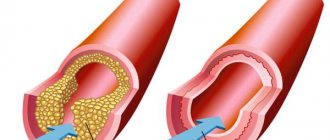
Stenosing atherosclerosis is a chronic vascular disease in which the lumen of the vessel narrows due to the formation and increase in size of atherosclerotic plaques. The disease is accompanied by pathological changes in the structure of the walls of the affected vessel, as well as impaired nutrition and oxygen supply to the surrounding soft tissues. The main reason for the development of atherosclerosis is a high level of cholesterol in the blood, which is gradually deposited on the walls of blood arteries in the form of fatty plaques, narrowing their lumen and disrupting normal blood circulation. The disease is diagnosed mainly in patients aged 50–55 years. Timely detection of such vascular pathology makes the prognosis for successful treatment as favorable as possible.
Difference between stenosing and non-stenosing atherosclerosis
Atherosclerosis is a chronic vascular disease that develops with age, and all people are susceptible to it. At the initial stage, the plaques in the vessels are small, but if they do not block the vessel by more than half, this condition is called non-stenotic atherosclerosis. In this case, there are simply no signs of atherosclerosis, and the person feels great. As the cholesterol plaque grows, the vascular lumen becomes blocked—arterial stenosis occurs. In this case, organs deprived of the usual amount of oxygen and nutrients suffer from ischemia. This explains why the diagnosis of “stenotic atherosclerosis” occurs mainly in older and elderly people.
How is stenosis formed in atherosclerosis?
The study of atherosclerosis is still ongoing. The main role of disturbances in fat and protein metabolism and the proliferation of connective tissue in the area of the affected vessel has been established. The earliest sign is the accumulation of macrophages-phagocytes in the artery. It is associated with the consequences of virus attacks. Cells of the inner membrane grow, collagen and fibrin are released.
Conditions are created for platelets to “stick.” The optimal places for the branching of blood vessels are (division of the carotid artery into external and internal branches, origin of the coronary arteries). The deposition of low-density lipoproteins and fibrin is added to the blood cells.
The process depends not only on eating a large amount of animal fats, but also on special sensitivity, inherited.
Consequences
Among the causes that provoke various diseases of the blood vessels of the legs, heart, and brain, stenosing atherosclerosis occupies a leading position.
- If the coronary vessels are affected, symptoms of cardiac ischemia occur. Coronary heart disease makes itself felt by chest pain and shortness of breath during exercise. This diagnosis ends with myocardial infarction. Every year, thousands of people are admitted to cardiology hospitals in Moscow due to atherosclerosis of the heart vessels.
- When stenosing atherosclerosis affects the arteries of the vascular system of the legs, obliterating atherosclerosis of the lower extremities occurs - a disease that threatens disability and amputation of the limb.
- Atherosclerotic plaques in the vessels supplying the kidneys lead to the development of renovascular hypertension and renal dysfunction.
- If the neck vessels narrow and the arteries supplying blood to the brain (BCA - brachiocephalic arteries) are blocked, stenosis in the damaged area leads to cerebral ischemia and stroke. Read more about stenosing atherosclerosis of the brachiocephalic arteries and its consequences in the following publication.
Symptoms of stenosing atherosclerosis
In the early stages of development, the symptoms of stenosing atherosclerosis are nonspecific and often do not force the patient to seek medical help. Periodically, painful sensations in different parts of the body may occur, indicating tissue ischemia. Unreasonable paresthesias are a consequence of blockage of small vessels that provide nutrition to the sensitive cells of the skin.
If atherosclerotic changes affect the carotid arteries, the following pathological symptoms occur:
- blurred vision;
- frequent headaches, dizziness;
- disorientation;
- unsteadiness of gait;
- numbness of the upper and lower extremities.
With vascular stenosis of the lower extremities, the following symptoms develop:
- lameness;
- feeling of muscle fatigue;
- soft tissue atrophy;
- burning, goosebumps;
- muscle pain that worsens after walking or physical activity.
With damage to the coronary arteries, the clinical picture is as follows:
- pain in the left side of the chest;
- shortness of breath, disturbing even at rest;
- violation of myocardial contractility.
Risk factors
In addition to the age-related changes in the condition of blood vessels that we have already mentioned, atherosclerosis is caused by factors associated with a person’s habits and lifestyle. Smoking, alcohol abuse or fatty foods increase the risk of developing atherosclerosis. Nicotine causes vascular spasms, and alcohol and junk food increase cholesterol levels, which contributes to the formation of atherosclerotic plaques. People who lead a sedentary lifestyle are at risk. Among the causes of coronary heart disease and other vascular diseases, hereditary predisposition is also noted.
Atherosclerosis of the carotid arteries
What is atherosclerosis of the carotid arteries. One of the most common causes of arterial damage is atherosclerosis. Atherosclerosis is a systemic disease that results in the pathological deposition of cholesterol and fat on the inner wall of the artery, leading to the formation of plaque. Over time, the plaque grows, blocks the internal lumen of the artery and impedes blood flow as a result. Atherosclerosis affects all arteries supplying blood to the brain - vertebral and carotid; the aorta and arteries of the lower extremities, as well as arteries supplying internal organs - visceral and renal arteries.
Why is atherosclerosis dangerous?
Due to the narrowing of the carotid arteries, the blood supply to the brain sharply decreases and a stroke (acute cerebrovascular accident or cerebrovascular accident) can occur with a variety of motor and sensory disorders, including paralysis, and speech disorders. Sometimes a fragment or thrombus breaks off from the surface of an atherosclerotic plaque of the carotid artery, leading to the same consequences. In 70% of cases, a cerebral stroke develops without any warning signs, and in 40% of cases, a stroke leads to the death of a person. It is believed that after the artery lumen narrows by more than 60%, the likelihood of developing a stroke increases sharply.
Who may be at risk?
The following groups of patients are at greater risk of developing atherosclerosis of the carotid arteries:
- with high blood pressure
- with high blood cholesterol levels
- with diabetes
- obese
- smokers, etc.
Symptoms of arterial damage.
It is important to know! Damage to the carotid arteries often occurs without any complaints or symptoms!
Who should see a doctor and what tests should they undergo?
If there are predisposing factors in your life:
- age over 55 years,
- smoking,
- hypercholesterolemia (abnormal increase in blood cholesterol levels),
- hereditary predisposition (stroke or heart attack in relatives),
you need to undergo a special study - duplex scanning of the carotid arteries (brachiocephalic) and seek advice from a vascular surgeon.
Indications for surgical treatment.
Large - hemodynamically significant, i.e. disrupting the flow of blood through the carotid artery - atherosclerotic plaques are an indication for surgical treatment to prevent the development of stroke.
Possibilities of surgical treatment.
There are several types of surgical treatment:
- open surgical removal of plaque from the lumen of the artery (carotid endarterectomy)
- endovascular treatment - placement of a stent into the lumen of the vessel.
The surgeon makes a decision on the volume and type of surgical treatment based on the results of the examination.
Possible consequences of the operation.
These operations are usually safe. The likelihood of complications developing is estimated at 1-2%. The most important thing is that in the future, repeated narrowings usually do not occur and strokes do not develop. History of a patient at MCSC.
A 70-year-old man contacted the MCSC. He previously suffered a stroke due to blockage of blood flow through the right internal carotid artery. As a result, my right arm and leg began to work poorly. With a diagnosis of atherosclerosis of the carotid arteries, he was admitted to the vascular surgery department of the Moscow Scientific Research Center.
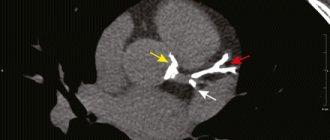
MCSC specialists diagnosed atherosclerosis of the carotid arteries: atherosclerotic stenosis (narrowing to a minimum) of the left internal carotid artery by 90%, and performed carotid endarterectomy (direct removal of atherosclerotic plaque from the affected artery) in order to prevent stroke on the left. The patient was successfully operated on in our Center.
Rehabilitation was easy. On the fifth day, the patient was discharged and returned home without assistance.
Doctors at the vascular surgery department managed to improve the patient’s quality of life and prevent a second stroke.
How to detect atherosclerosis?
To identify atherosclerosis, it is recommended that all people over 40 years old have a preventative blood test twice a year for the following indicators:
- lipoproteins, cholesterol, triglycerides;
- glucose;
- fibrinogen;
- coagulability.
They may indirectly indicate a disorder of protein-lipid metabolism.
Special methods include:
- intravenous and arterial angiography of blood vessels - a series of images after the injection of contrast into the artery;
- rheovasography - blood viscosity and patency are examined;
- Doppler study - diagnosis is based on echographic signs caused by the passage of a sound wave through the vessels and the return signal. Computer processing allows you to register a graphic image in color.
The triplex scanning technique is used. It allows you to identify:
- the degree of narrowing of the arteries;
- atherosclerotic plaques, blood clots in a vessel;
- detachment of the choroid of the artery;
- change in direction, shape of blood vessels, presence of loops, additional bends;
- mobility and elasticity of the wall;
- the likelihood of aneurysm formation.
The ultrasound examination method is indispensable for deciding on the use of surgical treatment
"Bad" and "good" cholesterol
This complex organic compound belongs to fats, more specifically to fatty alcohols. Cholesterol is involved in various processes in our body, for example, it is a kind of building material for cell walls, and is also part of hormones and vitamins.
For the most part (about 70%) cholesterol is produced in the liver, the remaining amount enters the body through food. There is no cholesterol in the body in its “pure form”, since it is part of complex compounds of fats and protein - lipoproteins (lipoproteins).
Atherogenic (promoting the development of atherosclerosis) are low-density lipoproteins (LDL), containing up to 45% cholesterol. Low-density lipoproteins transport cholesterol from the liver to cells, where it participates in the synthesis of cell membranes. LDL and VLDL cholesterol are the main risk factors for the development of atherosclerosis, since these compounds easily pass into the vessel wall and form an atherosclerotic plaque.
High-density lipoprotein (HDL) contains much less cholesterol and much more protein and phospholipids (approximately 50%). They, on the contrary, are able to remove cholesterol from the walls of blood vessels and other tissues and transport it to the liver for “disposal”. Therefore, HDL cholesterol is considered “good.” The ratio of “bad” and “good” cholesterol determines the atherogenicity coefficient.
Stages of atherosclerotic plaque formation
There are proven stages in the formation of atherosclerotic plaque:
- Pre-lipid.
- Lipoidosis.
- Liposclerosis - the plaque grows inward, at this stage the narrowing of the arteries begins.
- Atheromatosis – a loose mass of fatty inclusions forms in the center of the plaque.
- Ulceration - the stage is dangerous because part of the plaque breaks off and turns into an embolus.
- Atherocalcinosis - the deposition of calcium salts compacts the affected area of the vessel, deformation of the artery occurs.
Clinic of atherosclerosis of coronary vessels
Atherosclerosis of the coronary (coronary) vessels contributes to the manifestation of chronic myocardial ischemia in the form of angina attacks, causes arrhythmia due to the development of foci of cardiosclerosis, and gradually leads to circulatory failure.
Patients are concerned about:
- Substernal pain, at the initial stage associated with physical and nervous stress, which subsequently occurs at rest. Irradiation to the left arm, shoulder blade, jaw. The duration of the attack is up to 30 minutes. Removable with Nitroglycerin.
- Tachycardia.
- Dizziness.
The acute manifestation is myocardial infarction with subsequent severe complications (formation of cardiac aneurysm, rupture, cardiogenic shock) or sudden death syndrome. For acute heart attack:
- The pain is very intense, radiating, as with angina, but lasts up to a day or more.
- Often accompanied by unexpected complex arrhythmias.
- The pressure drops, weakness and dizziness occur.
Diagnosis and treatment of atherosclerosis of the brachiocephalic arteries in the clinic on the Yauza
The development of atherosclerosis can be detected using instrumental studies of the brachiocephalic arteries. At the medical center on Yauza, you can undergo several diagnostic procedures to accurately determine the presence and characteristics of the disease. To identify pathology, the following are used:
- triplex scanning;
- angiography with contrast;
- multislice tomography.
The hospital does not have outdated equipment. All studies are carried out on modern high-precision devices used in leading clinics in the world.
Aortic atherosclerosis clinic
Atherosclerotic changes in the aorta are among the most common manifestations of the disease. The abdominal region is most often affected. The disease not only causes the formation of aneurysmal dilatation of the wall of the largest vessel with subsequent dissection, but is also dangerous due to its thromboembolic complications.
From the aorta, emboli easily enter the vessels of the kidneys, intestines, and femoral artery and cause tissue infarctions and gangrene at the level of the foot and above. Clinically, this is expressed by sharp cutting pains, dysfunction with increased blood pressure (with embolism in the kidneys), vague intestinal pain, quickly turning into peritonitis due to necrosis and rupture of intestinal tissue (if the embolus enters the mesenteric artery).
Aortic rupture leads to instant death. Delamination can last for several years, but also leads to rupture.
Headache is a symptom of many diseases that requires seeing a doctor and urgent examination.