is as follows: the outflow of blood occurs not only due to the fact that the muscles of the foot, which have a relatively small mass, contract, but due to the influence of the entire body weight.
The calf musculovenous pump is designed to maintain the desired level of venous return to the heart. This can be shown in the following example. During centrifuge testing, the sudden increase in gravity from the head to the feet may reduce visual acuity or cause darkening or even loss of consciousness. These phenomena can be avoided if the subject works vigorously with his legs, for example, moving the weight of the body from one leg to the other without lifting them from the support. Even a small amount of leg work leads to a restoration of cardiac output and an increase in blood flow in the lungs to the levels that can be observed when the body is in a horizontal position.
Suction forces:
Work of the heart. At the moment when blood is expelled from the heart, the ventricles and atrioventricular septa shift downwards, thereby leading to an increase in the capacity of the right atrium. As a result of this, the pressure in it quickly decreases and the blood flow from the vena cava increases sharply, which is due to the increased pressure gradient. The manifestation of the suction action of the ventricles is less, the further from the heart a particular area of the human body is located. For example, changes in venous pressure associated with contractions of the heart muscle were not detected in the abdominal cavity, either in a vertical or horizontal position of the body. The suction force of the heart ceases to affect the pressure level in the inferior vena cava just below the diaphragm.
Breathing movements. If a person's breathing is normal, then changes in intra-abdominal pressure affect venous flow to the heart only to a small extent. This is due to the fact that when, at the moment of lowering the diaphragm, the intra-abdominal pressure briefly becomes higher, this is countered by an increase in the resistance of the vessels located in the liver. When a person takes a deep breath or strains, the increase in intra-abdominal pressure has a greater effect on venous return. If intrathoracic pressure decreases, this affects venous return from a physiological point of view: the pressure in the vena cava decreases and the venous pressure gradient increases. During quiet breathing, the pressure in the chest during exhalation is 5 cm of water column, and during inspiration - 10 cm of water column. If breathing is forced, then the chest pressure decreases much more, which can lead to collapse of the venous walls and cessation of venous inflow. It is worth remembering that respiratory movements affect distant parts of the venous system, which is how they differ from the suction force of the heart.
Treatment
In the initial stages, it is often possible to do without medications, with the help of additional non-drug interventions. It is possible to prescribe physiotherapeutic procedures, osteopathy, reflexology. The results of treatment are assessed using ultrasound.
But the first step that needs to be taken to treat a violation of venous outflow is to consult a neurologist. In case of serious disorders and complications, treatment begins with drug therapy. Restoration of the nervous system, increased vascular tone, and elimination of vein compression are required. Treatment with medications is carried out in parallel with non-drug treatment. Therefore, in parallel, the patient is prescribed a visit to an osteopath and physiotherapy sessions.
Treatment continues until the problem is resolved. This may take several weeks or months depending on the severity of the disease and the individual characteristics of the body.
Treatment of venous outflow disorders
Typically, patients are prescribed the same drugs - venotonics - as for chronic venous insufficiency of the lower extremities.
However, a much more effective method is osteopathy: there are many osteopathic techniques that affect the possibility of improving the outflow from the venous sinuses, as well as techniques that can affect the suture between the occipital and temporal bones, where the outlet of the jugular vein is located, through which 95% of the discharge occurs. blood from the head.
Using these methods, an osteopathic doctor can improve blood flow and outflow of venous blood, which will quickly and permanently alleviate the condition of a patient suffering from chronic cerebral venous insufficiency.
Vladimir Bykov, leading osteopathic doctor (chiropractor, neurologist) Osteopolyclinic.
The article is located in the sections: OSTEOPATHY FOR ALL NEUROLOGY AND MANUAL THERAPY