Reasons for the blockade
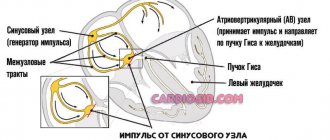
The human heart beats as a result of electrical impulses that regulate the sequence and frequency of contractions of the chambers of the heart.
Electrical impulses are generated in the sinus node, a structure located in the upper chamber of the heart - the atrium. From the sinus node, impulses propagate down to the ventricles at a certain frequency, thereby setting the heart rate. If, for some reason, the impulses slow down or are blocked, a disease develops - heart block (atrioventricular block).
Heart block is a disease in which a person’s heart contracts with an abnormal frequency and rhythm due to disruption of the conduction system of the heart. As a result of blockades, arrhythmia or other, more serious diseases may develop.
Place of manifestation
Intraventricular block can occur anywhere in the ventricles. Therefore, the resulting disorders are divided into nonspecific and bundle block. Each of these subtypes has its own ECG criteria.
It is noteworthy that intraventricular block can develop even in an absolutely healthy person, without affecting his well-being in any way. But this is still considered conduction disorders along the right branch. When registering the left hemiblock, as well as with a two- or three-fascicle blockade of the terminal branches, it is generally accepted that some kind of cardiac pathology is present.
Classification
There are several types of heart block. They are divided based on the location of the area where the conduction function of the heart is difficult or completely blocked. Due to the development of the disease in different parts of the heart, each blockade has its own characteristic features.
Photo: psodaz / freepik.com
Sinoatrial blockade
Sinoatrial block or sick sinus syndrome (SSNS) develops as a result of complete or partial dysfunction of the sinus node. This can occur both as a result of physiological disorders and due to other factors not related to the state of the body (extracardiac factors).
The main cause of SSSS can be considered fibrosis (development of connective tissue and its scarring) of the sinus node tissue. This pathology can be caused by inflammatory processes, increased tone of the vagal nerve, or taking medications.
SSSU can manifest itself:
- shortness of breath;
- general weakness of the body;
- pain in the heart;
- dizziness and loss of consciousness;
- low blood pressure;
- arrhythmia.
Interatrial block
Interatrial block develops when the propagation of electrical impulses is disrupted, both within and between the atria. The propagation of excitation occurs along special conduction pathways, which are circular and longitudinal muscle bundles, usually not described as part of the specialized conduction system of the heart.
One of the mechanisms of changes in the electrophysiological properties of the atrial myocardium, leading to a slowdown in conduction, is the development of fibrosis. There is a violation of the integrity of myocardial cells with the deposition of collagen in the intercellular space, which prevents the movement of impulses throughout the heart.
Accompanied by general weakness, pain in the chest and abnormal heart rate.
Atrioventricular block
Atrioventricular (AV) block is a partial or complete interruption of the transmission of impulses from the atria to the ventricles, leading to disturbances in heart rate and blood flow rate.
There are 3 types of atrioventricular block:
- 1st degree - due to a slow transition of impulses from the atria to the ventricles;
- 2nd degree - characterized by blocking of some impulses;
- 3rd degree - (complete atrioventricular block), associated with blocking of all impulses coming from the atria to the ventricles.
It occurs due to damage to the most sensitive area of the conduction system of the heart - the atrioventricular junction.
Intraventricular block
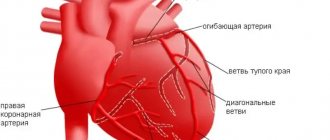
Intraventricular block occurs when the His bundle, the conducting region of the heart located in the region of the ventricles, is disrupted. The bundle of His consists of 3 branches: the left and right anterior branches and the posterior branch. The posterior branch is also divided into right and left.
Figure 1. Differences in ECG readings with normal rhythm and with blockades.
Intraventricular block is classified based on damage to 1 of 3 branches:
- Blocking of the anterior right branch - the innervation of the right ventricle is disrupted;
- Blocking of the anterior left branch - in case of disruption of the innervation of the left ventricle;
- Blocking of the posterior branch - the work of the His bundle is disrupted to the greatest extent, since along this branch impulses go from the atria to the ventricles, and are subsequently divided into right and left;
- Three-bundle block is associated with disruption of the conduction of the entire His bundle.
Signs on ECG
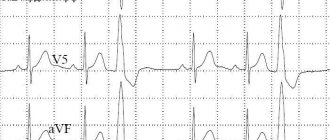
The disease is detected in a patient after he undergoes electrocardiography.
When deciphered, the main sign that indicates an existing pathology is the QRS complex, which characterizes the functioning of the ventricles. Thanks to the ECG, the main disturbances in the rhythm of the ventricles are identified: inhibition or interruption of conduction, blocking of the re-entry of an impulse or acceleration of conduction. Each pathology has its own development mechanism and features visible on the electrocardiogram.
The main signs of the development of pathology on the electrocardiogram:
- Changes in the QRS complex: in the case of incomplete blockade, the width is 0.1-0.12 s, if the blockade is complete, it increases - 0.12 s or more.
- Abnormalities in the right leg - the R wave in the chest leads is split, the ST segment and the T wave change their direction.
- Complete blockade of the left leg - in the 5th and 6th thoracic leads the R wave expands, in the 1st-3rd leads the R and S waves decrease or are completely absent.
- Blockade of the anterior branch of the left leg is characterized by deviation of the electrical axis to the left side, the width of the QRS complexes is less than 0.1 s. In the 2nd and 3rd chest leads, enlarged S and reduced R waves are visible.
- A disorder in the posterior branch is characterized by deviation of the electrical axis to the right, QRS complexes less than 0.1 s. In the 2nd and 3rd chest leads, enlarged R and reduced Q waves are visible. Violation of intraventricular conduction on the ECG
- With paroxysmal tachycardia (accelerated contraction of the ventricles), changes are visible on the ECG - the S or R waves are directed in one direction, the electrical axis is tilted to the left, the QRS complexes are increased to 0.14-0.16 s.
- Trifascicular block is characterized by varying durations of PQ intervals. Often there is atrial fibrillation or a complete stop of contractions.
- Ventricular fibrillation presents in a chaotic rhythm.
An important indicator is the time during which the impulse travels the entire path (from the sinus node to the ventricles). The rate of passage of one pulse is 0.07-0.09 s.
Degrees and their symptoms
Heart blocks are classified not only by the place of its development, but also by the degree of severity, which reflects the danger of the disease to human health and approaches to treating a particular stage of heart block. There are three main stages of heart block
First degree heart block
The first degree is the mildest form of manifestation. There is a delay of a fraction of a second in the time required for electrical impulses to travel through the atrioventricular junction. Complete blocking does not occur and the impulses reach the desired point.
First-degree heart block usually does not cause any noticeable symptoms and is diagnosed by examining other medical conditions in the person. Treatment may be limited to eliminating risk factors that affect heart health.
Second degree heart block
As the second degree develops, there is a series of increasing delays in the time it takes for the atrioventricular junction to conduct an impulse into the ventricles until the heart beat is missed. Partial blocking of impulses is possible.
The second degree is divided into 2 types:
- The first type of Mobitz. This is a less serious type of second-degree heart block. Characterized by slow conduction of impulses. May cause symptoms of mild dizziness and weakness. Usually does not require treatment.
- Mobitz's second type. Electrical signals reach the ventricles slowly or may be completely blocked. This type of heart block can often progress to third degree heart block. May cause symptoms of dizziness and fainting, accompanied by bradycardia. Requires medical consultation and full treatment.
Third degree heart block
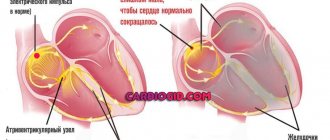
Third degree heart block is the most dangerous degree for a person’s health and life and requires immediate medical attention. It is characterized by complete blocking of the transmission of electrical impulses from the atria to the ventricles due to the lack of communication between the atrioventricular junction and the ventricles.
In this case, the ventricles can partially take over the function of a pacemaker, but they are not able to ensure full functioning of the heart.
Third degree blocks can be congenital or acquired as a result of other heart diseases or injuries.
Symptoms include:
- shortness of breath;
- weakness;
- fainting conditions;
- chest pain;
- pale skin, spots;
- arrhythmia.
Many cases of third-degree congenital heart block are diagnosed during pregnancy because ultrasound scans can often determine whether the baby has bradycardia.
Important! If the diagnosis is missed during pregnancy, symptoms of third-degree congenital heart block usually do not appear until the baby is older and his heart is more developed.
Diagnostics
Diagnosis of heart block begins with an interview and physical examination of the patient. Medical history and family history are studied. The patient's symptoms and lifestyle are examined. Medicines that the patient may have taken are checked.
Testing is carried out using a Holter or event monitor - devices that track heart rhythm over a certain period of time.
Figure 2. Signs of heart block.
A Holter monitor is used to study the heart over 24 or 48 hours. Event monitor - for a month or more. They allow changes in heart rate to be recorded even if they do not occur frequently or predictably.
An implantable loop recorder, a small heartbeat recorder that is placed under the skin over the heart, may be used. Capable of analyzing heart function for up to 2 years.
Basic methods of studying the functioning of the heart are used, such as electrocardiography (ECG) and electrophysiological studies. To diagnose heart diseases of a child in the womb, the ultrasound method is used.
Holter monitor. Photo: yupachingping / freepik.com
Intraventricular block - diagnosis in Germany
The following methods are used to diagnose intraventricular blockades in Germany:
- Electrocardiogram . Allows you to notice the presence of a blockade and determine from the characteristic “pattern” of the cardiogram what kind of blockade is taking place.
- Holter monitoring . Used to diagnose non-permanent blockades.
- Ultrasound of the heart . Allows you to determine the condition of various parts of the heart, to find out whether there are pathologies of the heart valves.
Heart surgeries in Germany
Treatment
When diagnosing first-degree heart block and first-degree Mobitz block, treatment as such is not necessary. These types of blockades do not pose any serious danger. The doctor may advise you to lead a healthy and active lifestyle, with moderate physical activity, and give up bad habits such as smoking and drinking alcohol.
When diagnosing Mobitz block of the second type and block of the 3rd degree, the patient needs medical attention, since the lack of treatment can lead to death.
The main treatment method for these types of blockades is the installation of a pacemaker. This device is surgically placed near the heart and monitors the correct frequency and rate of generation of electrical impulses.
Pacemaker. Photo: PantherMediaSeller / Depositphotos
Characteristic symptoms of intraventricular blockades
Very often, intraventricular block does not cause any symptoms and is detected during a cardiac examination of the heart.
Nonspecific, frequently occurring symptoms may include fatigue and fatigue. In addition, the patient may experience a feeling of a sinking heart or a loss of heartbeat.
With complete blockades, bradycardia appears. With distal complete blockade, heart failure may develop and there is a risk of sudden death.
Forecast
Heart block can be congenital) but most often develops after birth. In general, the risk of acquired heart block increases with age, as does the incidence of cardiovascular disease.
First-degree heart block is common in well-trained athletes, adolescents, young adults, and individuals with a highly active vagus nerve. People with various heart conditions, including coronary artery disease, rheumatic heart disease, sarcoidosis, or other structural heart disease, are also at risk of developing first-degree heart block.
Without proper treatment, second-degree Mobitz blocks and third-degree blocks can be accompanied by symptoms that significantly impair the quality of life: constant fatigue, chest pain, severe dizziness and fainting. Without treatment, complete cardiac arrest can result.