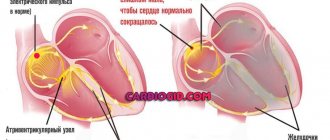
Conduction of nerve excitation is one of the unique functions of the heart. It ensures sequential transmission of impulses from the main node to the atria and ventricles. To do this, special cells connected into branches run inside the interventricular septum. After the name of the discoverer, they are called bundles or legs of His.
The endings in the area of the lower part of both ventricles and the apex of the heart form a thin network of Purkinje fibers.
Any disturbance of intraventricular conduction entails a more or less pronounced interruption of the method of impulse transmission. Such changes are called blockade. They are functional or organic in nature. Most often, obstruction of the ventricular tract reflects the degree of damage to the heart muscle by the pathological process.
Intraventricular blockades themselves do not pose any harm to the functioning of the heart. But they seriously complicate the underlying disease and affect other myocardial functions and prognosis.
Intraventricular conduction disorders do not have typical clinical symptoms and are detected during a control ECG study.
How common are intraventricular blocks?
Impaired conduction within the ventricles can be found in both children and adults. Among the pathologies detected using electrocardiography, the proportion of intraventricular blockades is up to 2.4%. There has been an increase in the frequency of detection in elderly patients.
By prevalence among the population:
- in the first place is a block in the left leg (anterosuperior branch);
- on the second - the right leg.
Impaired conduction in the posteroinferior bundle is rare.
Types of ventricular blocks
According to V.L. Doshchitsin’s classification, all intraventricular conduction disorders are divided into:
- mono-, bi- and trifascicular depending on the damage to one or two or three bundles;
- focal: local damage is not confirmed in all ECG leads;
- arborization: localized in the terminal part of Purkinje fibers;
- transient: changes alternate with correct conductivity;
- persistent;
- complete and incomplete;
- alternating: first one or another type of blockade is detected.
A pathological process can cause an impulse block at any level
Depending on the location of the impulse interruption, blockades are distinguished:
- monofascicular (single-bundle): a block of the left anterior or posterior, only the right bundle branch is detected in isolation;
- bifascicular (two-bundle): available in two versions: unilateral (left leg) or bilateral (right with the left anterior branch, right with the left posterior).
- trifascicular (three-bundle).
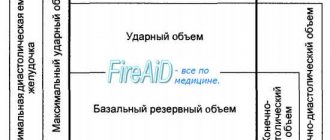
The type of blockade is reflected in the transcript of the electrocardiogram. The conduction of impulses from the supraventricular nodes of the heart slows down or is completely interrupted. This disrupts the sequence of excitation of the ventricles, affects the biochemical processes in the myocardium, and the fullness of cardiac output.
The reasons for different types of blockades differ from each other and cause different changes. Let us consider how intraventricular conduction disturbance occurs in myocardial diseases.
Diagnosis
- You can suspect a pathology of impaired patency of the NI during the initial examination of the patient, namely by tapping his chest. The doctor may notice an increase in the size of the heart, which indicates the presence of dysfunction;
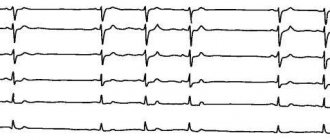
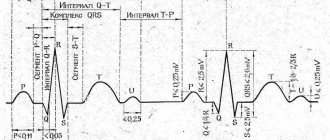
- The electrocardiogram method most often shows the development of the disease. When interpreting the results on the ECG, there will be a noticeable increase in the height of the P wave, as well as its significant thickening. In addition, you can see a difference in the duration of the PQ interval, which indicates that the heart is contracting at an uneven rate. Often, specialists prescribe electrocardiographic monitoring of the patient’s heart function throughout the day. This method makes it possible to monitor the dynamics of the heart rhythm on an ECG over a long period or with increasing physical activity;
- conducting a general analysis of the patient's blood and urine. Based on their results, it is possible to determine the amount of specific hormones in the blood and urine that affect the slowdown of the contraction of the heart muscle;
- Using an electrophysiological examination method, it is possible to determine the exact location of the disorder. To do this, a thin electrode is inserted through which the heart is exposed to a low-power impulse. The electrode is inserted through the intestine or cardiac aorta. This method will help to carry out treatment as effectively as possible.
The use of these and other techniques will allow us to determine the main cause of the disease, and therefore prescribe drugs that will quickly eliminate it.
If the disorder is not associated with the patient having any cardiovascular disease, specialists prescribe a course consisting of the following medications:
- vitamins or mineral complexes;
- drugs whose action is aimed at regulating and stabilizing the process of blood flow into the heart (ATP or Preductal).
When diagnosing complete intraventricular obstruction, treatment consists of introducing an artificial pacemaker that will stimulate the heart rhythm at a set frequency. Otherwise, the patient may develop cardiac bradycardia with subsequent complications.
If a patient is diagnosed with both intraventricular conduction disorder and 1st or 2nd degree atrioventricular block, the prescription of any drugs should be extremely careful and attentive. This is due to the fact that by blocking an attack of one type of blockade, it is possible to activate the cause for the development of another type of pathology
Such patients should be under constant supervision of specialists and periodically undergo electrocardiographic examination
This is due to the fact that by blocking an attack of one type of blockade, it is possible to activate the cause for the development of another type of pathology. Such patients should be under constant supervision of specialists and periodically undergo electrocardiographic examination.
Take care of yourself and be healthy!
What happens when there is a block in the right bundle branch?
Mechanism of conduction disturbance: in the case of complete block of the right branch of the bundle, the right ventricle and the adjacent half of the interventricular septum receive excitation in a different way. The wave of cellular depolarization passes here from the left part of the interventricular septum, from the other ventricle. They are excited first, and slowly transmit impulses through the fibers to the right ventricle.
Incomplete blockade is distinguished by the correct transmission path, but the slow speed of the impulse.
The causes of complete block are mainly diseases accompanied by overload of the right ventricle:
- chronic lung diseases with the formation of “pulmonary heart”;
- congenital malformations, valve failure in children;
- of the acquired defects, mitral stenosis is important, creating increased pressure in the pulmonary circulation;
- chronic ischemic disease combined with arterial hypertension;
- myocardial infarction of the posterior diaphragmatic and apical region, detection of pathology is regarded as an indicator of the high prevalence of the zone of necrosis and ischemia.
X-ray of the overloaded right ventricle is visible as an expansion of the contours at the top right
In a healthy heart, this type of blockage is rare.
The reasons for incomplete blockade should be added:
- myocarditis (rheumatic carditis, consequences of infectious viral diseases in a child);
- diffuse and focal cardiosclerosis;
- thickening of the left ventricle due to hypertension;
- intoxication with drugs (digitalis derivatives, quinidine, β-blockers).
- nonspecific electrolyte disturbances.
In these cases, slow conduction indicates ventricular hypertrophy. Possible as a variant of the norm in athletes.
Expert advice: when to install a pacemaker
Installation of a pacemaker is a surgical procedure and is prescribed only when indicated.
There is no point in carrying out the procedure in the absence of obvious symptoms of pathology. If the patient feels well, the introduction of an artificial pacemaker is not indicated. Surgery is not recommended if the identified symptoms are associated with reversible causes. You need to cope with the underlying disease - and the heart muscle will be able to function fully again. Indications for installation of a pacemaker:
- bradycardia with a heart rate less than 40 beats/min and rhythm disturbances in the presence of obvious symptoms;
- complications that threaten the patient's life;
- MAS attacks;
- persistent conduction disturbances after myocardial infarction.
The possibility of installing a pacemaker is being discussed when the pulse is less than 40 beats/min in the absence of obvious clinical symptoms. The procedure is performed at any age.
Prevention of cardiac conduction disorders has not yet been developed. Do not delay treatment, avoid risk factors. This will reduce the chances of developing pathology. To identify the problem in time, regularly undergo preventive examinations with a therapist with an ECG assessment (as necessary).
Disorders with blockade of the left anterior branch
Mechanism of conduction disturbance: there are necessarily obstacles to the conduction of excitation along the anterior and lateral walls of the left ventricle. First, the impulse passes through the left posterior branch, activating the interventricular septum and the lower posterior wall. Then, along the Purkinje fibers, the excitation wave, directed from bottom to top, passes to the anterolateral part of the left ventricle.
Causes: pathology of the left chambers of the heart:
- myocardial infarction of the anterior or lateral wall;
- focal cardiosclerosis;
- hypertension;
- non-closure of the interatrial septum;
- aortic defects;
- mitral valve leaflet insufficiency;
- myocarditis;
- hypertrophic cardiomyopathy;
- myocardial dystrophy with metabolic changes.
How is a blockade formed in the left posterior branch?
Mechanism of conduction disturbance: impulse delivery is inhibited in the posteroinferior part of the left ventricle. Excitation goes along the left anterior bundle to the myocardium of the anterolateral region, and along Purkinje fibers it spreads to the posterior and lower sections. The myocardium is activated along the anterior wall from top to bottom.
This type of block is rarely isolated; it is more often found in conjunction with a right bundle branch block.
Causes: focal changes in the left ventricle from the posterior wall with:
- posterior phrenic myocardial infarction;
- cardiosclerosis;
- myocarditis;
- cardiomyopathies;
- idiopathic calcification of the conduction system.
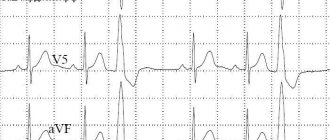
ECG picture for myocardial infarction with left leg block
Double-bundle block of the left leg
Mechanism of conduction disturbance: the block of the common trunk of the left leg should be located before the branching into the anterior and posterior branches or simultaneously block the flow of impulses along both branches. The right ventricle is excited in the usual way, after which the wave is transmitted through the contractile cells to the left ventricle from right to left. In the case of an incomplete block, some impulses, albeit slowly, “break through” along the left leg.
The reasons for the occurrence of this type of conduction disorder must be sought in very extensive damage to the left ventricle when:
- acute transmural myocardial infarction;
- diffuse cardiosclerosis;
- aortic defects and coarctation;
- malignant course of arterial hypertension.
Clinical case
Patient M., 65 years old, was admitted to the therapeutic department. At the time of examination, he complains of shortness of breath during physical activity, frequent attacks of dizziness, and general weakness. There were repeated losses of consciousness.
During the interview, we found out that similar symptoms had been bothering her for more than a year. Over the course of 14 months, severe weakness, headaches, and dizziness are noted. For six months there were losses of consciousness - about once a week. Over the past month, fainting has occurred almost daily. The patient loses consciousness for one minute, then general weakness is noted.
During further examination, changes were detected on the ECG. Ultrasound and Doppler sonography were performed and left ventricular failure and valvular stenosis were detected. Diagnosis: Coronary heart disease; rhythm disturbances such as bifascicular blockade and attacks of MAS; heart failure stage I
The patient was fitted with a pacemaker, her condition improved, and she was discharged.
Based on the nature of the violations, they are distinguished:
- Incomplete blockade. Impulse conduction is slow, but it is preserved. Excitation of the myocardium occurs due to intact branches. This condition occurs in healthy people, but can also indicate pathology. Changes are usually discovered incidentally on an ECG. The patients have no complaints, sometimes there is general weakness and increased fatigue.
- Complete blockade. The impulses do not reach the lower parts of the ventricles. There is a high probability of cardiac arrest due to bradycardia. This condition is accompanied by obvious clinical symptoms.
By type of violation there are:
- Focal changes are observed in certain areas of the myocardium closer to the Purkinje fibers, the impulse partially passes through the ventricles.
- Arborization changes - signal transmission is preserved in all parts of the conduction system, except for its terminal sections.
Features of a two-bundle blockade of the right leg with the left anterior branch
Mechanism of conduction disturbance: the obstacle is located simultaneously in the right leg and the left anterior bundle (branch). The posterior wall and lower part of the left ventricle are the first to be excited through the intact left posterior branch, and the anterior and lateral ones are excited along the anastomotic paths. With a great delay, the impulses reach the right ventricle in a roundabout way. This is the most common variant of intraventricular disorders of the propagation of excitation.
Causes:
- chronic ischemic disease;
- acute widespread myocardial infarction with involvement of the interventricular septum;
- heart defects;
- diffuse sclerotic, inflammatory and degenerative lesions of the ventricles in Lenegra disease (degeneration, calcification and sclerosis of the conduction system inside the ventricles), Lewy disease (fibrous growths in the interventricular septum).
Complications
The cause of intraatrial conduction disturbance is weakness or dysfunction of the sinus node.
The condition threatens with the following consequences:
- Cardiac arrest or asystole. The result of insufficient stimulation of cardiac structures, in particular the muscle layer.
- Heart attack. The result of poor nutrition. Little blood flows through the coronary arteries. Hence acute necrosis or, at least, repeated attacks.
- Stroke. Death of nerve cells and tissues. Ends in death or permanent neurological deficit.
- Cardiogenic shock.
- Fainting and injuries incompatible with life.
- Vascular dementia.
All conditions, one way or another, lead to a minimum of severe disability. There is no point in delaying therapy, if indicated.
Features of the blockade of the right leg with the left posterior branch
Mechanism of conduction disturbance: through the left intact anterior branch, excitation enters the anterior and lateral walls of the left ventricle, then through anastomoses it covers its posterior and lower sections. Last, the impulses reach the right ventricle.
The causes do not differ from the widespread and deep lesions of the left ventricular wall described above. ECG signs combine changes in the chest leads due to blockade of the right leg with a right-sided deviation of the electrical axis.
Visit to the doctor
After a heart attack or other serious cardiac pathology, it is necessary to regularly visit a cardiologist, at least in the first six months. This will allow you to record your condition, identify complications, if any, and promptly eliminate them.
Separately, it is worth noting that any type of this blockade at the initial stage requires increased attention and mandatory consultation with your doctor.
First of all, you should go to a therapist or cardiologist, who can guide you on whether you really should be afraid of this disease, what examinations to undergo, and how to structure your therapy. After all, as we have already noted in this article, this disease can be either completely harmless or seriously threaten your life and health. In the latter case, hospital treatment, possibly surgical intervention, will be required.
Three-bundle blockades
Mechanism of conduction disturbance: when incomplete, the electrical impulse follows from the atria to the ventricles along one of the branches (less affected). In this case, signs of atrioventricular block are detected. Complete block is characterized by third degree atrioventricular obstruction and an altered source of ventricular rhythm.
The causes are severe organic damage to the myocardium, already listed above.
The shape of the teeth indicates the type of intraventricular block
How does conductivity differ on an ECG?
Signs of impaired conduction depend on the type of blockade. They differ in:
- the direction of the electrical axis of the heart;
- the shape of the ventricular complexes;
- place in chest and standard leads;
- width of teeth and intervals.
Sometimes changes in ventricular complexes are not considered specific because they are also present in cases of acute cor pulmonale and right ventricular hyperfunction. Transient blockade simulates ventricular extrasystole.
The two-bundle type of blockade is regarded as a harbinger of the development of a three-bundle lesion. In the three-bundle variant, the shape of the ventricular complexes depends on the location of the source of damage; with partial preservation of conductivity in one of the branches, it resembles the variants of two-bundle blockades. The ECG picture is superimposed on atrioventricular disorders of varying severity.
When assessing the characteristics of blockades, it is important for the doctor to look at previous ECGs to be sure of the age of the changes.
Possibility of death
Therefore, one should be most wary of double-bundle His blockade, which is combined with symptoms of the underlying cardiac disease. In this case, it is necessary to closely monitor the patient's condition, as there is a possibility of death.
If signs of second or third degree AV block appear on the cardiogram, the doctor decides to install a pacemaker. It is important that it be implanted even in patients who do not experience serious attacks, since their lives are still at risk.
It should be noted that, in addition to AV block, intraventricular problems of this nature cause ventricular fibrillation, ventricular tachycardia, which can also lead to a fatal outcome.
Treatment
Stable long-term intraventricular block does not require specific treatment. The initial detection of intraventricular changes, especially in an elderly patient, requires hospitalization and a full examination to determine the causes.
Ischemia suggests the use of coronary lytics and careful use of weak beta-blockers.
If the inflammatory nature of the changes is detected, a course of antibacterial therapy and hormonal agents is carried out.
In case of combination with chronic heart failure, small doses of digitalis and diuretics are used.
It is important to promptly decide on the advisability of installing a pacemaker. This is especially true in cases of two- and three-bundle blocks.
How to determine the prognosis for impaired conduction?
Since conduction pathology is not isolated, but is a consequence of other diseases, prediction is only possible taking into account the clinical course and the effectiveness of treatment of the underlying disease.
Left bundle branch block increases the risk of death by 5 times. Right leg block is not considered a risk factor for heart disease.
Double-bundle disorders precede the transition to complete atrioventricular block annually in 5% of patients. You should be wary of increased conductivity with intermittent types of changes.
If blockades occur during the acute stage of myocardial infarction, the mortality rate increases to 50%. This indicates a widespread focus of necrosis.
Intraventricular conduction cannot be considered in isolation from all cardiac pathology. The type of blockade is important in diagnosis, prescription and choice of treatment.
Symptoms: what most often bothers a person
Intraventricular conduction failure has no specific symptoms. Often this condition remains unrecognized for a long time. The patient does not complain about anything, and the problem is discovered by chance - during medical examination, undergoing a medical examination before starting work or study, serving in the army, before surgery, etc.
Possible signs of pathology:
- feeling of “freezing” in the chest;
- interruptions in the functioning of the heart - the appearance of extraordinary contractions;
- slow heart rate;
- dyspnea;
- feeling of lack of air;
- dizziness;
- worry, anxiety.
As the process progresses, Morgagni-Adams-Stokes syndrome (MAS) develops. At the beginning of the attack, the patient turns pale and loses consciousness. After the condition improves, redness of the skin persists. Such episodes last 1–2 minutes and are caused by insufficient blood supply to the brain due to a sharp decrease in cardiac output. Neurological complications are usually not observed.