Blood pressure measurement: a method that has stood the test of time
Maintaining
There are very few research methods that have stood the test of time. As a rule, one method, on which great diagnostic hopes were pinned, is replaced by another, more modern and informative, relegating its predecessor to the background. In 1905, at a meeting of the Imperial Military Medical Academy, Russian surgeon and scientist N.S. Korotkov gave a report in which he described the sound method for determining blood pressure (BP) using the Riva-Rocci manometer. Biographers N.S. Korotkov note that the essence of his discovery, which became a milestone in the history of clinical medicine, was outlined in less than a page of text in the News of the Imperial Military Medical Academy in St. Petersburg. Nevertheless, initially the development of a new method was not the goal of N.S.’s scientific research. Korotkova. At the Military Medical Academy, he carried out experimental work on the study of collateral blood circulation and in the process of research, using a phonendoscope, he listened to successively changing sounds over the peripheral arteries under conditions of their compression. Nikolai Sergeevich found that if you place a Riva-Rocci cuff on the shoulder and increase the pressure in it until the pulse disappears in the radial artery, then no sounds are heard in the distal segment of the brachial artery; but then, if you gradually reduce the pressure in the cuff, tones are first heard in the same place, then noises, then again loud tones, the intensity of which decreases, and finally all sounds in the brachial artery completely disappear. To evaluate the diagnostic value of the proposed method and the prospects for its use in clinical practice N.S. Korotkov was helped by Professor of the Department of Diagnostics and General Therapy M.V. Yanovsky, under whose leadership the research of N.S. Korotkov’s studies were completed, which made it possible to develop a modern method for measuring blood pressure [1]. The first direct (bloody) measurement of blood pressure was made in a horse in 1733 by the philosopher and inventor, and according to other sources, monk, Stephen Hales [2]. The experimenter inserted a brass tube into the left femoral artery of the animal, which was connected to a glass tube installed vertically. After removing the clamp from the artery, the height of the blood column in the glass tube reached 8–9 feet, and fluctuations in its level appeared synchronous with heart contractions [3]. The great scientist I.P. Pavlov, the first Russian Nobel laureate, wrote: “Science moves in impulses, depending on the successes achieved by the methodology. With each step of the methodology forward, we seem to rise a step higher, from which a wider horizon opens up to us, with previously invisible objects.” Since its introduction into clinical practice to the present day, the Korotkoff method has been the only official method of non-invasive blood pressure measurement, approved in 1935 by the World Health Organization.
Diagnosis of arterial hypertension
It is this method that serves as the basis for diagnosing arterial hypertension (AH). In accordance with national clinical guidelines, in patients with a newly detected increase in blood pressure, the diagnosis of hypertension is established based on at least twice the blood pressure measurements at different visits [4]. The value of this clinical blood pressure allows not only to diagnose hypertension, but also to stratify the risk of cardiovascular complications. Other research methods used for hypertension (24-hour blood pressure monitoring, echocardiography, duplex scanning of the brachiocephalic arteries, determination of pulse wave velocity and many others) provide important additional information about the nature of hypertension, possible damage to target organs, but, as noted above, are not fundamental for establishing a diagnosis of hypertension in a patient. The classification of blood pressure levels assumes the existence of several levels of normal blood pressure, 3 degrees of its increase (according to systolic - SBP and diastolic - DBP pressure), as well as the identification of isolated systolic hypertension (ISAH). The modern classification of blood pressure levels is shown in Table 1 [5, 6].
Requirements for blood pressure measurement
Considering that the method for determining blood pressure according to Korotkov is not without subjective aspects, and blood pressure itself is a very labile constant that changes under the influence of various external factors, a number of mandatory requirements are imposed on the simple procedure for measuring blood pressure. Blood pressure measurement is carried out while sitting in a position comfortable for the patient, the hand is placed on the table at the level of the heart; The cuff is placed on the shoulder, its lower edge 2 cm above the elbow. Avoid drinking coffee and strong tea for 1 hour before the test; smoking is not recommended for 30 minutes before measuring blood pressure; the use of sympathomimetics, including nasal and eye drops, is discontinued. Blood pressure is measured at rest after a 5-minute rest; if the procedure for measuring blood pressure was preceded by significant physical or emotional stress, the rest period should be extended to 15–30 minutes. The size of the cuff should correspond to the size of the arm: the rubber inflating part of the cuff should cover at least 80% of the circumference of the shoulder. The following cuff sizes are recommended: for a shoulder with a circumference of 27–34 cm - cuff 13x30 cm; for a shoulder with a circumference of 35–44 cm - cuff 16x38 cm; for a shoulder with a circumference of 45–52 cm - a cuff of 20x42 cm. Thus, for many obese patients, standard size cuffs may not be sufficient to obtain reliable blood pressure measurement results. The mercury column or pressure gauge needle must be at zero before starting the measurement. To determine the blood pressure level, at least two measurements should be taken with an interval of at least 1 minute on each arm; with a difference in blood pressure>5 mm Hg. Art. make an additional measurement; The average value of 2–3 measurements is taken as the final blood pressure value. In elderly people, patients with diabetes, and patients with other conditions that may be accompanied by orthostatic hypotension, it is advisable to measure blood pressure 1 and 3 minutes after standing (orthostasis). The cuff is inflated to a pressure level that exceeds the SBP by 20 mm Hg. Art. (assessed by the disappearance of the pulse). The pressure in the cuff should be reduced slowly, at a rate of 2 mmHg. Art. in 1 s. The blood pressure level at which the 1st tone appears corresponds to SBP (1st phase of Korotkoff sounds), the pressure level at which the disappearance of tones occurs (5th phase of Korotkoff sounds) corresponds to DBP. During the initial examination of the patient, the pressure in both arms should be measured; further measurements are carried out on the arm on which the blood pressure is higher. All these requirements for measuring blood pressure are, of course, well known, but it should be emphasized that negligence in fulfilling one or more requirements can lead to a significant distortion of real blood pressure values, and consequently to under- or over-diagnosis of hypertension. Thus, an incorrectly sized cuff can distort the true blood pressure figures by an average of 5–8 mm Hg. Art., measuring blood pressure in a cold room - by 8–10 mm Hg. Art. (due to peripheral vasoconstriction), and drinking coffee or smoking immediately before measurement - by 10 mm Hg. Art. Undoubtedly, the correct technical implementation of the technique itself plays an important role in measuring blood pressure. Sound phenomena heard during cuff decompression, N.S. Korotkov divided it into 5 phases. The first phase begins with the appearance of faint sounds, which become clearer and more intense as the cuff deflates. The first of at least two consecutive sounds corresponds to SAD. The next, 2nd phase, is accompanied by the appearance of noise and a “russling” sound as the cuff is further deflated; The 3rd phase corresponds to the period during which the sound resembles a crunching sound and increases in intensity; during the 4th phase a soft “blowing” sound appears; The 5th phase is characterized by the disappearance of the last tone. Accordingly, the blood pressure level at which the first distinct tone appears (1st phase of Korotkoff sounds) corresponds to SBP, and the pressure level at which the disappearance of tones occurs (5th phase of Korotkoff sounds) corresponds to DBP. In clinical practice, there are special situations when measuring blood pressure. These include: the absence of the 5th phase of Korotkoff sounds - the phenomenon of “infinite tone” (observed with high cardiac output: in children, with thyrotoxicosis, fever, aortic insufficiency, in pregnant women. Korotkoff sounds are heard until the zero division of the sphygmomanometer scale). In these cases, the beginning of the 4th phase of Korotkoff sounds is taken as DBP; auscultative failure - a period of temporary absence of sound between the 1st and 2nd phases of Korotkoff sounds (can last up to 40 mm Hg, observed with high systolic blood pressure). A doctor may also encounter a special situation when measuring blood pressure in the elderly, since with age there is an increase in the rigidity of the walls of the arteries, including the brachial artery. To achieve compression of a stiff artery, a higher (above intra-arterial) level of pressure in the cuff is required, which may result in a false increase in blood pressure (pseudohypertension). The issue of measuring blood pressure in patients with atrial fibrillation remains complex and unresolved.
Classification and diagnosis of hypertension in the light of modern recommendations
It would seem that the main issues related to the measurement of blood pressure and the gradation of its levels have been clearly worked out for decades and cannot be a reason for discussion. However, a peculiar sensation was the revision of blood pressure levels carried out in 2021 by the American College of Cardiology and the American Heart Association (ACC/AHA). According to the proposed ACC/AHA classification, SBP in the range of 120–129 mmHg is considered elevated. Art., and stage I hypertension is established when SBP is 130–139 mm Hg. Art. and/or DBP 80–89 mm Hg. Art. The European Congresses, where the updated recommendations of the European Society of Cardiology and the European Society of Arterial Hypertension were expected to be presented and discussed, were supposed to take place later in 2021, so from 2021 it remained an open question whether the European community would accept the American approach to grading blood pressure levels. However, European cardiologists have retained the same view on the classification of blood pressure levels, which is reflected in the European recommendations of 2021. The same classification, presented in the national recommendations (2013), is also used in Russian clinical practice. The currently actively discussed European recommendations, having not undergone radical changes compared to the previous edition, nevertheless contain a number of updated positions and clarifying points. Commenting on the recommendations for the management of arterial hypertension of the European Society of Cardiology and the European Society of Arterial Hypertension 2021, leading Russian cardiologists draw attention to the following points [7]. It is noted that the diagnosis of hypertension is still based on data from clinical measurements of blood pressure (IC), however, a more clear algorithm for screening and diagnosing hypertension is proposed, in which, depending on the level of blood pressure, the frequency of its measurement in the traditional way or the need for 24-hour blood pressure monitoring is determined ( ABPM) or self-monitoring of blood pressure (SBP), in particular to identify hidden hypertension and confirm its diagnosis. The algorithm for screening and diagnosing hypertension is shown in Figure 1.
In the context of the 2021 European recommendations, one cannot fail to mention some revision of the approach to determining target blood pressure levels: the primary goal is still to achieve a blood pressure level of less than 140/90 mmHg. Art. in all patients (level of evidence IA). If therapy is well tolerated, it is recommended to reduce blood pressure to 130/80 mmHg. Art. or lower in most patients (IA). A target DBP level should be considered below 80 mm Hg. Art. in all patients with hypertension, regardless of the level of risk or comorbid conditions (II AB). However, as follows from the recommendations, the same blood pressure level cannot be applied to all patients with hypertension. Differences in target SBP levels are determined by patient age and comorbid conditions. A new provision that is important for real clinical practice is the designation of the level below which blood pressure should not be reduced: for all patients it is 120 and 70 mm Hg. Art. Emphasizing the fundamental role of clinical (office) blood pressure measurement both in diagnosis and in monitoring the effectiveness of treatment of hypertension, it should be noted some limitations of this method in the context of its routine use. These include, first of all, “researcher error” - arbitrary rounding, mainly to the nearest ten; subjectivity of measurement (attendance to a certain result - the level of blood pressure that a given patient “should have”); the possibility of overdiagnosis of hypertension due to the phenomenon of “white coat hypertension” (WHC) (in 15–20% of patients); the possibility of underdiagnosis of hypertension or overestimation of the effectiveness of antihypertensive therapy due to the phenomenon of “HBH in reverse” (in 10–15% of patients) and some others [8].
Measuring blood pressure at home
Additional methods for measuring blood pressure—ABPM and measuring blood pressure at home—SCAD can overcome the above-mentioned limitations [9]. The diagnostic value of ABPM as a method used for several decades is beyond doubt, since it is described many times and in detail in various manuals, recommendations, and articles [10–13], and its informativeness has been verified by many years of clinical practice. As for SCAD, this method of measuring blood pressure has always existed in the everyday life of every person, and even more so of patients with hypertension, but its results, as a rule, were questioned by representatives of the medical community due to various technical and methodological problems, as well as the lack of agreed approaches to assessing its results. To date, threshold blood pressure levels for diagnosing hypertension according to various measurement methods have already been clearly defined and prescribed in the relevant recommendations (both Russian and European) (Table 2).
When comparing the blood pressure values given in the table, which make it possible to establish a diagnosis of hypertension according to various measurement methods, it is noteworthy that the blood pressure values corresponding to hypertension in SCAD are 5 mm Hg. Art. lower than when measured in an office. In addition, as mentioned above, ACS, in addition to the office determination of blood pressure, makes it possible to further increase the objectivity and accuracy of its measurements (Table 3 [8]).
Despite the fact that in the arsenal of a modern cardiologist there is a large number of antihypertensive drugs and their combinations with proven effectiveness, the problem of the high prevalence of hypertension and insufficient blood pressure control remains, unfortunately, still relevant [14, 15]. In this situation, the issue of patient compliance becomes of great importance, since it is careful adherence to the doctor’s recommendations for lifestyle correction, regular medication use and systematic monitoring of blood pressure at home that allows the patient to achieve the best results [16–18]. The ability to independently control blood pressure makes the patient an active participant in the treatment process and allows him to see the results with his own eyes; taking medications becomes more meaningful [19]. Accordingly, it is SCAD that can be considered as an effective way to strengthen the interaction between the doctor and the patient and increase the patient’s motivation for treatment.
Choosing the optimal tonometer for SCAD
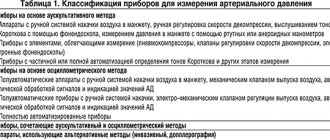
It is quite natural that in the conditions of home blood pressure measurement, the question of choosing the optimal sphygmomanometer (tonometer), which must meet a number of requirements, becomes very relevant. Modern devices designed to measure blood pressure must have accuracy, reliability, compactness, functionality, resistance to negative external influences, artifacts, and in no case should they mislead a person with false readings [20]. In accordance with the existing classification, sphygmomanometers are divided into mercury, mechanical (aneroid) and electronic. The operating principle of mercury and aneroid sphygmomanometers is based on the auscultatory method of measuring blood pressure according to N.S. Korotkov. However, although blood pressure measurement by auscultation is recognized as a reference method, it cannot always be recommended for AMS. A worthy alternative are electronic sphygmomanometers, which allow you to determine blood pressure oscillometrically. Their main advantages include convenience and ease of use; in addition, these devices do not require acute hearing to measure blood pressure, which is important for elderly patients. Electronic sphygmomanometers, depending on the model, can operate in semi-automatic or fully automatic modes. Of course, sphygmomanometers with memory are preferred, which automatically store the values of each measurement (with date and time) and the average of all measurements until the doctor's visit.
Conclusion
Thus, in conditions of insufficient blood pressure control, ACS at home becomes important, which can significantly increase the compliance of patients and, accordingly, the effectiveness of therapeutic measures. The information content of the SCAD is determined by the correct measurement technique and the reliability of the sphygmomanometers used. OMRON (Japan) is deservedly considered one of the world's best manufacturers of electronic sphygmomanometers. She developed her first digital tonometer in 1973. In the early 1990s, Japanese tonometers appeared in Russia and have since been in constant high demand. OMRON is constantly improving and developing technological solutions in the production of tonometers based on the unique patented Intellisense technology, which makes each measurement for any patient individual, accurate, safe and comfortable. The Intellisense technology in the algorithm for calculating the value of systolic and diastolic pressure uses more than 3 indicators per unit of time - the patient’s vascular resistance, time, oscillations and heart rate, unlike other tonometers on the market, which use only one parameter in their algorithm. Intellisense technology provides accurate, safe and comfortable blood pressure measurement for every patient, including patients with arrhythmias. The high sensitivity of the OMRON tonometer is ensured by a pressure sensor, the only one in the world with an official patent. The excellent quality of the equipment is ensured by strict requirements for its production: 100% control and 100% reliability. Currently, the Russian market offers a wide variety of models of OMRON tonometers (OMRON M2 Basic, OMRON M2 Classic, OMRON M3 Comfort, OMRON MitElite, etc.), but each of them is characterized by maximum ease of use, a high level of reliability and efficiency. It is obvious that effective monitoring of blood pressure at home is one of the important conditions for increasing the awareness and compliance of a patient with hypertension, which, in turn, cannot but affect the increase in the effectiveness of antihypertensive therapy and measures aimed at lifestyle correction.
Errors in blood pressure measurements interfere with correct diagnosis
March 14, 2021 marks the 100th anniversary of the death of the Russian surgeon Nikolai Sergeevich Korotkov, who proposed a non-invasive method of auscultal (sound) measurement of blood pressure (BP) back in 1905. And although the Korotkoff method has been used for a long time, errors are still made in measuring blood pressure. On March 3, 2020, the traditional “Scientific Tuesday” of the Federal State Budgetary Institution “NMITs TPM” of the Ministry of Health of Russia was devoted to the issues of measuring blood pressure. , Doctor of Medical Sciences, Professor V.M., reviewed the current international recommendations for measuring blood pressure. Gorbunov.
He gave examples of specific recommendations for blood pressure measurement developed by the American Heart Association (AHA) and the Lancet Commission on Hypertension Group and discussed in detail various aspects of this procedure.
Talking about office blood pressure measurement (measurement within the walls of a medical institution), Vladimir Mikhailovich presented interesting data on mathematical modeling of the prevalence of arterial hypertension (AH) with a normal diet and with a reduction in daily salt intake using the example of Canada. The expected effect of the intervention is only 5 mm Hg. However, even such a seemingly insignificant reduction in blood pressure in the population would have a huge effect: the prevalence of hypertension would decrease from 3.5 to 2.5 million patients, or by 30.3%. This implies the need for extremely careful and accurate blood pressure measurements.
The speaker noted some important elements of standard blood pressure measurement that need to be addressed. Outside of measurement, the mercury column of the tonometer must be at zero, the tonometer must not be damaged, and the numbers must be clearly visible. Aneroid (mechanical) tonometers require regular calibration.
As for electronic tonometers, according to Professor V.M. Gorbunov, the oscillometric algorithms used in them are different and are not disclosed by the manufacturers. Therefore, these devices must be validated according to an international protocol in an independent clinical study. However, in some patients, measurements may be inaccurate due to the limitations of the oscillometric method, which most accurately estimates mean, but not systolic or diastolic blood pressure. As the specialist noted, the validation of electronic blood pressure measurement devices is a critically important point when choosing them for clinical purposes.
To avoid errors when measuring blood pressure in a health care setting, it is important to record readings to the nearest 2 mmHg. avoid arbitrary rounding to 5 or 10 mmHg. Art. At the patient’s first visit to the doctor, blood pressure measurements should be taken on both arms, and subsequently measurements should be taken on the arm on which higher pressure is recorded. At each visit, the patient must take at least two measurements. The Expert Committee recommends the use of arithmetic averages for clinical decisions.
As Vladimir Mikhailovich said, when measuring blood pressure, four types of errors can occur: those associated with the patient, with the procedure itself, with the device and with the observer. Thus, the patient’s intake of food and caffeinated drinks, smoking before the procedure, a full bladder and the well-known so-called “white coat effect” can lead to errors in measurements.
Procedural errors include measuring blood pressure after insufficient rest, incorrect patient positioning (crossed legs), low cuff placement (below heart level), talking during the procedure, and deflating air too quickly. Erroneous data can also be obtained with an inappropriate cuff size. However, the speaker noted, the error arising due to the last two reasons, well known to doctors, is significantly lower than when the basic conditions for preparing the patient and performing the procedure are not observed (insufficient rest, smoking, talking).
Observer errors include arbitrary rounding of the obtained figures, which in 80% of cases gives inaccurate results of systolic and diastolic blood pressure, a single measurement (according to the 2019 AHA recommendations, blood pressure figures can be significantly higher than the true ones, which leads to gross errors in the classification of patients with hypertension) and inaccuracies in determining Korotkoff sounds.
In his speech, Professor V.M. Gorbunov noted that the concept of “office dimension” is becoming more and more blurred with the advent of new varieties of it. Today, there are measurements in clinical studies (carefully standardized, carried out according to a protocol), measurements in real practice - “casual” (without strict compliance with the requirements for the procedure and giving inflated indicators) and automatic office measurements (has many advantages, but gives somewhat underestimated blood pressure numbers and requires additional resources; not yet available in our country).
As Vladimir Mikhailovich said, one of the serious disadvantages of “casual measurements” is that in 20-45% of cases it leads to errors in classifying a patient with hypertension. In addition, during such measurements, high variability of results is noted; systolic pressure is overestimated by 10-15 mm Hg. Art. In addition, the results obtained weakly correlate with signs of target organ damage due to hypertension.
Professor V.M. Gorbunov also spoke in detail about the phenotypes of arterial hypertension and additional indicators of blood pressure, recalled the differences in the recommendations of the European and American Cardiological Societies for diagnosing and determining the degree of arterial hypertension, and provided a new screening algorithm for determining blood pressure phenotypes.
The report also discussed the practical significance of various indicators of blood pressure variability. In conclusion, V.M. Gorbunov focused on new approaches to determining ambulatory blood pressure standards based on assessing the risk of cardiovascular complications. New standards make it possible to more accurately formulate a diagnosis in patients with “problematic” blood pressure phenotypes (masked hypertension and “white coat” hypertension).