Cardiac diseases are not always detected by routine methods. Especially functional, in the early stages of their development. Long-term follow-up is required, which apparently healthy patients do not receive.
Slowing of intraatrial conduction is a clinical variant of the disorder in which the intensity of the electrical impulse from the natural pacemaker to the atria weakens.
As it progresses, the entire organ, including the ventricles, becomes involved in the pathological process.
The main and immediate cause is the death of the structures of the sinus (SA) node, which precisely forms the very signal necessary for myocardial contraction.
Treatment has different prospects. Secondary forms (caused by non-cardiac diseases), provided that the main factor of formation is eliminated, are completely stopped.
Cardiogenic diseases cannot be eradicated, but there are good opportunities to slow down and even stop the progression, relieve symptoms and equalize the patient’s chances of life with other people who do not have cardiac pathologies.
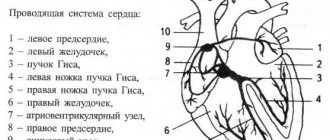
Development mechanism
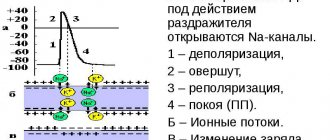
Slowing of impulse conduction through the atria is a consequence of the death of cells of the sinoatrial or sinus node.
As a result of insufficiently intense production of the bioelectric impulse, weak activity of the myocardium itself is observed. First, only the atria, then the ventricles and the entire muscular organ as a whole suffer.
Read more about intraventricular conduction disorders here.
Up to a certain point, violations are not visible at all; information about the deviation is provided only by electrocardiography, if you look closely.
As it progresses, bradycardia (slow heart rate) develops. The natural pacemaker produces an insufficiently strong signal, and after reaching a critical cell level, threatening consequences develop. The probability of cardiac arrest increases to 70%; only transplantation can save the patient.
The contractility of the myocardium decreases, the volume of pumped blood decreases, therefore all organs and systems suffer from ischemia. Liver and kidney failure, brain hypoxia, and neurological deficits develop.
Death is a matter of time. Fortunately, such a fatal scenario is not a matter of just one year. There are chances for high-quality diagnosis and the prescription of adequate therapy.
Exercising with arrhythmia
Active sports are contraindicated for people suffering from slow intraatrial patency. In cases where it is complicated by ischemic arrhythmia, any physical and emotional stress becomes strictly contraindicated, as it can provoke a pre-infarction state.
Sudden death syndrome due to arrhythmia occurs even in very young athletes. In most cases, this syndrome develops against the background of previously undetected damage to the conduction system of the heart.
Currently, scientists are paying special attention to the study of arrhythmia in children. This is explained by the specific development of arrhythmia at a young age, which, in the presence of increased physical activity, can provoke pathophysiological changes in the cardiovascular system, and in severe cases, lead to death.
The optimal solution for slowing intraatrial conduction detected on the ECG is the regular implementation of a complex of exercise therapy developed by a medical specialist. Properly selected physical therapy exercises increase the effectiveness of treatment, reduce the rehabilitation period and prevent the subsequent development of pathology.
However, independent exercises performed without prior consultation with a doctor or instructor can have the opposite effect and lead to a deterioration in the patient’s condition.
Classification and degrees
Typifications that are used in clinical practice.
According to the number and nature of symptoms:
- No manifestations. The most common option. There is no picture at all, the patient feels fine. Changes in the electrocardiogram are absent or insignificant. Diagnosing pathology at this stage is a great success.
- With mild symptoms. Deviations occur when 10-30% of the sinus node cells die.
- With pronounced clinical signs. It can be easily detected by objective methods. Treatment is prescribed urgently, there is a risk of death of the patient.
Depending on the current:
- Paroxysmal type. Symptoms or, in their absence, signs on the ECG are inconsistently detected. Develops in episodes. Each lasts from a few minutes to hours. Such moments may arise repeatedly.
- Persistent form. About the same thing, only the duration is longer. Several days in a row.
- Chronic variety. Symptoms and the objective picture do not disappear at all; they are constantly recorded.
- Spicy. The symptoms are most pronounced; with significant cardiac dysfunction, there is a high risk of cardiac arrest and sudden death of the patient.
Depending on the main feature:
- Sinoatrial node block (SA block).
- Slowing down the sinus cluster.
- Classic sinus bradycardia.
All three forms appear approximately the same. ECG findings vary. The critical option is to stop the natural pacemaker. This is a direct path to death, asystole.
Based on etiology:
- Primary variety. Develops as a result of heart disease itself.
- Secondary. Or external. The result is the influence of other pathological conditions.
There are only three degrees of intra-atrial conduction disturbance:
- First. The patient has no complaints about his health. Objectively, minor deviations in the electrocardiogram are detected. The discovery was purely an accident.
- Second. The symptoms are pronounced, the ECG pattern is clearly visible. Specific signs make it possible to detect blockade or disruption of the sinus node. This is the most common point of diagnosis.
- Third. All manifestations are expressed to the maximum extent. The cardiologist notices “his” patients with the naked eye. A cardiogram verifies conduction disturbances. Treatment is urgent, otherwise cardiac arrest will occur as a result of insufficient stimulation and death of the person.
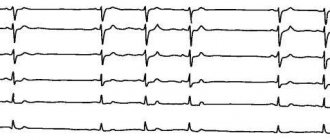
Detection of conduction disorders using Holter monitoring.
Akselrod A.S., Head of the Department of Functional Diagnostics,
Cardiology Clinic of the MMA named after.
THEM. Sechenov Conduction disturbances are less common in cardiologist practice than cardiac arrhythmias. However, a significant proportion of syncope of unknown origin is represented by conduction disorders. If they are transient (which happens quite often), it is extremely difficult to detect them when recording a standard ECG. In such a situation, consistent use of a 24-hour recorder over 3 days or a single use of a 72-hour recorder is absolutely recommended.
As is known, patients with various conduction disorders may not present any complaints for a long time. In such situations, the appearance of syncope is often the first indication for Holter ECG monitoring.
During 24-hour ECG recording, it is possible to detect conduction disturbances that occur only at night. Of course, daily ECG monitoring also reveals the connection between conduction disorders and medication use, physical activity, etc. Transient sinoatrial and atrioventricular blockades, transient frequency-dependent blockades of intraventricular conduction, changes in the degree of previously diagnosed blockade - this is an incomplete list of the most common conduction disorders, which can only be identified with long-term ECG monitoring.
When purchasing software, you should pay attention to the mandatory presence of three features:
1. changing the tape drive speed: this feature allows you to more clearly set the boundaries of the PQ interval and PP distance;
2. changing the overall voltage: this feature allows you to increase the amplitude of the P wave and, thus, visualize it more clearly in doubtful cases;
3. the presence of a ruler with colored stretchable jaws: when you set these jaws to the interval you need, its duration in ms automatically appears on the fragment.
Sinoatrial blocks
associated with a slowdown (grade 1) or disruption (grades 2 and 3) of the generation or conduction of sinus node impulses to the atrial myocardium and, accordingly, the atrioventricular node. Sinoatrial block can be transient or permanent, occur at any heart rate and be combined with other conduction and heart rhythm disorders.
Sinoatrial block 1st degree
can be suspected by fragments of a sudden slowdown in rhythm followed by its acceleration (difficult to differentiate with sinus arrhythmia) during Holter monitoring.
With 2nd degree SA blockade
Some of the impulses arising in the sinus node do not reach the atria. In this case, a pause (more than 2 seconds) without atrial activity is recorded on the ECG: unlike AV block, during a pause with SA block there are no P waves.
With 2nd degree block of type I (partial sinoauricular block with Samoilov-Wenckebach periods)
There is a progressive shortening of the RR intervals before a long pause - Samoilov-Wenckebach periodics. In this case, the degree of conduction disturbance can be characterized by the ratio of the number of sinus impulses, for example, 3:2, etc. (in the numerator the number of sinus signals is set
impulses, including the expected and failed impulses; the denominator is the number of actually conducted impulses). The detected pause is not a multiple of the distance PP of the main rhythm.
For sinoatrial block of the 2nd degree, type II (Mobitz type)
no such periodicals are found. This type of blockade is diagnosed more often. The identified pause is a multiple of or equal to one distance PP of the main rhythm. Often, with this type of blockade with a 2:1 or greater degree of blockade, it becomes necessary to differentiate monitoring fragments from sinus bradycardia. Often, during the same Holter registration, it is possible to register both types of SA blockade.
Pay attention to the ability of your software to display in each of the printed fragments both the duration of the pause and the heart rate value against the background of this pause. This marking makes the fragment very visual and once again emphasizes its diagnostic significance (Fig. 1).
Rice.
1. Patient S., 64 years old, variants of sinoatrial block of the second degree: A - C A block of the 2nd degree, type I with Samoilov-Wenckebach periodicity; B – SA blockade 2nd degree type II with 3:2.
A
B
About the third degree of sinoatrial block (complete sinoatrial block or sinus node failure, “sinus arrest”)
they speak in the absence of atrial waves and the presence of replacement contractions from the distal centers of automaticity - the AV connection or the ventricular conduction system (Fig. 2).
Often during Holter monitoring one can see fragments of conduction disturbances that occur against the background of respiratory arrhythmia. In such a situation, it can be quite difficult to qualify the identified pauses. For example, in patient Zh., 45 years old, at night (from 2:00 to 5:00) episodes of SA conduction disturbance were recorded without multiplicity and clear Samoilov-Wenckebach periodicity, 9 pauses of more than 4 seconds, including 2 episode of sinus node arrest.
Fig.2. Patient Zh., 45 years old: A - episodes of slowing of SA conduction without a clear multiplicity and Samoilov-Wenckebach periodicity, B - arrest of the sinus node with the formation of a pause of 4.048 sec.
A
B
For novice doctors, I would like to note three important points:
1. often the degree and type of blockade may vary depending on the time of day;
2. the lack of multiplicity of the PP interval and the duration of pauses may be due to concomitant sinus arrhythmia, often respiratory;
3. when qualifying a pause as an SA blockade, you must be absolutely sure that this fragment is not artificial: the pause is duplicated in both leads. In doubtful cases, monitoring will have to be repeated.
Atrioventricular blockade.
Atrioventricular (AV) blocks are caused by damage to the conduction system at the 2nd and 3rd levels - the conduction of the sinus impulse to the atrioventricular node, as well as pathology of the atrioventricular node itself. In this case, both a delay in the conduction of the impulse from the atria through the AV node, and a complete cessation of its conduction are possible.
Prolongation of the PQ interval by more than 200 ms in adults and more than 170 ms in children indicates 1 degree of AV block (slowing of AV conduction)
. Incidental detection of this type of blockade at night in patients taking beta-blockers and not showing any complaints is one of the most common favorable conduction disorders in practical cardiology and can be qualified in conclusion as “slowing of AV conduction” if PQ does not exceed 300 msec (Fig. 3).
Rice. 3. Patient R., 57 years old: slowing of AV conduction was detected during night sleep (PQ interval reached 240 ms). A – PQ 146 ms (15:10), B – PQ 240 ms (4:33).
A
B
A much greater danger is posed by a significant (more than 300 ms) slowdown in AV conduction, which must be qualified in the conclusion as “1st degree AV block” (Fig. 4). When a PQ interval of more than 300 ms is recorded on the resting ECG, the patient is advised to have 24-hour ECG monitoring to decide on the need for therapy correction. Such severe conduction disturbances often progress over the course of a day.
Fig.4. Patient G, 64 years old: 1st degree AV block
“Loss” of the ventricular complex (pause, a multiple of the duration of the RR interval) with registration of an unchanged P wave (as opposed to sinoatrial block) is a sign of 2nd degree AV block
.
With an increasing lengthening of the PQ interval before the pause, they speak of type I partial AV block of the 2nd degree with Samoilov Wenckebach periods (Mobitz type I)
.
In the absence of such periodicals, type II AV block of the 2nd degree (Mobitz type II)
. It is convenient to indicate the degree of conduction using the ratio 5:2, 3:2, etc. (the first digit indicates the number of P waves, the second - the number of ventricular QRS complexes). It can be extremely useful to use graphs (or tables) of the distribution of pauses by hour. At the same time, having distribution graphs in your program is much more convenient: they are more visual and allow you to quickly and correctly assess the prevalence of pauses by hour (Fig. 5).
Fig.5
.
Patient B, 76 years old: 2nd degree AV block, type II.
A – stereotypical fragment of blockade with the formation of a pause of 2.288 sec; B – graph of the distribution of pauses by hour (predominance at night is expressed) A
B
Complete atrioventricular block (3rd degree AV block, complete transverse block)
is detected as a loss of connection between atrial (P wave) and ventricular contractions (QRS complex), while the atrial rhythm is more frequent than the ventricular one (Fig. 6). In such fragments one can see the layering of P waves on the ventricular QRS complexes, so the possibility of increasing the total voltage (and, accordingly, the amplitude of the P wave) is simply necessary.
Fig.6. 3rd degree AV block in patient Zh., 69 years old.
Often, against the background of 3rd degree AV block, replacement contractions or rhythms are recorded (Fig. 7).
Fig.7.
Patient G, 64 years old: replacement idioventricular rhythm against the background of 3rd degree AV block.
Quite often in patients, AV block occurs sporadically or its degree varies depending on the time of day. Rare episodes of 2nd degree AV block may also occur at night (usually in the early morning hours) with a normal PQ interval for the rest of the monitoring time. In addition, during follow-up of a patient with AV block, one can often see a progressive deterioration of AV conduction over several years (Fig. 8).
Fig.8.
Progressive deterioration of AV conduction in patient L., 45 years old: A – slowing of AV conduction was first detected at the age of 45 years; B – 2nd degree AV block type II at 46 years old; C and D – 2 consecutive episodes of 3rd degree AV block 3:2 and 5:2 with the formation of pauses of 2.31 and 5.34 seconds, respectively.
A
B
IN
G
Every novice doctor is faced with the difficulty of differential diagnosis between 2nd degree AV block type II and 3rd degree AV block. Only with a detailed comparison of the fragments and the use of the “ECG review” option can we conclude that there is a complete transverse blockade on the controversial fragment.
Blockades of the branches of the His bundle
A standard 12-channel resting ECG allows you to clearly diagnose variants of conduction disorders along the His system. During daily ECG monitoring, it is possible to identify transient blockades of the branches of the His bundle, which are recorded at night or, conversely, during intense physical activity. They are often an incidental diagnostic finding. However, such intraventricular conduction disturbances (for example, transient complete block of the left bundle branch) can mimic paroxysmal ventricular arrhythmias and lead to overdiagnosis of life-threatening arrhythmias (Fig. 9).
Fig.9.
Patient K., 72 years old: transient complete blockade of the left bundle branch. A – beginning of the blockade, B – end of the blockade.
A
B
As a rule, it is not difficult to differentiate conduction aberration along the His system from paroxysmal ventricular rhythm disturbances: the block is characterized by a regular regular rhythm, smooth regular cycles, the absence of a compensatory pause (or lengthening of the RR interval) at the end of a rhythm fragment from extended complexes and a smooth restoration of normal sinus rhythm .
None of the listed signs can be seen in Fig. 10, which allows us to qualify this fragment as ventricular tachycardia. Rice. 10. Patient K., 79 years old: paroxysm of unsustained ventricular tachycardia
In conclusion, I would like to note: for a clear diagnosis of conduction disorders, a single Holter recording is often not enough. If there are dubious changes suspicious for conduction disorders (especially at night), the study must be repeated with a total monitoring duration of up to 72 hours.
Moscow, 04/16/2009
Causes cardiac
All factors need to be considered in the system. During the survey, they are excluded one by one.
A sharp increase in blood pressure
If, against the background of chronic hypertension and a gradual increase in blood pressure, the body somehow manages to adapt to new, albeit difficult, conditions, a rapid increase in the tonometer reading leads to overload of the right atrium.
The result is damage to the cells of the sinus node. If such episodes are repeated, and this is exactly what happens against the background of uncorrected hypertension, more and more cells die.
Progression depends on the course of headache. Crises have an even more severe impact.
Inflammation of the heart muscle or myocarditis
It has a detrimental effect mainly on the atria. Without treatment it leads to tissue destruction and severe scarring.
The sinus node is located in the right chamber, and its partial destruction is possible. Slow conduction is a complication of the disease.
The nature of inflammation can be infectious or autoimmune. Both forms are acute, with a pronounced clinical picture of the heart, blood vessels, respiratory and nervous systems.
Treatment is strictly in a hospital. Endocarditis is a similar pathological process affecting the inner lining of the heart. Less often it leads to a slowdown, but this is also possible.
Coronary insufficiency
Narrowing or blockage of special arteries that supply the heart itself. Tissue necrosis is a variant of the condition. Another is possible. The so-called angina pectoris.
It is not so catastrophic; there is death, but the process does not reach that critical point when destruction leads to damage to large areas.
May last for years. It flows spasmodically. In waves. Each episode destroys part of the myocardium. The result is insufficiency and dysfunction. The sinus node suffers not least.
In addition to the death of cardiomyocytes, scarring of the impulse pathways occurs. The so-called bundle of His and its branches (legs), which leads to blockade.
Atherosclerosis of the coronary arteries or aorta
The essence of the process is the formation of cholesterol plaques that close the lumen of blood vessels. Blood flow weakens, pressure in the atria and ventricles increases.
How the growth of the indicator ends is with an increase in load and tissue destruction at the cellular level.
There is another variant of pathology - narrowing of the lumen of the arteries. This is the result of smoking, vasculitis, when the walls of blood vessels scar and close, alcohol abuse, and other autoimmune pathologies.
Treatment is urgent, conservative in the first stages. If ineffective, surgical intervention is indicated.
Heart attack
Acute circulatory disorder in the heart muscle. Leads to rapid destruction of cardiomyocytes. The process is avalanche-like, the longer the ischemia is observed, the more significant the area of destruction.
Major heart attacks are almost guaranteed to result in death. Even with colossal luck, the process will not pass without a trace. Heart regeneration is impossible. The affected tissue is replaced by scar tissue, unable to contract or create impulse. The result is ischemic disease.
Therapeutic measures
Slowing of intraatrial conduction on the ECG, occurring in an acute form, requires specific therapy.
| Drug groups | Drug names | Action provided |
| Anticholinergics | atropine, scopolamine, platyphylline | Reducing smooth muscle tone, improving the conduction of electrical impulses in the heart. |
| Vasopressors | norepinephrine | Increased blood pressure |
| Glucocorticoids | hydrocartisone | Stopping and relieving inflammation |
| Diuretics | lasix, furosemide | Removing excess potassium and fluid from the body. |
| Cardiac glycosides | cordigitite, lantoside, adonis-bromine | Elimination of arrhythmia, stimulation of the heart muscle. |
In some cases, the doctor decides on the advisability of using sedatives.
Pregnant women are prescribed magnesium supplements, which do not have a negative effect on the development of the fetus. Other medications aimed at improving intraatrial conduction are used only for clinical indications when there is a threat to the mother's life.
Extracardiac causes
Other factors also play a role, although they are not directly related to the heart. They are easier to correct, and there is the possibility of completely eradicating conduction disorders:
- Cardioversion performed. Prescribed to patients with paroxysmal tachycardias and other arrhythmias. The procedure involves placing electrodes and passing a charge through the heart.
A side effect is a slowdown in conduction due to dysfunction of the sinus node. Correction using medications.
This is a reversible condition. The acute period requires resuscitation, but this phenomenon occurs relatively rarely.
- Compression of the neck at the level of the carotid sinus. As a result of wearing clothes with a tight collar, tie, jewelry. The process is also reversible, but threatening acute variants of the condition are possible. Nocturnal cessation of breathing or apnea. It develops in patients with ENT problems, obese people, and severe snoring. Heart pathologies in this category of people are a proven fact. The condition needs to be corrected as soon as possible.
- Stroke affecting the subarachnoid space. Violation of cardiac activity is a purely reflex act associated with dysfunction of the parasympathetic region of the autonomic nervous system. Requires urgent medical attention. A prerequisite for the development of deviations is bleeding. The same effect is observed in traumatic brain injuries with the formation of a hematoma.
- Prolonged or improper use of certain medications. Particularly dangerous are cardiac glycosides, calcium antagonists, beta-blockers, neuroleptics, anxiolytics (tranquilizers), mood stabilizers, psychotropic drugs in general, opioids, narcotic analgesics, corticosteroids in inappropriately large dosages, and others. Correction of the treatment regimen or replacement of drugs is required.
- Excessive amount of potassium in the body. Excessive consumption takes its toll. It is difficult to achieve such a concentration with food; most likely, the patient is taking drugs like Asparkam.
- Excess calcium in the bloodstream. The result of leaching of mineral salt from bones. Observed in cases of cancer and prolonged immobilization. Osteoporosis. The nutritional factor does not play a role.
- Intoxication with salts of heavy metals, tumor decay products (for cancer, especially advanced ones).
- Increased intracranial pressure (hypertension caused by impaired outflow of cerebrospinal fluid).
Factors are taken into account in the system. Diagnostics puts an end to the issue. It is extremely rare that no cause is found. Then they talk about the idiopathic form. May be revised in the future.
How does pregnancy go with this diagnosis?
Any disruptions in the functioning of the female body during pregnancy are unpredictable, especially when it comes to heart pathologies. Rhythm disturbances are a serious medical problem that threatens the life of the fetus. The mechanisms for the development of such deviations are usually associated with hormonal changes and functional changes that occur in a pregnant woman.
If there is any deviation in the functioning of the cardiovascular system, the patient is referred for diagnostics. The research methods are practically no different from the generally accepted ones. If necessary, drug therapy is prescribed, including antiarrhythmic drugs.
Symptoms
The clinical picture is variable. In some cases it is absent altogether. The patient does not experience any difficulties in everyday life or when performing work duties.
Attention:
Insufficient conductivity is an incidental finding. There are also acute forms that are aggressive and often end in death.
A sample list of symptoms looks like this:
- Blood pressure surges. Sometimes low, sometimes high. The change in numbers is not due to any external factor, such as physical activity or food intake. This is a spontaneous process. As it progresses, frequent crises with high tonometer readings develop. The effect of the drugs is minimal.
- Peripheral edema. The lower extremities suffer, less often the fingers. Face.
- Dyspnea. After intense physical activity. When the process enters the critical phase (stage 3 and beyond), it is observed in a state of rest.
- Discomfort and pain in the chest of moderate intensity. Severe attacks are uncharacteristic, although this is also possible with a parallel course of angina pectoris. Nitroglycerin has no effect.
- Darkening in the eyes, tinnitus, headache, fog in the field of vision, flickering, vertigo, inability to navigate in space, fainting. The result of insufficient blood circulation in cerebral structures.
- Weakness, drowsiness, decreased performance. Already from the second stage. In some cases, symptoms are also detected at the first stage.
- Bradycardia. Decrease in heart rate. Up to 50-60 beats per minute and below.
During acute periods or moments of deterioration, apathy or psychomotor agitation, fear, suffocation, pallor of the skin, mucous membranes, and cyanosis of the nasolabial triangle are also noted.
As part of the development of heart failure, ascites is possible - an enlargement of the abdomen due to the accumulation of fluid.
How does pathology affect the functioning of the body?
With a partial disorder of sinoarterial conduction, no symptoms appear, but with a complete disorder, an adult may experience pain in the chest and dizziness caused by poor blood flow in the brain against the background of rare heart contractions.
As for interatrial block, it does not pose a threat to life. But its presence increases the risk of developing atrial fibrillation, which is a serious threat to human health. This disorder is accompanied by shortness of breath at rest and when walking, swelling of the legs, bluish discoloration of the skin, and discomfort in the chest.
Atrioventricular block is not always expressed by symptoms, but its combination with bradycardia can lead to an attack of MAS (Morgagni-Adams-Stokes). The patient at this moment may suddenly feel weak in the body. It is possible that you may experience dizziness or even loss of consciousness. Seizures associated with deterioration of blood supply to the blood vessels of the brain may also occur. This condition requires emergency medical attention. Inaction can cause cardiac arrest.
The intraventricular type of pathology occurs due to a disorder of ventricular conduction through the bundle branches. Partial blockade does not always manifest itself, but complete blockade is accompanied by a rare pulse, loss of consciousness, and pain in the chest.
Diagnostics
It takes place on an outpatient basis. Impaired intra-atrial conduction means that there is damage to the sinus node. A thorough examination is required to detect the causes of this phenomenon.
Sample list:
- Oral interview with the patient by a cardiologist. When complaints appeared, whether they exist at all, how much they interfere with daily activities and other points are subject to clarification.
- Anamnesis collection. Family history, lifestyle, past or current pathologies.
- Measurement of blood pressure and heart rate. The classic picture is that blood pressure is unstable, even when the procedure is repeated after 10-15 minutes, an increase in the indicator prevails. Heart rate is consistently below normal.
- Daily monitoring. Gives a lot of information about the dynamics of the same levels over 24 hours. The result is an indirect confirmation of the presence of conduction disturbances in the atria.
- Echocardiography. Visual assessment method. Deviations of anatomical development are detected only with gross defects, after a heart attack, inflammation and other moments. In advanced forms, the left ventricle enlarges and blood flow is disrupted.
- X-ray of the chest. An increase in the pulmonary pattern and an increase in the size of the heart are detected.
- ECG. Profile research. Gives basic information. Typical features: decreased pulse, deformation or complete disappearance of atrial waves (P), heart rate does not increase during physical activity, detection of replacement sliding complexes. A slowdown in AV conduction on the EGC is recorded even in the early stages.
EPI is also performed (for severe concomitant diseases, the technique is not used); if necessary, a consultation with a neurologist is prescribed.
ECG and other diagnostic methods
Slowing of intraatrial conduction is detected on ECG, EPI or Holter monitoring. Standard electrocardiography is a mandatory and most accessible examination method used in all medical institutions. It is based on the registration of bioelectric signals occurring during heart contractions using graphic images.
Holter monitoring is an ECG that lasts from 24 hours to a week. This method makes it possible to record and track the bioelectrical activity of the heart in everyday situations.
To carry it out, electrical impulse sensors are attached to the patient’s body. The information they read is displayed on the monitor screen and is subsequently interpreted by a cardiologist.
During the examination period, the patient leads a normal lifestyle, including work, eating, physical activity, travel, sleep and other normal activities.
A person must write down information about his physical and emotional state in a diary. It also indicates data on food intake and medications, duration and quality of sleep, and changes in well-being.
EPI (electrophysiological study of the heart) is an expensive method performed in a hospital setting.
There are 2 types of this examination, used in the study of various pathologies.
In the first case, special catheters are installed in the veins of the patient’s upper and lower extremities. Electrodes are inserted through them, through which electrical stimulation of the cardiac conduction system is carried out. In this way, it is possible to cause, eliminate and study the parameters of emerging conduction disturbances.
A simpler type of EPI is the transesophageal insertion of a probe-electrode, through which the left atrium is stimulated. This method allows you to study the most common types of slowdowns in the conduction of cardiac impulses, as well as accurately determine sick sinus syndrome, which is common in older people.
Treatment
{banner_banstat9}
Therapy depends on the form and course. Early stages that do not produce obvious symptoms and do not interfere with the patient in any way do not require urgent supervision. Further examination and clarification of the etiology of the process is necessary.
In case of secondary origin, the underlying disease is eliminated. Cardioprotectors, such as Mildronate, and vitamin and mineral complexes are prescribed as a supportive measure.
The patient is monitored every 3 months. Deterioration of the condition is the basis for surgical intervention. The way is implantation of a pacemaker, which artificially creates the required electrical impulse.
As a measure to prepare for surgical treatment, the use of antiarrhythmics (Amiodarone), antihypertensives (Perindopril in different trade variations, Moxonidine, Diltiazem or Verapamil, others, at the discretion of the treating specialist), diuretics, and cardioprotectors is indicated. Cardiac glycosides as needed.
Also indicated are cessation of smoking, drinking alcohol, excessive physical activity, and consumption of fatty foods (treatment table No. 10).
Correction methods and treatment: what and when to do
An isolated disturbance in the conduction of impulses along the interatrial fibers, which is not accompanied by clinical symptoms, does not require treatment. Drug therapy is prescribed for the development of arrhythmias with hemodynamic disturbances: atrial fibrillation, extrasystole, paroxysmal tachycardia.
Groups of drugs used:
- antiari, Cordarone, Etatsizin, Bisoprolol.
- cardiac glycosides: Digoxin;
- diuretics: Eplerenone, Spironaloctone, Torsemide.
High-degree intraatrial blocks that cause symptoms of heart failure require a pacemaker (artificial pacemaker). Installation of electrodes in both atria allows synchronizing the work of the myocardium.
Forecast
{banner_banstat10}
Depends on the diagnosis. Primary forms cannot be cured, but in the early stages they can be corrected with medication, the survival rate is 90% or higher.
Secondary ones require relief of the cause. Mortality due to atrial conduction disorders generally ranges from 10-60%, acute forms are fatal in 40% of situations. The death of more than 90% of sinus node cells almost always leads to death.
Young patients without bad habits, with a good family history, relatively healthy, have a better chance of survival.
Surgical treatment
If conservative therapy is ineffective, the following surgical methods are used:
- implantation of a pacemaker;
- replacement of heart valves with artificial analogues
Implantation of an electrical stimulator has no age restrictions. In the future, operated patients can lead a full life. They should only avoid exposure to strong electromagnetic waves, including undergoing magnetic resonance imaging.
People with built-in pacemakers should periodically visit a neurosurgeon and cardiologist to check the functionality of the device and adjust its settings.
This implantation is possible even during pregnancy. But, if there is no real threat to life, then doctors recommend refraining from surgery until 8 weeks. The installation of a pacemaker must be carried out under the supervision of an echocardiograph and using means that provide maximum protection for the fetus.
If conduction disturbances are caused by pathological changes in one of the heart valves, then the specialist suggests replacing it with a mechanical or biological artificial analogue. The choice is determined by a number of factors that the doctor evaluates after conducting numerous examinations and obtaining the results of laboratory tests of the patient’s blood.
The mechanical heart valve is reliable and does not require replacement. However, after its installation, a person must constantly use medications that reduce blood clotting.
Biological valves begin to gradually deteriorate after a certain period of operation. Therefore, they are recommended to be installed by elderly people.
Complications
The cause of intraatrial conduction disturbance is weakness or dysfunction of the sinus node.
The condition threatens with the following consequences:
- Cardiac arrest or asystole. The result of insufficient stimulation of cardiac structures, in particular the muscle layer.
- Heart attack. The result of poor nutrition. Little blood flows through the coronary arteries. Hence acute necrosis or, at least, repeated attacks.
- Stroke. Death of nerve cells and tissues. Ends in death or permanent neurological deficit.
- Cardiogenic shock.
- Fainting and injuries incompatible with life.
- Vascular dementia.
All conditions, one way or another, lead to a minimum of severe disability. There is no point in delaying therapy, if indicated.
Treatment of cardiac conduction disorders
- Medication - the doctor may prescribe vitamins and restoratives, a diet (limiting fatty and sweet foods, eating more fresh vegetables and fruits), as well as drugs to cure or reduce the symptoms of the disease that caused the blockade (if the cause is known).
- Surgical – used in case of ineffectiveness of drug treatment, frequent fainting and malignant (life-threatening) course of the disease. An electrical pacemaker (ECS) is installed - a small device that generates the correct heart rhythm, which sets the heart to contract correctly and rhythmically.