Aortic regurgitation is mistakenly taken to be the name of the disease. Some are even trying to find an analogue in the ICD due to lesions of the aortic valves of various natures. Regurgitation is a physical phenomenon caused by the return of fluid flow. When applied to the aorta, it is the reverse flow of blood into the left ventricle. This is the meaning given to the term in functional diagnostics.
If previously experienced doctors could indicate this process only from a subjective point of view (as a result of auscultation and determination of the characteristic noise on the aorta), then with the introduction of ultrasound examination of the heart into practice, it became possible to see the movement of blood in the opposite direction. And the Doppler ultrasound method made it possible to assess the degree of return and connect this diagnostic sign to solving the problem of choosing a treatment method.
Prevalence
Patients with aortic regurgitation are recorded only in functional diagnostic rooms. Therefore, prevalence can be judged in relation to the number of Doppler-examined patients rather than in relation to the total population.
Various degrees and signs of reverse blood flow through the aortic opening are found in 8.5% of examined women and 13% of men. Among all heart defects in adults, chronic aortic regurgitation is detected in every tenth patient. Most often in old age in men.
What anatomical structures are involved in the formation of regurgitation?
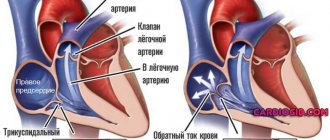
The structure of the four chambers of the heart ensures normal filling of the ventricles (blood flows from the atria) and active ejection into the aorta from the left ventricle, and into the pulmonary artery from the right. The valve system between the cavities and main vessels forms a natural barrier to the return flow.
View of an unclosed aortic opening when the heart is stopped, when valve replacement is required
The physiology of valves, their structure, and muscle bundles for tension react to blood pressure and obey nerve impulses that control the functions of the heart. Any violations of the structure and structure contribute to incomplete closure of the valves. The blood, having passed through the hole, is directed back.
The heart has 4 types of valves between:
- atria and ventricles on the left and right;
- left ventricle and aorta;
- right ventricle and pulmonary artery.
Accordingly, depending on the location of the lesion, mitral regurgitation, return through the tricuspid valve, and incompetence of the valves in the pulmonary artery are possible.
Aortic regurgitation seems to be a special case of dysfunction of the valve apparatus.
Modern methods of treating tricuspid valve insufficiency in children in Israel
The pediatric cardiology department at Hadassah is headed by Dr. Azariah Rein. After receiving higher medical education at the Hebrew University, he trained at the Shaare Zedek Clinic. After receiving his degree, he became a university professor in Jerusalem and Harvard. Permanent member of the Academic Council of Israel, engaged in scientific research.
Cardiac surgery is under the direction of Professor Eldad Erez, holder of two higher qualifications, specializing in the treatment of congenital defects in children. The future doctor of medicine's internship took place in Haifa and Beilinson, his residency in Atlanta (USA), where the doctor mastered the technology of heart transplantation. Erez teaches medical students in Tel Aviv and Jerusalem, and is the author of scientific works.
The first day after hospitalization in the hospital is reserved for examination, medical history, and documentation in Hebrew. Throughout the entire stay in the hospital, the little patient and his parents are accompanied by a Russian-speaking consultant.
Treatment for tricuspid valve insufficiency in children is selected strictly on an individual basis and depends on the degree of regurgitation of blood flow (1, 2, 3 or 4):
- 1 - subtle throw or touch of the tricuspid valve;
- 2 — reverse ejection is determined at a distance of 2 cm from the atrioventricular opening;
- 3 — return of blood from the right ventricle to a distance of more than 2 cm;
- 4 - regurgitation in the right atrium over a significant extent.
The first stage may be limited to medical observation or conservative therapy. Starting from the second, the nature of the intervention will depend on the intensity of casting, complications caused by the defect, and the presence of combined anomalies.
Elimination of the defect and the consequences of improper functioning of the heart is carried out through medication or surgery.
Drug therapy
The conservative approach includes drugs that ease the work of the heart and reduce pulmonary hypertension. This list includes diuretics, anticoagulants, b-blockers, glycosides, drugs that increase metabolism, and ACE inhibitors.
Surgical intervention
The main types of surgical techniques are repair of the patient's own valve or prosthetics using a bioprosthesis or a mechanical analogue.
Indications for prosthetics are considered to be severe changes in the valves. The material for the manufacture of a biological prosthesis is the aorta of an animal (pig). Unlike a mechanical one, a bioprosthesis significantly reduces the development of thromboembolism, but lasts only 10 years, requiring repeated replacement.
Preference is given to plastic correction, but only if no pronounced changes in the structure of the valves are detected. The obvious advantages of this procedure are minimal postoperative complications and a reduction in the rehabilitation period. In addition, restoration using one’s own, normally functioning tissues increases resistance to infections and eliminates the need for constant use of special medications.
The mechanism of regurgitation in normal and pathological conditions
Cardiologists identify minor physiological regurgitation, which is possible under normal conditions. For example, 70% of tall adults have incomplete closure of the tricuspid valve, which the person is not aware of. Ultrasound reveals slight swirling flows when the valves are completely closed. This does not affect general blood circulation.
Pathology occurs during inflammatory processes:
- rheumatism,
- infective endocarditis.
Most typical for mitral localization, the formation of heart disease. It should not be confused with prolapse (stretching and bending of the valves into the atrium). It is with prolapse that physiological regurgitation often occurs and is found in growing children and adolescents. It is taken into account as a possible cause of extrasystole. The child must be observed by a cardiologist and re-examined. No special treatment is required.
The formation of scars after an acute heart attack, against the background of cardiosclerosis, in the area approaching the valve leaflets and threads, leads to breakdown of the necessary tension mechanism and changes the shape of the leaflets. Therefore, they do not completely close.
In a pathological process, an equally significant role is played by the diameter of the outlet, which must be blocked. Significant enlargement due to left ventricular dilatation or hypertrophy prevents the tight junction of the aortic valve leaflets.
Auscultation
On auscultation, the first heart sound (S1) may be normal or weakened if a tricuspid regurgitation murmur is present. The second heart sound (S2) may be split (with a loud pulmonary component [P2] in pulmonary hypertension) or single due to rapid closure of the pulmonary valve, combined with P2 and an aortic component (A2). A third RV heart sound (S3) may be heard near the sternum in RV-induced HF.
Often the noise with TN is not heard. Although it is obvious that this is a holosystolic murmur, it is better heard on the left middle or lower border of the sternum, or if the stethoscope is placed in the epigastrium when the patient is sitting upright or standing. The murmur may be high-frequency if TN is functional or caused by pulmonary hypertension, or mid-frequency if TN is severe and has other causes. If there is no murmur, the diagnosis is best made by the nature of the pulse wave in the jugular vein and the systolic pulsation of the liver. The noise changes with breathing, intensifying with inspiration (Carvallo's sign).
In part, a person may not always know about problems that have arisen in the heart. And if any of the described symptoms suddenly appear, you should immediately consult a doctor for an examination, during which tests are taken and hardware diagnostics are performed.
Regurgitation can become an acquired disease, but sometimes there are congenital cases. Changes in the heart occur during the intrauterine development phase of the fetus. This deviation from the norm appears in infants immediately after birth:
- In a newborn, pronounced cyanosis can be observed.
- There are breathing disorders.
- Examination reveals right ventricular failure.
The disease is so serious that it can lead to the death of a child. This is why it is so important to examine the fetus before birth.
Table of characteristic symptoms at different stages of pathology:
| Stage of tricuspid regurgitation | Symptoms of the disease |
| First | Absent or may appear as excessively intense pulsation of the veins in the neck. |
| Second | The neck veins are noticeably pulsating and trembling. |
| Third and fourth | Swelling of the jugular vein. Blueness of the skin on the lips, nose, under the nails. Swelling of the lower extremities. Atrial fibrillation. Shortness of breath, fatigue during physical activity (as it progresses, it is also diagnosed at rest). Pain in the right hypochondrium. Enlarged liver. |
Most of the signs are similar to other cardiovascular diseases, but the most clear indication of tricuspid valve regurgitation is swollen jugular veins and the development of atrial fibrillation.
Main valvular causes of aortic regurgitation
The causes of damage to the aortic valves, the diameter of the hole between the left ventricle and the initial part of the aorta, are:
- rheumatic inflammation localized along the line of valve closure - tissue infiltration at the initial stage leads to wrinkling of the valves, forming a hole in the center for the passage of blood during systole into the cavity of the left ventricle;
- bacterial sepsis with damage to the endocardium and aortic arch;
- warty and ulcerative endocarditis in severe forms of infection (typhoid fever, influenza, measles, scarlet fever), pneumonia, cancer intoxication (myxoma) - the valves are completely destroyed;
- congenital defects (formation of two leaflets instead of three) involving the aorta, large ventricular septal defect;
- specific autoimmune processes in the ascending aorta in chronic syphilis, ankylosing spondylitis, rheumatoid polyarthritis;
- hypertension, atherosclerosis - the process of compaction of the valves with the deposition of calcium salts, expansion of the ring due to dilatation of the aorta;
- consequences of myocardial infarction;
- cardiomyopathy;
- chest injuries with rupture of the muscles that contract the valves.
Bicuspid aortic valve is considered a type of congenital defect and increases the risk of regurgitation
The reasons include complications of treatment of heart diseases using catheter radiofrequency ablation, as well as cases of destruction of the biological valve prosthesis.
Classification
We found that tricuspid valve regurgitation can be congenital or acquired, primary (organic) or secondary (functional) by etiology. Organic failure is expressed by deformation of the valve apparatus: thickening and wrinkling of the valve leaflets or their calcification. Functional failure occurs when valve dysfunction is caused by other diseases and is manifested by rupture of the papillary muscles or chordae tendineae, as well as disruption of the annulus fibrosus.
Causes associated with aortic damage
The portion of the aortic arch closest to the heart is called the aortic root. It is its structure that influences the “health of the valves” and the width of the gate ring from the left ventricle. Root lesions include:
- age-related or degenerative changes causing dilatation;
- cystic necrosis of the middle layer of the aorta in Marfan syndrome;
- dissection of the aneurysm wall;
- inflammation (aortitis) with syphilis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis;
- giant cell arteritis;
- malignant hypertension.
Among the reasons, a negative effect of drugs used to reduce appetite in obesity was found.
Consequences of aortic regurgitation
The return of blood to the left ventricle inevitably leads to its expansion and increase in volume. Possible expansion of the mitral annulus and further enlargement of the left atrium.
At the point of contact of the blood flow, “pockets” are formed on the endocardium. The greater the degree of regurgitation, the faster the left ventricular overload develops.
Studies have shown the meaning of heart rate:
- bradycardia increases the volume of return flow and promotes decompensation;
- tachycardia reduces regurgitation and causes greater adaptation.
Risk factors
They do not directly cause tricuspid regurgitation, but lead to the onset of the pathological process:
- Long-term smoking.
- Consuming alcohol in immoderate quantities.
- A long period of immobilization, without the possibility of vigorous activity. Development takes a long time, from six months or more.
- Drug addict.
- Excessive use of “dangerous” drugs: glycosides, antiarrhythmics, progestin agents, also hormonal medications, broad-spectrum antibiotics.
- Harmful working conditions affect chemical, hot production, and mines.
The reasons are considered as a whole; a system of development factors is possible.
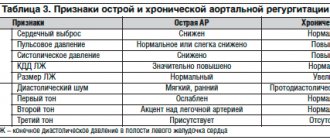
Forms of aortic regurgitation
It is customary to distinguish between acute and chronic aortic regurgitation.
Features of the acute form
Typical causes of acute aortic regurgitation are:
- injuries;
- dissecting aneurysm;
- infective endocarditis.
The volume of blood entering the left ventricle during diastole increases suddenly. Adaptation mechanisms do not have time to develop. The load on the left side of the heart and myocardial weakness increases sharply. Insufficient blood volume is released into the aorta to support general circulation.
Patients develop signs of pulmonary edema and cardiogenic shock. Symptoms are very severe when hypertension and aortic aneurysm dissection are combined.
Features of chronic aortic regurgitation
A distinctive feature of the chronic form is sufficient time for the full activation of compensatory mechanisms and adaptation of the left ventricle. This causes a period of compensation for circulatory disorders. Myocardial hypertrophy helps compensate for the reduced output.
When reserve energy reserves are depleted, a stage of decompensation occurs with severe heart failure.
List of sources
- L.A. Boqueria, O.L. Bockeria, E.R. Jobava review article “Functional mitral regurgitation in atrial fibrillation”, 2015
- Mashina T.V., Golukhova E.Z. Left ventricular diastolic dysfunction in patients with atrial fibrillation: pathogenetic mechanisms and modern ultrasound assessment methods (analytical review). Creative cardiology. 2014
- Karpova N.Yu., Rashid M.A., Kazakova T.V. , Shostak N.A. Aortic regurgitation, Regular issues of “RMZh” No. 12 from 06/02/2014
Clinical manifestations
In the acute form of aortic regurgitation, the patient suddenly exhibits signs of cardiogenic shock:
- severe weakness;
- pale skin;
- severe hypotension;
- dyspnea.
For pulmonary edema:
- the patient is suffocating;
- breathing is noisy and hoarse;
- when coughing, foamy sputum mixed with blood is released;
- face, lips, limbs are cyanotic;
- heart sounds are sharply muffled;
- A lot of moist rales are heard in the lungs.
With chronic aortic regurgitation, a long asymptomatic period is possible. Symptoms appear only with the development of myocardial ischemia and severe cardiac decompensation. The patient notes:
- shortness of breath on exertion;
- strong heartbeats;
- extrasystoles;
- angina attacks at night;
- a “cardiac asthma” clinic is possible.
During the examination, the doctor notes:
- shaking the head in rhythm with the pulsation of the heart;
- a typical pulse on the radial artery is a sharp shock wave and an immediate fall;
- trembling when palpating the chest at the base of the heart;
- expansion of the left cardiac border;
- pulsating carotid arteries;
- diastolic murmur on the aorta, along the left edge of the sternum in the third and fourth intercostal spaces, is better heard in a sitting position with a slight bend forward, the first sound is clapping.
How is the disease classified?
In medical practice, four main degrees of tricuspid regurgitation are known:
- The return of blood flow is carried out in a minimal volume. The clinical picture and symptoms are not traceable, so no patient has ever experienced discomfort in such a situation.
- The return of blood flow is performed within a range of several centimeters from the inner walls. There are also no signs of the development of the disease, however, an increase in pulse rate in the area of the jugular veins may indicate this disorder.
- At this stage of the disease, blood flow is released beyond 2 cm in the valve. The patient feels a powerful pulsation in the vessels located in the neck, a noticeably rapid heartbeat, sweetness throughout the body, a deterioration in general well-being and a decrease in activity even with minor physical activity. Shortness of breath often occurs.
- Blood flows back through the valve into the right atrium. The patient's general condition may worsen, his health may deteriorate, heart failure may develop, swelling in the legs may appear, pulmonary hyperplasia may be observed, the heartbeat will increase, and the sensitivity of tactile sensations in the limbs will decrease. In such a situation, the liver often increases in size, ascites is diagnosed, and the stomach hurts.
We can conclude that in the first two stages of the disease, patients may not notice changes in their own body at all, but the transition to the third stage of the disease immediately noticeably changes their normal lifestyle. For this reason, cardiologists advise everyone to undergo a medical examination annually to prevent the subsequent development of the disease if it is detected.
Diagnostic methods
Indirect signs of aortic regurgitation are noted in:
- chest x-ray - the left contour of the cardiac shadow is expanded to the side and down, the expansion of the aortic arch is similar to an aneurysm, there are clear signs of enlargement of the left atrium, calcifications may be detected in the aortic arch;
- electrocardiogram - overload of the left chambers of the heart is revealed.
Deviation of the electrical axis to the left, a characteristic change in the shape of the ventricular complexes in leads I, AVL, V3-V6, negative T waves
Echocardiographic method
In the diagnosis of regurgitation, echocardiography serves as the main objective method; it allows one to determine the cause, the degree of regurgitation, the sufficiency of compensatory reserves, and circulatory disorders even in the asymptomatic stage of the disease with minimal disturbances. It is recommended for patients in the initial stage annually, and twice a year when clinical symptoms appear.
The calculations take into account the surface area of the patient's body, due to the lack of pronounced expansion of the ventricular chamber in short people.
The most commonly used mode is color Doppler scanning. The sensors are installed in such a way as to measure the area of blood flow at the aortic valves, in the initial part of the aorta, and compare it with the width of the passage. In severe cases, it exceeds 60% of the ring diameter.
The device allows you to record the time interval of the wave and establish the expansion of the left ventricle
In the practice of cardiologists, a division of the return jet into 4 degrees is used in relation to its length to the size and internal formations of the left ventricle:
- 1 - does not extend beyond half the length of the anterior leaflet at the mitral valve;
- 2 - reaches or crosses the gate;
- 3 - the flow value approaches half the length of the ventricle;
- 4 - the jet touches the top.
The definition of regurgitation depends on the area (width) of the jet, its location, the level of loss of blood ejection from the left ventricle, and the volume per contraction. Based on quantitative indicators, they are conventionally divided into mild, moderate and severe forms.
If information from Doppler sonography is not enough, the following is carried out:
- magnetic resonance imaging;
- radionuclide angiography;
- cardiac catheterization.
Who is indicated for surgical treatment?
The only form of surgery is aortic valve replacement. The operation is indicated for:
- severe form of regurgitation with impaired left ventricular function;
- if the course is asymptomatic, with preserved ventricular function, but pronounced expansion (dilatation).
Aortic valve replacement surgery is often combined with coronary artery bypass grafting.
Forecast
The prognosis for the patient’s life depends on the underlying disease, the degree of regurgitation, and the form. An early mortality rate is typical for the acute development of pathology. In the chronic form, 75% of patients live more than 5 years, and half live 10 years or longer.
In the absence of timely surgical intervention, the development of heart failure is noted in the next 2 years.
Treatment of moderate clinical symptoms is accompanied by positive results in 90% of patients. This reinforces the importance of evaluating and monitoring patients with aortic regurgitation.