Arterial hypertension affects more than 50% of the world's population. The risk of changes in the functioning of blood vessels and the heart increases with age. If in children and young people the indicators are almost always normal or slightly below average, then in men and women after 50 years of age, people with stable 120/80 are rarely found. In most cases, blood pressure levels tend to rise. This is facilitated by a decrease in the elasticity of the vascular walls, accumulated chronic disorders, changes in hormonal status and other factors.
Why is it necessary to reduce blood pressure?
Lowering blood pressure is a necessary part of the treatment of hypertension, which has various origins. This must be done not only to improve well-being, but also to eliminate dangerous conditions:
- crisis;
- arrhythmias;
- hypoxia;
- disturbances in the blood supply to the tissues of internal organs and the brain.
If you ignore high blood pressure readings, the risk of strokes, heart attacks, progression of angina and heart attacks increases. Everyone whose indicators are outside the normal range has to resort to drugs that normalize blood pressure:
- 120–140 mm/Hg: systolic (upper);
- 80–89 mm: diastolic (lower).
Blood pressure close to the lower limits is considered ideal. A tendency to periodically increase values may be the first sign of pathology. Factors provoking the development of the disease:
- stress;
- chronic systemic diseases;
- unfavorable heredity;
- congenital heart and vascular defects;
- disorders of the kidneys;
- unhealthy diet;
- smoking;
- obesity;
- disturbance of carbohydrate or lipid metabolism.
People with incipient or established hypertension often think that they have no health problems. High blood pressure may not show itself at first. As the pathology progresses, it causes sharp throbbing headaches. During an increase in pressure, vision impairment, tinnitus, nausea, and general weakness may occur. Without drug correction, it is not far from a serious attack and irreversible consequences.
Features of the treatment of hypertension
Therapy for hypertension is not carried out periodically, but with the constant use of an antihypertensive drug.
It is an extremely dangerous misconception to use the drug only “when there is pressure.” If hypertension is diagnosed, there is a tendency for a persistent increase in systolic pressure above 140 mm. rt. Art., an antihypertensive drug is taken daily, preferably at the same time, under constant monitoring of blood pressure, for life.
How to use high blood pressure medications
People suffering from hypertension should not buy medications that normalize blood pressure on the advice of friends, pharmacists, or by their own choice. Medicines in this category are selected strictly individually. This is done by the attending physician based on the results of the examination. The type of tablets, their dosage, frequency of administration, and course duration are also determined separately for each patient. The age, stage of hypertension, the causes that caused it, and concomitant diseases are taken into account.
In most cases, patients require medication correction constantly. The doctor may prescribe one or more drugs with different principles of action. Over time, it may be necessary to increase the dosage of tablets. And as your physical condition improves, the amount of medication is reduced.
There are 6 groups of medications to normalize high blood pressure. They all have different mechanisms of action and are available by prescription.
Classification of antihypertensive drugs
Medicines for hypertension, depending on the mechanism of their effect on the human body, are divided into the following groups:
- Agents acting on the renin-angiotensin system.
- Calcium channel blockers.
- Alpha adrenergic blockers.
- Beta blockers.
- Diuretics.
- Neurotropic drugs of central action.
- Medicines that affect the central nervous system.
Doctors often prescribe several blood pressure-lowering drugs to a patient at once, and there is a rational grain in this - combination therapy for many patients will have a more effective effect than taking one drug.
Below we will describe the principle of operation of drugs representing each of the above pharmacological groups.
Calcium antagonists
By blocking the penetration of calcium ions into cells, these drugs cause a reflex relaxation of the muscle walls of blood vessels, reducing their tone. As a result of the expansion of the lumen of the arteries, the blood pressure decreases. Side effects of such drugs include: tachycardia, heart rhythm disturbances, dizziness. Popular tablets of this group:
- Dialtiazem;
- Verapamil;
- Norvasc.
The drugs effectively reduce blood pressure in various forms of hypertension, but do not combine well with other groups of antihypertensive drugs and have many contraindications.
Clinical indications for taking rapid-acting drugs
“First aid” tablets or medicines with instant action should be used in extreme cases, for example, with a rapid increase in blood pressure or an attack of hypertension, when previously used therapeutic actions have proven ineffective.
This rule is due to the fact that such medications contain an increased concentration of active substances, so there is a high probability of an unpredictable reaction of the body due to side effects.
In addition, these drugs are not first-line medications in the treatment of hypertension, as they have a rapid but short-lived effect.
- ACE inhibitors - list of drugs. Mechanism of action of new generation ACE inhibitors and contraindications
So in what cases can you take pills to quickly lower blood pressure? Experts name a number of conditions when taking these drugs is advisable:
- The frequency between sudden surges in blood pressure is less than 30-60 minutes.
- The blood pressure level in patients over 60 years of age exceeds 150/90 units.
- There is severe dizziness.
- There is an increase in heart rate.
- Manifestation of cramps in the calf muscles.
- Nausea and vomiting are present.
- Blurred consciousness and black spots before the eyes.
- Recently suffered from a hypertensive crisis.
- The doctor prescribed taking this medicine in case of a significant increase in blood pressure.
When eliminating an acute pathological situation with fast-acting medications at home, doctors advise:
- The pressure should not be reduced quickly, but gradually, in several stages, that is, at first by no more than 25%.
- Then, over the course of 2-6 hours, reduce to 160/100, measuring blood pressure every 30 minutes, monitoring the upper and lower arterial levels.
- If the pressure rises again to 180/110, take a second dose of the medicine (the interval between the previous dosage should not be less than 30 minutes).
- Maintain the minimum effective dosage, which will help avoid overdose and a sharp drop in blood pressure and pulse rate, as well as the manifestation of hypotension, which is dangerous for the development of ischemia and other serious consequences.
ACE inhibitors (angiotensin-converting enzyme)
Drugs that reduce the production of the enzyme that produces angiotensin, a hormone that provokes vascular spasms and a subsequent increase in blood pressure. They act quite gently, improve the outflow of excess fluid from the body, eliminating swelling. But they often provoke coughing attacks - this is their characteristic side effect. Common drugs:
- Zokardis;
- Captopril;
- Criminals
All products are available in the form of tablets of various dosages.
The most popular drugs for high blood pressure
April 5, 2021
13796
4.9
4
Content
- Captopril
- Amlodipine
- Losartan
- Prestarium
- Veroshpiron
- Concor
- Enalapril
Blood pressure can tell a lot about the state of the cardiovascular system, the functioning of the endocrine organs, the hematopoietic system and the nervous system. There is simply no universal remedy for blood pressure, because blood pressure can be constantly high, or it can rise sporadically. High blood pressure can be an independent pathology, or it can be one of the symptoms among a whole list of problems.
Therefore, you cannot just come to the pharmacy and ask for “something for blood pressure” - such drugs are prescribed exclusively by a doctor, knowing the full picture of the disease.
Principles for choosing antihypertensive drugs
A.A.
UPNITSKY ,
Russian National Research Medical University named after. N.I. Pirogova, Moscow Arterial hypertension (AH) and its complications are widespread in the population today and carry a high risk of disability and death among the population, mainly of working age (cerebral stroke, myocardial infarction, chronic heart failure, end-stage renal failure, cardiac arrhythmias, etc.) .
At the same time, the effectiveness of blood pressure control in patients with hypertension remains unacceptably low for various reasons. This article presents an attempt to streamline the prescription of antihypertensive drugs by applying a specific algorithm for their prescription, including adequate monitoring of the ongoing antihypertensive therapy. The article uses the latest ESC/ESH-2013 recommendations, as well as the American JNC-8 of December 2013 for the treatment of hypertension (JAMA-2014, December, online). The work provides an original algorithm for choosing antihypertensive therapy, including methods and timing for assessing both the effectiveness and safety of antihypertensive therapy. At the beginning of the article, it is appropriate to provide a classification of arterial hypertension according to blood pressure level ( Table 1
).
Table 1. Classification of arterial hypertension by blood pressure level
| Category | Systolic blood pressure, mm Hg. Art. | Diastolic blood pressure, mm Hg. Art. |
| Optimal | <120 | <80 |
| Normal | <130 | <85 |
| High normal | 130-139 | 85-89 |
| Hypertension 1st degree | 140-159 | 90-99 |
| Hypertension 2nd degree | 160-179 | 100 -109 |
| Hypertension 3rd degree | ≥180 | ≥110 |
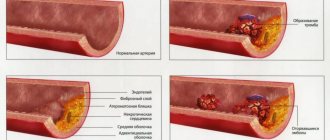
Relationship between blood pressure and damage to the cardiovascular system and kidneys
The relationship between blood pressure and cardiovascular and renal complications and mortality has been studied in a large number of observational studies. Their main results are as follows:
1. Office BP is directly associated with the incidence of stroke, myocardial infarction, sudden death, heart failure and peripheral arterial disease (PAD), as well as end-stage renal disease (ESRD). 2. In individuals over 50 years of age, SBP appears to be a better predictor of clinical events than DBP. In elderly and senile people, pulse pressure (the difference between SBP and DBP) plays a possible additional prognostic role. This is also evidenced by a particularly high cardiovascular risk in patients with elevated SBP and normal or low DBP - isolated systolic hypertension (ISAH). 3. Blood pressure values measured outside the office, such as those obtained during ABPM and home blood pressure monitoring (HBP) are also related to clinical events. 4. The relationship between cardiovascular morbidity and mortality varies depending on the presence of other concomitant cardiovascular risk factors listed below.
Risk stratification criteria for arterial hypertension (recommendations of VNOK-2004)
Risk factors
Basic
- Men > 55 years old.
- Women > 65 years old.
- Smoking.
- Cholesterol > 6.5 mmol/L, or low-density lipoprotein cholesterol >.4.0 mmol/L, or high-density lipoprotein cholesterol < 1.0 mmol/L.
- Family history of early CCP (women <65 years, men <55 years).
- AO (OT ≥ 102 cm for men or ≥ 88 cm for women).
- CRP ≥ 1 mg/dl.
Additional
- NTG.
- Low physical activity.
- Increased fibrinogen.
Target organ damage (stage II hypertension) Left ventricular hypertrophy (ECG, echocardiography, radiography).
Microalbuminuria (30-300 mg/day). Ultrasound signs of thickening of the arterial wall (thickness of the intima-media layer of the carotid artery ≥ 0.9 mm) or atherosclerotic plaques of the great vessels. A slight increase in serum creatinine 115-133 µmol/l for men or 107-124 µmol/l for women. Associated clinical conditions (stage III hypertension)
Cerebrovascular diseases
- Ischemic stroke.
- Hemorrhagic stroke.
- Transient ischemic attack
Heart diseases
- Myocardial infarction.
- Angina pectoris.
- Coronary revascularization.
- Congestive heart failure
Kidney diseases
- Diabetic nephropathy.
- Renal failure (creatininemia > 2.0 mg/dL).
- Proteinuria (>300 mg/day).
Peripheral artery diseases
- Dissecting aortic aneurysm.
- Symptomatic peripheral artery disease
Hypertensive retinopathy
- Hemorrhages or exudates.
- Swelling of the optic nerve nipple.
Thus, to reduce cardiovascular risk and prevent the above-mentioned consequences of hypertension, along with a number of non-drug measures (control of body weight, metabolic profile, smoking control, limiting salt intake, cyclic aerobic exercise of sufficient intensity and duration, a full night’s sleep), it is necessary to achieve target blood pressure levels using primarily antihypertensive drugs.
So, how to choose them correctly? Requirements for the treatment of hypertension [1]:
- Smooth decrease in blood pressure.
- Patient compliance.
- Regression of target organ damage.
- Increasing life expectancy and improving its quality.
- Stable maintenance of blood pressure at the target level.
Target blood pressure is the blood pressure level at which the minimum risk of cardiovascular morbidity and mortality is recorded ( Table 2
).
Table 2. Target blood pressure levels
| Patient group | Target BP |
| General population of patients with hypertension | <140/90 mmHg Art. |
| Hypertension + diabetes, proteinuria <1 g/day | <130/85 mmHg Art. |
| AH + DM, proteinuria > 1 g/day | <125/75 mmHg Art. |
| AH + chronic renal failure | <125/75 mmHg Art. |
| Patients over 60 years of age | <150/90 mmHg Art. * |
| * JNC-8, JAMA, December 2014, online. | |
We propose to select antihypertensive drugs according to a certain scheme - an algorithm consisting of three main fundamental stages. The use of such an algorithm should help the doctor treating such patients to achieve maximum effectiveness and at the same time minimize the risk of side effects of the pharmacotherapy.
The first stage of choosing an antihypertensive drug is pathogenetic ( Fig. 1
). In a patient with hypertension, we suggest two steps at this stage. The first is compiling a list of drugs that effectively affect the pathogenesis of the symptom - high blood pressure. In other words, the doctor should try in each specific case to determine which hemodynamic factor “warms up”, so to speak, increased blood pressure [1-3].
Figure 1. Pathogenetic stage of selection of antihypertensive drugs
Selection of drugs depending on the cause of increased pressure
| Increased cardiac output | Increased peripheral resistance | Increased circulating blood volume |
|
|
|
Selection of drugs in accordance with their organoprotective properties
| Cardioprotective drugs | Cerebroprotective drugs | Nephroprotective drugs |
|
|
|
This factor may be, for example, increased cardiac output (in the “hyperkinetic” version of hypertension, as in hyperthyroidism, or in the early stages of hypertension in young and sometimes middle-aged people).
In patients with “experienced” hypertension, cardiac output is extremely rarely increased, and increased peripheral resistance comes to the fore in maintaining elevated blood pressure. First, it is caused by transient increases in peripheral arterial vascular resistance in response to increases in blood pressure (the meaning of this phenomenon is the protection of peripheral organs and tissues from hyperperfusion). Over time, hypertrophy of the middle muscular layer of arterioles—resistance vessels—develops, and increased peripheral resistance is fixed at the organic level. Another component of this “equation” may be an increased circulating blood volume (CBV), the so-called. volume-dependent hypertension. As a rule, these are patients with obesity (there are many small vessels in the adipose tissue with additional blood volume), with swelling or pastiness of the legs, if they are not caused by chronic venous insufficiency.
According to the assessment of the hemodynamic variant of hypertension by the attending physician, in the first case, the list of effective drugs will include those that reduce cardiac output (beta-blockers, centrally acting drugs, “rhythm-slowing” calcium antagonists) [1, 4]
In the second, this will be a list of drugs that reduce total peripheral vascular resistance (TPVR): ACE inhibitors, angiotensin II receptor antagonists of the 1st subtype (sartans), calcium antagonists (all), centrally acting drugs (I1 receptor agonists - rilmenidine, moxonidine etc.), sympatholytics (dopegit), beta-blockers with a vasodilating effect (carvedilol, nebivolol, etc.), long-acting alpha-blockers (doxazosin, terazosin, etc.), diuretics (with regular use for at least 2-3 weeks .). The latter reduce OPSS due to the removal of sodium from the vascular wall, which leads to a decrease in OPSS both by reducing its edema and by reducing its response to vasoconstrictor stimuli.
In the third case, preference will be given to diuretics. It should be remembered that mixed hemodynamic options are possible, and in such cases, drugs are combined [5].
But, given the importance of target organ damage in hypertension and organ protection, the doctor must identify in each patient with hypertension his version of target organ damage: this could be the brain and its vessels (“cerebral” version according to the old classification), the heart - in the form changes in the left sections (hypertrophy or dilatation of the left atrium and ventricle), as well as damage to the coronary arteries with an obvious or latent form of myocardial ischemia (cardiac form of hypertension); kidneys (microalbuminuria); hyperazotemia indicates advanced stages of kidney damage in hypertension. It is also possible to detect changes in the vessels of the retina or arteries of the lower extremities (also often asymptomatic, but detected during a targeted examination).
In accordance with the identified “target” organ (“targets”), the doctor compiles, still at the same first stage, a list of antihypertensive drugs that have appropriate organoprotective properties for hypertension (cardio-, cerebro- or nephroprotective).
ACE inhibitors, angiotensin II receptor antagonists of the 1st subtype (sartans), beta-blockers, calcium antagonists (to varying degrees), indapamide have proven cardioprotective properties; centrally acting antihypertensive drugs have moderate effects [1, 6–8].
Calcium antagonists (nimodipine) have cerebroprotective properties in hypertension, although this issue is not yet completely clear.
Nephroprotective properties in hypertension have been proven for ACE inhibitors, especially with a combination of hypertension and diabetes mellitus, angiotensin II receptor antagonists of the 1st subtype (sartans), as well as calcium antagonists.
Having now compared both lists (“hemodynamic” and “organoprotective”), the doctor should leave in the final list of the 1st stage only those drugs that are present in both lists simultaneously. This will be the final list of the 1st stage - a list of drugs that are effective in this particular case, but not yet taking into account their safety for the patient.
This aspect of drug selection is the subject of the second stage, in which the list of antihypertensive drugs that are effective for a given patient in a given situation, compiled at the first stage, should be considered from a different angle, namely: whether all effective drugs from this list will be safe for this patient. To solve this problem, we must return to the anamnesis (indications in the anamnesis of intolerance or unsatisfactory tolerability of certain drugs, including those related to those prescribed). Next, you should review the list of concomitant diseases in this patient - contraindications to taking certain medications may also be identified here. For example, if you have a history of bronchial asthma, drugs from the group of beta-blockers are contraindicated. These same drugs, with the exception of beta-blockers, which have vasodilating properties, are contraindicated in patients with stenosing atherosclerosis of the arteries of the lower extremities, with intermittent claudication. Beta-blockers are also contraindicated in cases of atrioventricular block above degree I/bradycardia less than 50 per minute. Alpha-blockers are contraindicated in case of concomitant angina pectoris, as they can cause an increase in anginal attacks. Sympatholytics, which have recently been used extremely rarely, are contraindicated in persons with peptic ulcer disease. Calcium antagonists are contraindicated in patients with gastroesophageal reflux disease (GERD) because they cause relaxation of the lower esophageal sphincter and thereby may worsen the symptoms of GERD. Calcium antagonists, primarily verapamil, can significantly aggravate constipation and are therefore contraindicated in this category of patients. Diuretics can increase the level of uric acid in the blood, and therefore hyperuricemia and gout are contraindications for them. For carbohydrate metabolism disorders, the only safe diuretic is indapamide. A number of antihypertensive drugs can have a negative effect on the course and outcome of pregnancy. Therefore, a limited range of antihypertensive drugs is prescribed for it [1, 6, 7]:
- Methyldopa.
- Labetolol.
- Pindolol.
- Oxprenolol.
- Nifedipine SR.
- Hydralazine.
- For kidney disease - diuretics.
Thus, after the 2nd stage of selection, only drugs that are effective and at the same time safe for a patient with hypertension will remain on the list.
The third and final stage of choosing an antihypertensive drug is the stage of individualization of pharmacotherapy.
The first step is to decide what pharmacotherapy is indicated for this patient (mono-or combined). When resolving this issue, one should proceed from the degree of increase in blood pressure and the duration of hypertension. With long-term hypertension, with high numbers, you should start with a combination of antihypertensive drugs from the very beginning. At the same time, rational and irrational combinations of antihypertensive drugs are distinguished ( Fig. 2
).
possible combinations (only dihydropyridine calcium antagonists can be normally combined with β-blockers) Red continuous line: not recommended combination |
In cases of mild hypertension, not corrected by non-drug treatment methods (see above), and moderate hypertension, monotherapy is possible in some cases.
However, in the treatment of hypertension there is a rule: combinations of antihypertensive drugs with different mechanisms of action are preferable to high-dose monotherapy. Firstly, in combination, the effect is achieved by influencing different parts of the pathogenesis of hypertension, and secondly, with the right combination, the side effects of the drugs are mutually neutralized. For example, “escape” of the hypotensive effect due to the activation of counter-regulatory mechanisms manifests itself when taking arteriolar vasodilators by increasing cardiac output; when taking all antihypertensive drugs, except diuretics, due to sodium and water retention in the body; when taking diuretics – due to the activation of the body’s neurohormonal systems, in particular the renin-angiotensin-aldosterone system [1, 5, 6]. The choice of method of administration of an antihypertensive drug is determined by the clinical situation: in case of an acute rise in blood pressure, drugs are administered parenterally (intravenously or intramuscularly), as well as sublingually (Capoten, Prazosin, Corinfar, etc.) ( Table 3
). It should be noted that these drugs have a short onset of effect and at the same time a short half-life. That is, they should be used specifically in acute situations, and are much less suitable for long-term use. The fact is that when taking short-acting drugs, there are constant fluctuations in their concentration in the blood, and after them, fluctuations in their hypotensive effect, which is accompanied by significant variability in blood pressure during the day. The latter is an unfavorable factor; in particular, the risk of hypertension complications increases. In addition, when taking the last dose of such a drug, even before bedtime, it still does not prevent the morning rise in blood pressure.
Table 3. Medicines for self-relief of blood pressure rise (according to M.V. Leonova, 2012, as amended)
| Drug (INN*) | Method of administration | Start of action | Maximum effect | Duration of action | Doses |
| Captopril | Inside, under the tongue | 15 minutes | 1-2 hours | 4-6 hours | 12.5-50 mg |
| Clonidine | Inside, under the tongue | 30 min | 1-2 hours | 8-12 h | 0.075-0.15 mg |
| Nifedipine | Orally or chew | 15 min 5 min | 30 min 15 min | 4-6 hours 4 hours | 10-20 mg |
| Prazosin | Inside, under the tongue | 15-30 min | 1-2 hours | 8 hours | 1-2 mg |
| Nitroglycerine | Under the tongue, lingual spray | 1 min | 15 minutes | 30 min - 1 hour | 0.3-0.5 mg |
| * International nonproprietary name. | |||||
Here it should be recalled that in case of exacerbation of hypertension, one should try to identify its cause.
In this case, we may encounter the patient’s abuse of table salt, alcohol, taking non-steroidal anti-inflammatory drugs to relieve pain (arthrosis, arthritis, sciatica, headaches, etc.), constant lack of sleep for some reason, non-compliance with the recommended pharmacotherapy (skipping medications). Therefore, long-acting drugs with a long half-life are indicated for continuous maintenance antihypertensive therapy. Another important advantage of drugs with a long duration of action is the possibility of taking them once or twice a day, which helps to increase patient adherence to treatment (according to some data, in the treatment of hypertension during the year it is about 40%). Obviously, this does not mean adequate blood pressure control.
In this regard, the antagonist of angiotensin II receptor subtype 1, candesartan, is of interest; it has the longest half-life of all drugs in this group (more than 24 hours), which makes it possible to achieve blood pressure control also in the morning. In addition, candesartan has advantages over other drugs in cases of combination of hypertension with chronic heart failure, type 2 diabetes mellitus, diabetic nephropathy, proteinuria, and left ventricular myocardial hypertrophy.
To date, the results of 14 placebo-controlled studies with candesartan in 3,377 patients with hypertension are available. Daily doses of the drug ranged from 2 to 32 mg with a follow-up period of 4 to 12 weeks. Baseline blood pressure (diastolic) (DBP) ranged from 95 to 114 mmHg. Art. Within this dosage range, 2,350 patients received active candesartan therapy and 1,027 patients received placebo. In all studies, a significant hypotensive effect of candesartan was noted, which was dose-dependent, i.e., it was more pronounced the higher the dose of candesartan.
From a safety standpoint, the absence of a “first dose effect” was demonstrated, i.e., when taking the first dose of candesartan, there was no sharp decrease in blood pressure. As with other antihypertensive drugs, the hypotensive effect of candesartan increased during the first two weeks and by the end of this period was already clearly expressed. Similar to other antihypertensive drugs, the maximum effect was observed at the end of the 1st month of therapy. Moreover, the hypotensive effect of candesartan did not depend on the age or gender of patients, as well as on race and ethnicity. Of particular note is the good tolerability of candesartan even at a daily dose of 32 mg.
As for the stability of the hypotensive effect, in studies lasting up to one year there was no evidence of the hypotensive effect of candesartan.
Comparative studies of candesartan and losartan in hypertension were also conducted (CANDLE, CLAIM I and II studies, meta-analysis by Zhenfeng Zh, Huillan Shi, Junya Jia et al.), which demonstrated the advantage of candesartan in terms of the severity of blood pressure reduction and its tolerability by patients.
Thus, candesartan has a long-term pronounced hypotensive effect, which depends on the dose of the drug.
The intervals between doses of antihypertensive drugs, with the exception of diuretics, are 2-3 half-lives of the drug and are indicated in the instructions for it. At the same time, one should keep in mind the possibility of reducing the duration of action of antihypertensive drugs when they are accidentally simultaneously prescribed with drugs that are inducers of hepatic metabolism, accelerating the metabolism of antihypertensive drugs in the liver and their excretion from the body. Inducers of hepatic metabolism include, in particular, phenobarbital, other anticonvulsants, rifampicin, etc. In such cases, the intervals between doses of antihypertensive drugs should be reduced [1, 6].
Duration of treatment. With a certain “experience” of hypertension in the body, a “reconfiguration” (“resetting”) of blood vessels, kidneys, brain, and heart occurs to work at elevated blood pressure. In addition, the body retains mechanisms that support hypertension (except for rare cases of surgical treatment of arterial stenosis, removal of adrenal aldosteroma, pheochromocytoma, thyroidectomy and some others). That is why, after normalization and stabilization of blood pressure, antihypertensive therapy should not be stopped. Another thing is that over time, especially in the warm season, it is permissible to reduce the dose and amount of antihypertensive drugs under the control of blood pressure and well-being, provided that all non-drug methods of lowering blood pressure are followed. Criteria for assessing the effectiveness and safety of antihypertensive therapy
To assess the effectiveness, along with assessing the dynamics of the patient’s well-being, office BP measurements should be used, as well as additional methods: 24-hour BP monitoring - ABPM, home measurement (HBP) by the patient.
When measuring office blood pressure, this should be done repeatedly at intervals of 2 minutes, following certain rules. In addition, to assess the safety of antihypertensive therapy, especially alpha-blockers, diuretics, ACE inhibitors and their combinations, blood pressure should be measured in clinostasis (lying down, after 5 minutes) and in orthostasis (after 2 minutes in an upright position). A pronounced decrease in blood pressure in orthostasis (by 20 mm Hg or more) increases the risk of cardiovascular complications and may adversely affect the patient’s well-being.
Additional methods of blood pressure control (ABPM and DMBP) make it possible to avoid unnecessary and unsafe therapy for the patient in the case of “white coat hypertension”, to identify patients with a predominantly nocturnal rise in blood pressure or with an insufficient or excessive decrease in blood pressure at night. The information obtained is valuable for the correct selection and evaluation of antihypertensive therapy [1, 2, 6–8].
To help the practitioner, we provide a list of some fixed combinations of antihypertensive drugs ( Table 4
).
Table 4. Fixed combinations of antihypertensive drugs
| Angiotensin-converting enzyme inhibitor + calcium antagonist |
| Enalapril 5 mg + felodipine 5 mg Benazepril 10/20 mg + amlodipine 2.5/5 mg Perindopril 5/10 mg + amlodipine 5/10 mg Trandolapril 1/2/4 mg + verapamil SR 180/240 mg Enalapril 10 mg + diltiazem 180 mg Lisinopril 10/20 mg + amlodipine 5/10 mg Ramipril 5 mg + felodipine retard 5 mg |
| Angiotensin II receptor antagonist + calcium antagonist |
| Valsartan 80 mg + amlodipine 5 mg |
| Angiotensin-converting enzyme inhibitor + diuretic |
| Lisinopril 10/20 + hydrochlorothiazide 12.5/25 mg Captopril 25/50 + hydrochlorothiazide 12.5/25 mg Enalapril 20 mg + hydrochlorothiazide 12.5 mg Enalapril 10 mg + hydrochlorothiazide 25 mg Enalapril 10 mg + hydrochlorothiazide 12.5 mg Quinapril + Hydrochlorotiazide 12.5/25 mg Lisinopril 10 mg + hydrochlorotiazide 12.5 mg ramipril 5 mg + hydrochlorotiazide 12.5 mg fosinopril 20 mg + hydrochlorotiazide 12.5 mg moexipril 15 mg + hydrochlorotiazide 25 mg cylized 5 mg + hydrochlorotiazide 12.5 mg Perindopril 2 mg + indapamide 0.625 mg Perindopril 4 mg + indapamide retard 0.5 mg |
| Angiotensin II receptor antagonist + diuretic |
| Losartan 50 mg + hydrochlorothiazide 12.5 mg Valsartan 80 mg + hydrochlorothiazide 25 mg Eprosartan 600 mg + hydrochlorothiazide 12.5 mg Irbesartan 150/300 mg + hydrochlorothiazide 12.5 mg Telmisartan 80 mg + hydrochlorothiazide 12.5 mg Telmisartan 40/8 0 mg + hydrochlorothiazide 12.5 mg Candesartan 8 mg + hydrochlorothiazide 12.5 mg |
| β-blocker + diuretic |
| Pindolol 10 mg + clopamide 5 mg Bisoprolol 2.5 mg + hydrochlorothiazide 12.5 mg Propanolol 40/80 mg + hydrochlorothiazide 12.5 mg Bisoprolol 2.5/5/10 mg + hydrochlorothiazide 6.25 mg Metoprolol 50/100 mg + hydrochlorothiazide 25/50 mg Atenolol 100 mg + chlorthalidone 25 mg Atenolol 50/100 mg + chlorthalidone 12.5/25 mg Calcium antagonist + |
| β-blocker |
| Felodipine retard 5 mg + metoprolol succinate 50 mg Amlodipine 5 mg + atenolol 50 mg |
In conclusion, we urge all doctors involved in the treatment of hypertension in outpatient and inpatient settings to approach the diagnosis and treatment of patients with hypertension thoughtfully, clearly understanding the sequence of actions for diagnosis and selection of antihypertensive therapy, and we wish them good luck on this thorny path.
BIBLIOGRAPHY
1. Recommendations for the treatment of arterial hypertension. ESH/ESC 2013. Russian Journal of Cardiology, 2014, 1: 5-92. 2. VNOK. Prevention, diagnosis and treatment of arterial hypertension. Russian recommendations (fourth revision). M., 2010. 3. Recommendations of VNOK. Diagnosis and treatment of arterial hypertension. M., 2009: 5-34. 4. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: Recommendations, review, and responsibility. JAMA, 2013, December 18. 5. James PA, Oparil S, Carter BL et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA, 2013, December 18. 6. Peterson ED, Gaziano JM, Greenland P. Recommendations for treating hypertension: What are the right goals and purposes? JAMA, 2013, December 18. 7. Sox HC. Assessing the trustworthiness of the guideline for management of high blood pressure in adults. JAMA, 2013, December 18. 8. Wood S. JNC 8 at Last! Guidelines Ease Up on BP Thresholds, Drug Choices. Medscape, December 18 (https://www.medscape.com/viewarticle/817991).
Prestarium
The advantage of this blood pressure drug is that it not only helps reduce blood pressure, but also treats hypertension, even complex forms. Prestarium is prescribed if there is a risk of heart attack; patients who have problems with cerebral circulation can take it. But the problem is that Prestarium tablets are not available in all pharmacies and they are not cheap. But there are analogues of this medicine that a doctor can select.
Prestarium
SERVIER (Servier), France
A drug used for arterial hypertension and heart failure.
Also for such indications as: Prevention of recurrent stroke in patients with cerebrovascular diseases. Prevention of cardiovascular complications in patients with documented stable coronary heart disease. from 193
1013
- Like
- Write a review
Captopril
This is one of the best drugs when you need to quickly lower your blood pressure. "Captopril" is not prescribed for use on an ongoing basis or in a course. This drug is often prescribed if a person has heart problems. Captopril has different dosages, but the most popular is 25 mg. For optimal results, take one tablet and place the second one under the tongue.
Captopril
OZON, Russia
Arterial hypertension (including renovascular), chronic heart failure (as part of combination therapy), left ventricular dysfunction after myocardial infarction in patients in a clinically stable condition.
Diabetic nephropathy in type 1 diabetes mellitus (with albuminuria more than 30 mg/day). from 8
5.0 1 review
766
- Like
- Write a review
Losartan
This drug can be taken as a course or once for emergency blood pressure reduction. "Losartan" acts instantly, without having a negative effect on the cardiovascular system. A maximum of an hour after administration, the blood pressure returns to normal. The drug is also prescribed if a person suffers from heart failure.
Losartan
JSC VERTEX, Russia
Arterial hypertension.
Reducing the risk of associated cardiovascular morbidity and mortality in patients with arterial hypertension and left ventricular hypertrophy, manifested by a combined reduction in the incidence of cardiovascular mortality, stroke and myocardial infarction. Protection of the kidneys in patients with type 2 diabetes mellitus with proteinuria - slowing the progression of renal failure, manifested by a decrease in the incidence of hypercreatininemia, the incidence of end-stage renal failure requiring hemodialysis or kidney transplantation, mortality rates, as well as a decrease in proteinuria. Chronic heart failure (as part of combination therapy, with intolerance or ineffectiveness of therapy with ACE inhibitors). from 30
1160
- Like
- Write a review
Concor
The active ingredients of these blood pressure pills reduce the amount of adrenaline in the blood, which has a good effect on the functioning of the heart. Concor reduces heart rate and is suitable for those who have had a heart attack. But Concor is not suitable for older people and those with severe hypertension.
Concor
Merkle GmbH, Germany
- arterial hypertension;
— IHD: stable angina; - chronic heart failure. from 123
5.0 1 review
1350
- Like
- Write a review