Pathological conditions that are manifested by changes in the frequency and strength of heart contractions. They manifest themselves as pain in the heart, rapid heartbeat, irregular heartbeat, shortness of breath and dizziness. Heart conduction disturbances (blocks) are a common finding on electrocardiographic (ECG) examinations. Most often, they do not manifest themselves clinically, but some blockades require the implantation (installation) of a permanent pacemaker (pacemaker).
Many types of intracardiac blockades (for example, incomplete blockade of the right bundle branch) are a normal variant.
Cardiological examination for cardiac conduction disorders is intended not only to determine the type of blockade, but also to determine whether it is a manifestation of organic heart damage. In addition, not all cases of blockade need to be treated. The main indications for installing a pacemaker are fainting and pre-fainting conditions, but you need to be sure that fainting is caused precisely by cardiac conduction disorders.
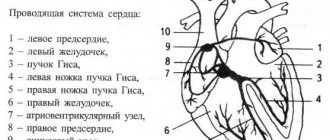
Conduction system of the heart
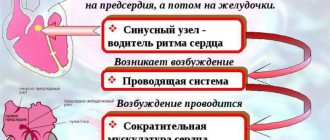
In general terms, the conduction system of the heart (the system responsible for conducting electrical impulses in the heart) is arranged as follows. The impulses are generated by the sinus node located in the right atrium. Along the intraatrial pathways, these impulses reach the atrioventricular (AV) node, where some delay of the impulses occurs: the atria and ventricles must contract at the same time. The impulse then travels along the bundle branches to the cells (cardiomyocytes) of the ventricles. The bundle of His consists of two legs - right and left. The left bundle branch consists of two branches - anterior and posterior.
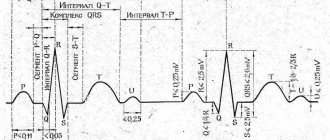
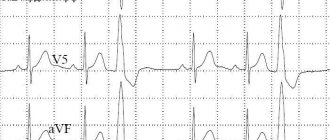
ECG
An ECG is a method of recording bioelectric potentials generated by the heart muscle.
ECG analysis is carried out in the following sequence:
1. assessment of the rhythm and conductivity of the heart and characteristics of their disorders.
2. differentiation of variants of the electrical activity of the heart from its pathological rotation.
3. identification of a complex of differential diagnostic signs.
4. assessment of nonspecific changes.
5. generalization of the detected deviations from the norm in the ECG conclusion, it indicates mainly the immediate cause that led to the development of changes in the ECG: hypertrophy of one or another part of the heart, focal changes, disturbances in the electrolyte balance, the nature and place of origin of the arrhythmia, etc.
Only in comparison with clinical symptoms and the system of treatment measures, with the nature of the ECG evolution - time shifts, in comparison with early ECGs, as well as with data from other instrumental and laboratory methods, can a clinical and electrocardiological conclusion be formed.
Additional leads help to correctly evaluate the ECG: the right extreme leads - to clarify the hypertrophy of the right ventricle, leads V7, V8, V9 allow us to identify changes in the basal sections of the lateral and posterior walls of the left ventricle, chest leads 2 ribs above allow us to identify changes in the high sections of the anterior wall, and 2 ribs below - true picture of pulmonary emphysema.
Taking an ECG, if necessary, during inhalation and exhalation allows you to avoid incorrect conclusions about focal changes in the lower wall.
ECG signs of abnormalities when you need to contact a cardiologist:
1. Rhythm disorders
Sinus arrhythmia - RR fluctuations more than 0.15 s.
Ectopic (heterotopic) cycles and rhythms, mainly not associated with a violation of automaticity.
Ventricular extrasystole is usually a complete compensatory pause, the QRS is widened, P is not associated with the QRS complex.
Supraventricular extrasystole is usually an incomplete compensatory pause, QRS identical to the previous one, P is associated with the QRS complex.
Atrial extrasystole is the premature, extraordinary appearance of the P wave and the following QRST complex. The presence of an incomplete compensatory pause.
Atrial tachycardia is a sudden onset and suddenly ending attack of heart rate up to 140-250 beats/min while maintaining the correct rhythm. The presence of a reduced, deformed, biphasic or negative P before each QRS.
Atrial flutter is a regular ectopic atrial rhythm with a frequency exceeding the level of supraventricular paroxysmal tachycardia - more than 220/min. With atrial flutter, an isoline is not visible between P waves, as with atrial tachycardia.
Atrial fibrillation is an uncoordinated excitation of individual fibers of the atrial myocardium. On the ECG, f waves with a number of contractions from 350 to 700 / min, RR intervals are different.
Ventricular tachycardia - when, during impulse formation in the His-Purkinje system, with a heart rate of 160-200/min, the QRS complexes are widened to 0.12 s or more, the RR is the same. The rhythm is generally regular. Irregularity is sometimes noted at the beginning and end of an attack.
2. Impaired conductivity function.
SA block is a violation of the conduction of electrical impulses from the sinus node to the atria.
More often, incomplete SA blockade occurs (periodic loss of individual cardiac cycles (P and QRST complexes). The increase in cardiac cycle pauses between two adjacent P or R waves is almost 2 times compared to the usual PP or RR intervals.
Atrioventricular block is a violation of the conduction of excitation impulses from the atria to the ventricles, AV is a first-degree block. A PQ prolongation of more than 0.20 each P wave is followed by an associated QRS complex.
AV block of the second degree - loss of QRS after Z. P:
- with a gradual increase in PQ - Mobitz 1;
- with stable PQ-Mobitz 2
AV block of the third degree - separation of the activity of the atria and ventricles. The PP interval (constant) is less than the RR interval (also constant).
The main signs of WPW syndrome are:
1.Shortening the P-Q® interval
2. The presence of an additional excitation wave in the QRS complex - ∆wave
ECG for ischemic damage and necrosis of the heart muscle.
- horizontal, obliquely downward directed, trough-shaped displacement of the ST segment by 1 mm. or more in one or more leads with a length of 0.08 mm/sec or more, lasting 1 minute.
- obliquely ascending decrease in the ST segment with a decrease in the j-point by more than 2 mm.
- ST segment elevation by 1 mm. and more in one or more leads.
The main ECG sign of cardiac muscle necrosis is a pathological Q wave (for non-transmural necrosis) or a QS complex (for transmural infarction).
The appearance of these pathological signs in chest leads V1-V2 and, less often, in leads I and AVL indicates necrosis of the anterior wall of the left ventricle.
The appearance of pathological Q or QS complex in leads III aVF and less often II is characteristic of myocardial infarction, posterior diaphragmatic (lower) parts of the left ventricle.
Pathological h. Q or QS complex in additional precordial leads V7-V9 indicates necrosis of the posterobasal or posterolateral sections of the left ventricle.
Thus, electrocardiography is indispensable in the diagnosis of rhythm and conduction disorders, ventricular and atrial hypertrophies, coronary heart disease, myocardial infarction and other heart diseases.
Be healthy!
Sign up for functional diagnostics
Functional diagnostics doctor - Miroshnichenko Elena Yurievna
You can make an appointment by calling (391) 218−35−13 or through your personal account
Basic methods for diagnosing cardiac conduction disorders
1. ECG (electrocardiogram)
A standard 12-lead ECG at rest can identify all the main types of cardiac conduction disorders: sinoatrial and atrioventricular block, bundle branch block. Drug tests in combination with ECG are almost never used at present.
2. Holter monitoring (monitoring) ECG
This type of study allows you to record an ECG for a day or more. It allows you to determine whether the patient has significant pauses (cardiac arrest). Pauses longer than 3 seconds are considered significant. If there are no significant pauses, installation of a pacemaker is almost never indicated.
3. Electrophysiological study of the heart (EPS)
This is the most reliable, but complex and expensive method for diagnosing arrhythmias. EPI is performed only in a hospital and requires the installation of several catheters in the veins of the arms and legs. Electrodes are inserted into the heart through these catheters and cardiac stimulation is performed—arrhythmias are caused and eliminated, and their parameters are examined.
To detect the most common types of cardiac conduction disorders, there is a simpler type of EPI - transesophageal EPI. In this case, a thin wire (probe-electrode) is inserted through the mouth or nose into the esophagus and the left atrium is stimulated through it. This type of study is performed on an outpatient basis. In particular, transesophageal EPI makes it possible to determine how long after cessation of stimulation the function of the sinus node (that is, its own pacemaker) is restored - this is necessary in order to make a diagnosis of sick sinus syndrome, one of the most common types of conduction disorders in the elderly.
Certain types of blockades
Atrioventricular (AV) block
There are 1st, 2nd and 3rd degree AV blocks. 1st degree AV block does not manifest itself clinically; the diagnosis is made by ECG (when the PQ interval on the ECG exceeds 0.20 seconds). 1st degree AV block often occurs normally, for example in athletes. Some drugs are contraindicated in this case, which can lead to higher degrees of AV block.
With 2nd degree AV block, loss of individual heart contractions is observed. There are two types of 2nd degree AV block, called Mobitz I and Mobitz II. Mobitz type I block is more benign in nature; implantation of a pacemaker is almost never indicated for it. Mobitz type II AV block indicates more serious damage to the cardiac conduction system and is sometimes treated with a pacemaker due to the risk of complete AV block.
3rd degree AV block is complete AV block. Impulses from the atria to the ventricles are not conducted, the ventricles work due to the fact that the AV node generates its own impulses, their frequency, however, is lower than that which the sinus node is capable of creating, and this rhythm is generally less reliable. Therefore, complete AV block, even asymptomatic, is often an indication for the installation of a pacemaker.
Bundle branch blocks
Bundle branch blocks are also diagnosed by ECG. Incomplete blockade of the right bundle branch is a normal variant. Of all the variety of bundle branch blocks, only complete blockade of the left bundle branch deserves special attention. Firstly, it may indicate an anterior myocardial infarction; secondly, it itself leads to asynchronous (non-simultaneous) contraction of the walls of the left ventricle and can lead to heart failure. In recent years, a special type of cardiac pacing has been developed; it is called biventricular (two-ventricular) cardiac pacing (see below).
Sick sinus syndrome
This disease of the conduction system of the heart usually occurs in older people. It is manifested by fainting and pre-syncope (often during physical activity), and the so-called tachy-brady syndrome: a rare pulse is replaced by a frequent one when the patient experiences atrial fibrillation. At the same time, it is difficult to treat atrial fibrillation itself (atrial fibrillation), since most antiarrhythmic drugs slow down the heart rhythm. For sick sinus syndrome, pacemaker implantation is indicated.
HAT Medicine
Case from practice.
When I was about 36 years old, I returned from visiting, where I drank a little. The mood was good. But I felt some kind of inner excitement. I don’t know what it was connected with. Suddenly, atrial fibrillation suddenly appeared. It did not go away and lasted about an hour, after which I decided to call an ambulance. I was given an injection of Novocainamide intravenously, after which the rhythm was restored right during the injection. I did not carry out any further special treatment. There were no rhythm disturbances. Subsequently, once or twice more I experienced atrial fibrillation, which lasted 10 and 40 minutes. Extrasystoles appeared very rarely. At one time they occurred when moving to a horizontal position during sleep, but then quickly passed.
They usually arose in cases where the activity of clinical attractors was observed in the gastric attractor. Since these were sporadic cases, I did not carry out specific NAT treatment for myself. I just strengthened my relaxation techniques at this time. Often walking around the room, I relaxed my fingers, my hands themselves. I paid special attention to relaxation in the esophagus area. To do this, taking a small sip of warm water, I imagined how the water passes through the esophagus, causing it to relax. At the same time, the diaphragm also relaxed. If you belch after this, then this is evidence of good relaxation.
Irregular heart rhythm (arrhythmia)
Irregular heartbeat is an arrhythmia. Your heart rate may also be irregular. The normal heart rate is from 50 to 100 beats per minute. Arrhythmia and abnormal heart rate do not necessarily occur simultaneously. Arrhythmia can occur against a background of a normal heart rate or even a slow rate (called bradyarrhythmia - less than 60 beats per minute). Arrhythmia can also occur against the background of an accelerated heart rate (called tachyarrhythmia - more than 100 beats per minute). In the United States, more than 850,000 people are hospitalized each year due to arrhythmias.
What causes arrhythmia?.
Arrhythmia can occur due to many different factors, including the following (common beliefs):
- Cardiac ischemia.
- An imbalance of electrolytes in your blood (such as sodium or potassium).
- Changes in your heart muscle.
- Damage due to cardiac risk.
- Recovery processes after heart surgery.
- Abnormal heart rhythms can also occur in a “normal healthy” heart.
The cause of arrhythmia from the perspective of HAT medicine.
Although it seems to us that our heart rate is rhythmic, this is not entirely true. If we determine the heart rate not per minute, but at another longer time interval, we will notice that the rhythm is not rhythmic. It is known that sinus arrhythmia in young people is associated with breathing and is completely normal. When you inhale, the heartbeat increases, and when you exhale, it decreases. Sinus arrhythmia decreases with age but persists in healthy hearts. These are manifestations of healthy chaos. That is, normal ri. It is with this rhythm that the heart better adapts to various loads and better tolerates stress. In cases of severe heart disease (in the absence of arrhythmia as a disease), as scientists have shown, the pulse is very rhythmic and does not change for a long period of time. This is a poor prognostic symptom. According to the NAT system, arrhythmia occurs either when there is a violation of the gastrointestinal tract or the genitourinary tract. We haven't clearly decided on this yet. When we have more experience, we will be able to treat rhythm disturbances very quickly (not too advanced, of course). We don't do that yet.
What types of arrhythmias are there?
Extrasystoles Premature atrial contractions. These extrasystoles occur in the atria (upper chambers of the heart). They do not cause harm and do not require treatment.
Ventricular extrasystole . This is the most common type of arrhythmia and occurs in people with and without heart disease. We all feel those missed heartbeats sometimes. In some people, they occur due to stress, excess caffeine, nicotine, or too much exercise. But sometimes ventricular extrasystoles can occur due to heart disease or electrolyte imbalance. People who experience these episodes frequently and/or are bothered by associated symptoms should be evaluated by a cardiologist. However, for most people, ventricular premature beats do not cause harm and rarely require treatment.
Atrial fibrillation . This is a very common type of heart rhythm disorder in which the atria (upper chambers of the heart) contract abnormally.
Atrial fibrillation (atrial flutter ). This arrhythmia occurs due to the impulse circulating too quickly through the atrium. Atrial flutter is usually more orderly and regular than atrial fibrillation. It most often occurs in people with heart disease and in the first week after heart surgery. Also, flutter often turns into atrial fibrillation.
Paroxysmal supraventricular tachycardia (SVT) .
This is a rapid heart rate, most often regular and comes from the upper parts of the ventricles. Paroxysmal SVT occurs and ends suddenly. Ventricular tachycardia. The accelerated heart rate comes from the lower parts of the heart (ventricles).
It prevents the heart from filling adequately with blood, so the heart pumps less blood into the body. This arrhythmia can be severe, especially in people with heart disease, and may be associated with other symptoms. People with such arrhythmia should be seen by a cardiologist. Ventricular fibrillation. This is a continuous, disorganized flow of impulses from the ventricles. The ventricles flutter, as a result of which they cannot contract and pump blood throughout the body.
Ventricular fibrillation is a very serious complication of heart disease that can lead to death. Immediate defibrillation is required.
We have all heard about the sudden death of young people. These could be football players, boxers. In some cases, this happens because they receive a strong blow to the chest, where the left ventricle is located. They develop ventricular fibrillation. Only in 15% of cases is it possible to quickly defibrillate and save the person. They may have had a long QT symptom. QT is the area on the electrocardiogram (ECG) that reflects the time the heart muscle spends contracting and then recovering. Long QT syndrome is inherited. Heart block. Slowing or complete blocking of the passage of electrical impulses on the way from the sinoatrial node to the ventricles. The level where the impulse is slowed or blocked may be in the atrioventricular node or in the His-Purkinje system. In this case, the heart may beat irregularly and often at a slower rate. If the heart block is severe, then implantation of a pacemaker is necessary.
What are the symptoms of arrhythmias?
Ari and not show any symptoms. Your doctor can detect an irregular heartbeat by feeling your pulse during a physical examination or by examining an electrocardiogram (ECG). If symptoms occur, they may include:
- Palpitations (the feeling of the heart skipping beats, fluttering or tumbling in the chest, or the feeling that the heart is jumping out of the chest).
- Sensation of dull knocks in the chest.
- Dizziness or feeling of confusion.
- Fainting.
- Dyspnea.
- Discomfort in the chest.
- Weakness or fatigue (feeling very tired).
Treatment depends on the type and severity of your arrhythmia. Some people with arrhythmias do not need treatment. Others are treated with medications, lifestyle changes, and surgical procedures.
What medications are used to treat arrhythmias?
Antiarrhythmic drugs. These medications control your heart rate and include beta blockers. Anticoagulant or antiplatelet therapy. Drugs in this group reduce the risk of blood clots and stroke. These include warfarin (a "blood thinner") or aspirin. Because these medications work quite individually, it may take time to try several medications and find the dose that is optimal for you.
What lifestyle changes do I need to make?.
- If you notice that your irregular heart rhythm most often occurs during certain types of exercise, then try to avoid them.
- If you smoke, you should definitely quit smoking.
- Limit your consumption of alcohol and other microbial fermentation products (NAT diet).
- Limit your caffeine intake.
- Stay away from stimulants used for coughs and cold medications. Some of these medications contain substances that can cause abnormal heart rhythms.
- Naturally, physical exercise is necessary for prevention and treatment: walking.
- A special place should be given to relaxation. Normalize your sex life. An incorrect rhythm can provoke arrhythmia.
What is a pacemaker?
A pacemaker is a device that sends low-intensity electrical impulses to the heart muscle to maintain an adequate heart rate. Pacemakers are usually used to prevent the heart from beating too slowly. They consist of a generator (which contains batteries and a small computer) and a conduction system (wires) through which impulses travel from the pulse generator to the heart muscle. Electrical cardioversion, anti-tachycardia pacing, defibrillation, catheter ablation, and cardiac surgery are also used. We do not treat arrhythmias with HAT medicine.
Leave your comment
- Comments
Comments
- No comments found
Pinned
Liked
Pacemakers
Currently, there are many options for permanent pacing. They have one thing in common: under the skin of the anterior chest wall (usually near the collarbone) an electric pacemaker is implanted - a small metal box, the wires from which (electrodes) go through the veins to the right side of the heart. These wires sense the heart's own electrical activity (to synchronize their work with it) and transmit impulses to the heart. Modern pacemakers almost always stimulate both the atria and the ventricles. In addition, they are tuned so that the heart rate increases during exercise and decreases at rest. There are essentially no contraindications for cardiac pacing: pacemaker implantation is a simple and harmless procedure that can be performed at any age.
A separate type of cardiac pacing is the so-called biventricular stimulation. It is performed not for conduction disorders themselves, but to achieve synchronous contraction of all the walls of the left ventricle. Therefore, the installation of a biventricular stimulator is also called resynchronization therapy. Electrodes from the stimulator go to the right ventricle and to the coronary sinus (which is directly adjacent to the left ventricle). This type of treatment greatly helps some heart failure patients.
Some pacemakers also have a defibrillator function: they detect life-threatening arrhythmias and automatically deliver a shock to stop them.
Patients with pacemakers lead normal lives. They just need to avoid the influence of a strong magnetic field. Thus, magnetic resonance imaging (MRI) is contraindicated in patients with implanted pacemakers.
From time to time, patients with implanted pacemakers need to be seen by specialists: to check the serviceability of the stimulator (in particular, its battery capacity), and to adjust the stimulation parameters.
Share:
Heart rhythm disturbances (arrhythmias)
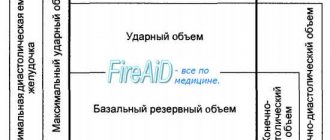
The heart is an incredibly complex organ. Its task is to collect the blood flowing to the heart through the veins and throw this blood into the arteries so that all cells of the body receive their share of nutrients and oxygen. Reacting to an increase in the nutritional needs of any organ or the whole organism, it increases the release of blood into the arteries. The heart consists of four chambers - two atria and two ventricles. In a healthy heart, the atria contract first, expelling the blood that entered them from the veins. Blood enters the ventricles of the heart. Contraction of the ventricles (systole) pushes blood into the arteries. In the right atrium, blood collects from the veins of the whole body, then it enters the right ventricle, from there it is released into the arteries of the lungs. In the lungs, the blood is enriched with oxygen, gives off carbon dioxide and is collected in the pulmonary veins. From there, the blood enters the left atrium, then into the left ventricle, and from there into the arteries of the body. The coordination of the heart is ensured by a special conduction system of the heart. These are specialized cells that produce and conduct electrical impulses that direct the coordinated contraction of the heart muscle. The impulse that triggers the contraction of the heart is produced in the right atrium, in the so-called sinus node (pacemaker). It is this node that is responsible for the fact that the heart contracts at a frequency of 60-90 beats per minute. The signal then spreads to the remaining atria, causing them to contract, and then to the ventricles. Disturbances in this system lead to heart rhythm disturbances (arrhythmias).
What are the types of arrhythmias?
Heart contractions follow each other at regular intervals. If this sequence is disrupted, the patient is said to have an arrhythmia. Depending on where the disturbances occur, all arrhythmias are divided into atrial (or supraventricular) and ventricular. Arrhythmia is not an independent disease, but a sign (symptom) of some disease. Therefore, the occurrence of arrhythmia requires mandatory examination by a cardiologist. The patient can detect the presence of arrhythmia himself. To do this, you need to learn to find and count the pulse.
Heart function (rhythms)
If the pulse rate exceeds 90 beats per minute, they speak of tachycardia. The heart rate may increase during physical or emotional stress (this is a normal reaction of a healthy heart). An increase in body temperature causes tachycardia. It is believed that an increase in body temperature by 1 degree leads to an increase in heart rate by 10 beats. Tachycardia can be a sign of many diseases, but it can also be a normal variant. Some types of tachycardia require special antiarrhythmic treatment. If the pulse rate is less than 60 beats per minute, they speak of bradycardia. Bradycardia can occur in absolutely healthy people. It is usually observed in athletes. Moderate bradycardia creates favorable conditions for the blood supply to the heart muscle. This is due to the fact that blood can only flow to it when it is in a state of relaxation (i.e. between contractions). The faster the rhythm, the more blood is needed to replenish the energy costs of the heart muscle, and the relaxation period becomes shorter. Therefore, some medications (for example, atenolol or anaprilin) that can slow down the rhythm (extend the period of relaxation) improve blood supply to the heart muscle. If bradycardia appears suddenly, if the slowdown in rhythm is accompanied by dizziness or loss of consciousness, consult a doctor immediately. You should also consult a doctor if your heart rate is less than 50 per minute and there are no other unfavorable signs. In some forms of bradycardia, it is necessary to implant a special device - a pacemaker. This device takes over control of the heart rhythm when its own pacemaker (sinus node) fails to cope with its task.
Extrasystole
If a premature contraction is woven into the correct rhythm of heart contractions, they speak of extrasystole. According to the place from which the electrical impulse emanates, leading to premature contraction, all extrasystoles are divided into atrial and ventricular. Even an absolutely healthy person can experience extrasystoles several times a day. However, their appearance is a reason to consult a cardiologist. Like all arrhythmias, extrasystole is not an independent disease, but only a sign of some disease. The examination will be aimed at finding the cause of the arrhythmia. Atrial fibrillation is the most common arrhythmia
What is atrial fibrillation
Atrial fibrillation is a type of rhythm disorder in which the atria are excluded from the coordinated work of the heart. An electrical impulse runs at high frequency through the atria, causing chaotic contraction of muscle fibers (fibrillation). Therefore, atrial fibrillation is also sometimes called atrial fibrillation. Some impulses break through to the ventricles, which contract due to this in an incorrect, irregular rhythm. The absence of the correct rhythm is the main sign of atrial fibrillation. Sometimes it is not possible to identify the cause of atrial fibrillation, then they talk about its idiopathic form. Most often, atrial fibrillation is a sign of heart disease, coronary heart disease, arterial hypertension, etc. Not only cardiovascular diseases can lead to atrial fibrillation. Common causes include diseases of the thyroid gland, lungs, acute and chronic poisoning (for example, alcohol) and many other diseases. It is important that for success in the treatment of atrial fibrillation, it is necessary not only to correctly prescribe special antiarrhythmic drugs, but also to correct its cause.
Manifestations (symptoms) of atrial fibrillation
The most common manifestation of atrial fibrillation is a feeling of palpitations. It is due to the fact that the average ventricular rhythm during atrial fibrillation usually increases and can reach 130-150 beats per minute. Interruptions in the functioning of the heart are often felt, sometimes a sharp feeling of lack of air, pain in the heart area, and dizziness. Approximately 1 in 10 patients does not feel the appearance of atrial fibrillation at all.
Types of atrial fibrillation
Long-term atrial fibrillation is called permanent. If it occurs paroxysmally, they speak of the paroxysmal form. Atrial fibrillation with a high heart rate is called tachysystolic, with a normal frequency - normosystolic and with a low frequency - bradysystolic form.
Is it necessary to treat atrial fibrillation?
According to various estimates, from 1.5 to 5% of humanity suffers from this type of arrhythmia. This is the most common type of arrhythmia requiring treatment. The appearance of atrial fibrillation (if left untreated) significantly (5-7 times) increases the risk of stroke and pulmonary embolism. The likelihood of developing heart failure also increases. Additional factors such as age and the presence of severe concomitant diseases further increase the risk of stroke and heart failure in patients with atrial fibrillation. Therefore, atrial fibrillation must be treated without fail.
Restoring the correct heart rhythm
The goal of treatment for a patient suffering from atrial fibrillation is, if possible, the restoration of the sinus (correct) heart rhythm and its subsequent maintenance. There are several ways to restore the correct rhythm. The first - the simplest - can be tried by the patient himself. The method is based on the possibility of stimulating the vagus, a nerve that slows down the heart rate. You need to take a deep breath. Then hold your nose and mouth tightly and try to exhale forcefully. This method can also stop other attacks of palpitations. Unfortunately, this method does not help all patients. The most common is restoring the heart rhythm with the help of medications. These medications are called antiarrhythmics. Typically, medications are administered intravenously. However, in some cases, the patient himself can take a previously selected medicine, which stops the attack of atrial fibrillation. Unfortunately, there are no special signs to determine which medicine will be more effective. In practice, you have to try several medications before choosing the drug that is most suitable for the patient. In some cases, when an attack of atrial fibrillation cannot be treated with medications, if it has existed for a long time, there is an immediate threat to the patient’s life, so-called electrical cardioversion is used to restore the rhythm. The patient falls asleep for a short time (1-2 minutes), then a special synchronized (i.e. applied at a certain phase of the cardiac cycle) electric current discharge restores the heart rhythm. The method has several disadvantages - the need to put the patient to sleep, the need for special equipment to carry out the procedure. In addition, this procedure must be performed in a hospital that has highly trained personnel. But there are also significant advantages. Thus, the rhythm is restored in almost all cases (unlike drugs, which restore the rhythm only in 60-80%). This method is the safest, since any medicine has side effects. If they appear, then it takes time for the medicine to leave the blood. Taking these advantages into account, special devices sewn under the skin - cardioverters - were created that detect atrial fibrillation and stop it. However, these devices are not yet widely used. After the rhythm is restored, it is necessary to maintain it. It is necessary to treat the disease that led to atrial fibrillation and eliminate the factors that provoke the attack. If attacks are rare, then sometimes special antiarrhythmic therapy is abstained. However, most often you have to take medicine to prevent the attack from developing. Sometimes, for frequent attacks that are difficult for patients to tolerate, surgical treatment has to be used.
Maintaining a normal heart rate when rhythm cannot be restored
In some cases, it is necessary to refuse to restore the normal rhythm. Usually in this case the patient has a so-called permanent form of atrial fibrillation. The main therapeutic measures are to maintain a normal heart rate and prevent complications.
Prevention of complications of atrial fibrillation
Since the main complications of atrial fibrillation are stroke and heart failure, their prevention should also be carried out in a patient with atrial fibrillation. The method of such prevention is chosen by your doctor.
Recommendations for a patient with atrial fibrillation
Try to find out and tell your doctor what precedes the next attack of atrial fibrillation. This may be unusual physical activity, increased blood pressure, taking any medications, drinking alcohol, exacerbation of lung disease, etc. Learn to count your pulse (or ask your doctor to teach you) and recognize whether you have atrial fibrillation or whether your heart rhythm is correct. If the attack does not go away on its own within 2-3 hours, does not go away with regular medications, or causes discomfort, pain, or shortness of breath, consult a doctor. The sooner from the moment the attack begins to treat it, the easier it is to restore the correct rhythm. Be sure to have your latest (or several recent) electrocardiograms with you. They may be needed for comparison in an emergency. Do not rely on your memory; have a sheet of paper with you with the name and dosage of the medications you are taking. This may be very important if you are being given a new medicine because many of the substances interact with each other. If you are taking phenylin or syncumar - medications that reduce prothrombin levels and prevent stroke and thromboembolism - do not forget to consult your doctor if:
- signs of bleeding appeared (nosebleeds, blood on the gums when biting, bruises began to appear)
- if you start taking new medications or change the dosage of previously taken medications
- if the diet has changed (for example, a new season has begun)
- if you have a cold, if you have an upset stomach, or any new illness. If you are planning any surgery or tooth extraction, tell your doctor that you are taking these medications.
Examination of a patient with arrhythmias
In order to properly treat arrhythmia, it is necessary to undergo a special examination. It consists of two parts. The first is the identification of the arrhythmia itself, the conditions for its occurrence and cessation. The second is the search for the disease that led to the arrhythmia. To detect an arrhythmia, it must be registered. To do this, an electrocardiogram is recorded. The desired arrhythmia is not always detected on a regular ECG. Therefore, the next step is to record an electrocardiogram over a long period of time (usually a day), then, using a special computer, the recording is deciphered. This examination method is called 24-hour Holter ECG monitoring. In some clinics, patients are given special devices to take home that allow them to transmit an ECG to their doctor if necessary. This method also allows you to record rare rhythm disturbances. Physical activity often provokes arrhythmias, so exercise testing is sometimes used to measure the level of acceptable physical activity and evaluate the preventive effect of antiarrhythmic drugs.