Violations of intraventricular conduction according to the electrocardiogram are quite often encountered at a doctor’s appointment, not only in cardiac patients, but also in absolutely healthy individuals. But in order to determine whether this is a manifestation of cardiac pathology or a variant of the norm, it is necessary to take into account a number of factors.
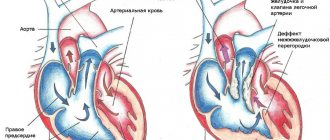
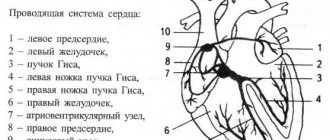
Normally, electrical impulses are conducted through the heart muscle from the atrial myocardium to the ventricular myocardium along specific fibers combined into the bundles of His (right and left). Along the most branched fibers, called Purkinje by the author, electrical excitation covers the most distant areas of the right and left ventricles.
the work of the conduction system of the heart - the impulse from the sinus node is “conducted” first through the atria, then through the ventricle of the heart
But the contractions of the heart parts may not always be harmonious and coordinated. Most people over forty years of age have certain deviations from the norm in the form of rhythm and conduction disturbances.
violation of intraventricular conduction - the passage of an impulse along one or more of the branches of the His bundle is blocked
How to distinguish whether it is normal or pathological?
So, in order to understand whether a violation of intraventricular conduction in a particular patient is normal or pathological, the following nuances should be taken into account:
Age
As a rule, nonspecific intraventricular conduction disorders can appear in people of any age. But at a young age there are usually no serious reasons for conduction disorders. That is, the younger the person, the more likely it is that the disorders are caused by functional characteristics that do not require treatment.
Concomitant cardiac pathology
If the patient has serious heart problems, conduction disorders are organic in nature, that is, there are significant obstacles to the path of electrical excitation. Usually this is cicatricial deformation of muscle fibers (after heart attacks, myocarditis) or hypertrophy of muscle fibers due to hypertension, heart defects, and coronary artery disease. Thus, local conduction disturbances in patients with a history of heart disease are always pathological in nature and cannot be regarded as a normal variant.
Particular attention here should be paid to complete left bundle branch block (LBBB), in which it is almost impossible to properly interpret the cardiogram. With this pathology, the ventricular complexes on the ECG are so deformed that it is extremely difficult to assess ischemia and necrosis (in case of a heart attack). That is why suddenly occurring PBLNP, especially in combination with pain in the chest, should be regarded by a doctor as a suspicion of acute myocardial infarction, with an appropriate examination, according to the standards.
Premorbid background
In patients with certain diseases, the likelihood of organic heart damage increases significantly. Thus, with diabetes mellitus, especially insulin-dependent diabetes, with obesity, with hypercholesterolemia, the risk of developing coronary heart disease, hypertension and heart attack increases significantly. Therefore, patients with the listed diseases, combined with local disturbances of intraventricular conduction, require regular medical supervision and, if necessary, treatment.
Reversible factors
This, first of all, should include taking certain medications - cardiac glycosides (digoxin), antiarrhythmics (beta blockers, etacizine, sotalol, etc.). It happens that these drugs are indicated for a patient to take regularly, for example, with sinus tachycardia, with atrial fibrillation, but as a result of their use, the conduction of impulses through the ventricles is affected. If the drugs are discontinued, intraventricular conduction disturbances disappear.
Improper lifestyle - smoking, alcohol abuse - have an extremely negative effect on the conduction system of the heart. Smokers often experience incomplete and complete blockades of the right bundle branch, which do not have a significant effect on the contractions of the heart as a whole.
Professional sports inevitably lead to the formation of hypertrophy of the heart muscle - the so-called “athletic heart” is formed. In professional athletes, the heart rate rarely exceeds 55-60 beats per minute, and this is due precisely to the delay in the conduction of impulses through the myocardium. Intraventricular blockades in athletes require only medical supervision and are not considered a pathology.
Intraventricular conduction disorders of the heart in childhood
In children, blockades are congenital in nature, and in the absence of congenital cardiac pathology, therapy is not required. Most often, conduction disorders are caused by a patent foramen ovale (very common in recent years), which does not have a significant effect on the functioning of the baby’s heart. However, a child with cardiac conduction disorders, even partial ones, must be regularly monitored by a pediatric cardiologist with an annual ECG and cardiac ultrasound (Echo-CS).
Two- and three-bundle blockades are considered dangerous in children, as in adults, and clinical manifestations of which may require medical or surgical treatment. Usually these blockades are accompanied by congenital cardiomyopathy, or heart defects.
Atrioventricular block
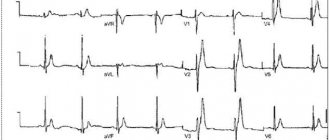
Signs of 1st degree atrioventricular block are prolongation of the PQ interval by more than 180 ms (for adult patients). Atrioventricular block of the 2nd degree is the loss of part of the ventricular complexes. If the loss is preceded by a gradual lengthening of the PQ interval, this is called the Samoilov-Wenckebach periodicity. The next degree of impairment of AV conduction is 3rd degree AV block (AV dissociation), in which the atria contract in one rhythm and the ventricles in another.
↓Atrioventricular block 1st degree. Atrial P waves begin immediately after T waves, and the duration of the PQ interval is impressive.
↓Episode of 2nd degree AV block without Samoilov-Wenckebach periodicity (equal PQ intervals before loss of QRS). “Lonely” P wave without subsequent QRS complex. Escaping contraction from the AV node after blockade (there is no atrial P wave before it). And also - early repolarization syndrome.
↓An episode of 2nd degree AV block with Samoilov-Wenckebach periodicity - a gradual lengthening of the PQ interval before the QRS loss and a return to normal PQ after the loss are visible.
↓Picture of 3rd degree AV block (AV dissociation): atrial P waves occur at one frequency, and ventricular complexes from the AV node are at a completely different frequency. Note the third QRS complex. The atrial P wave is between the complex and the T wave. The maximum PQ interval in this recording is 1.15 seconds.
What conduction disorders are most dangerous?
Intraventricular conduction disorders are divided into the following types:
- incomplete blockade of the right/left bundle branch,
- complete blockade of the right/left bundle branch,
- bifascial (two-bundle) blockade (right and one of the branches of the left),
- trifascial (three-bundle) blockade.
An isolated conduction disorder along one of the branches does not pose a threat to the life and health of the patient, but damage to two and three branches are potentially dangerous conditions. Firstly, this is because such disorders in most cases arise due to organic damage to the heart muscle (listed above), which in itself is already life-threatening. And secondly, a block along two and/or three bundles can lead to such a rare heartbeat that the patient may require implantation of a pacemaker.
Complete blockade of LBP is dangerous because it can aggravate the course of coronary heart disease, and in the event of the development of acute myocardial infarction, mask its manifestations on the ECG. In such cases, the doctor’s tactics boil down to regarding the first-time occurrence of LBBB on the background of chest pain as a possible acute infarction.
What symptoms should you look out for?
Usually, a violation of intraventricular conduction does not manifest itself in any way if it is a block of the right leg or one of the branches of the left is blocked. In cases of two- or three-bundle block, symptoms occur more often, but they are caused by the underlying cardiac pathology. This could be pain in the heart area, interruptions in heart function, increased blood pressure, etc.
Symptoms of blockades themselves occur in the case of a rare heartbeat (less than 50 per minute) and are expressed in the form of dizziness, flashing spots before the eyes, severe general weakness, lightheadedness or loss of consciousness. These symptoms are regarded as equivalents or attacks of MES (Morgagni-Edens-Stokes). They occur due to a sharp decrease in blood flow to the brain. Such symptoms require immediate medical attention. Remember! A rare pulse combined with loss of consciousness requires treatment in a cardiology or therapeutic hospital!
How does it appear on an ECG?
Usually in the cardiogram protocol the patient sees a conclusion of this kind - conduction along the right/left bundle branch is impaired, or complete/incomplete blockade. The specialist sees the following changes:
- The complexes in the leads showing the right/left ventricles are deformed, widened, the R and S waves do not correspond to the normal teeth. The rhythm may remain within normal limits, or be rare or frequent, depending on whether there are concomitant cardiac arrhythmias.
What it is
Normally, the impulse originates in the sinus node of the right atrium - where the superior vena cava flows into it.
Next, the wave travels through the atria and ends up at the next control point - the atrioventricular localization node. From here the excitation goes through the His bundle and gradually spreads to the apex. His fibers are special cells of the interventricular septum that form three branches. The right bundle branch (RBBB) delivers signals to the walls of the right ventricle. Along the left (LNPG), which is divided into anterior and posterior branches, there is coverage of the left ventricle. At the end, the branches divide into Purkinje fibers. This structure allows the impulse to be transmitted without loss and ensures uninterrupted heart function.
Conduction is slow and impaired - is there a difference?
In a healthy organ, impulses move from top to bottom in a set rhythm, with the required speed. With pathology, their conduction is slowed down or disrupted. If the passage of the signal is inhibited, excitation reaches the end point, but this process occurs at a slower speed. If conduction is disrupted, the impulse is interrupted in a certain area or is completely absent.
Impairment and slowing of intraventricular conduction occur at different ages. We cannot unambiguously estimate how often this pathology is detected. Failures in the conduction system of the heart often remain asymptomatic and are detected accidentally during a preventive examination. According to the medical literature, various types of conduction disorders are diagnosed mainly after 50 years (5–7% of cases). At 60–70 years of age, the frequency of detection of such conditions reaches 30%.
Failure of intraventricular conduction belongs to the group of bradyarrhythmias. Intra-atrial conduction disorders belong to this category. The causes and symptoms of the development of these conditions are similar. An accurate diagnosis can only be made after an examination.
What additional examination is necessary?
Typically, for intraventricular conduction disorders, an examination plan is required only if the patient has a concomitant pathology. For previously healthy young people, an annual ECG as part of a medical examination is sufficient.
In case of concomitant pathology (hypertension, ischemia, diabetes mellitus, heart defects, etc.), as well as in case of complaints from the heart or other organs, further examination is mandatory! This plan should include the following studies:
- general blood test (in case of dizziness and loss of consciousness, there may be a low level of hemoglobin),
- biochemical blood test (diagnostic search in terms of pathology of internal organs),
- determination of cholesterol and lipid levels in the blood (diagnosis of coronary heart disease)
- determination of fasting blood sugar (suspected diabetes mellitus),
- fibrogastroscopy (stomach pathology can often be accompanied by disturbances in heart rhythm and conduction),
- daily monitoring of blood pressure and ECG (Holter) for hypertension and other rhythm disturbances, especially with transient complete block of the bundle branches,
- Echo-CS (ultrasound of the heart) for suspected or confirmed diagnosis of heart defects, cardiomyopathy, post-infarction and post-myocardial cardiosclerosis, which are often the cause of conduction disorders in the ventricles of the heart.
Do cardiac conduction disorders need to be treated?
There is no independent treatment for intraventricular conduction disorders. If blockades are registered in healthy people, no specific treatment is required. In the case of a causative disease, observation by a cardiologist or a therapist is required, with regular use of prescribed medications.
Complete blockade of the left bundle branch deserves special attention . It was already mentioned above that this pathology is never a variant of the norm, unlike the right blockade
, and is always caused by organic heart diseases (previous myocarditis, heart attacks, myocardial hypertrophy with hypertension, etc.). The doctor’s tactics when PLBBB is first detected is a full examination, and if combined with pain in the chest, the patient should be treated as if it were an acute myocardial infarction.
***
Thus, it is possible to determine whether a violation of intraventricular conduction is a normal variant or a pathology only after interpretation of the cardiogram by a therapist or cardiologist. But if the patient has not previously noted any chronic diseases, and at the moment he is not bothered by certain complaints, conduction disturbances (except for complete blockade of LBP, two- and three-bundle blockades) can be regarded as individual characteristics.
Sinoatrial blockade
Strictly speaking, it is impossible to accurately prove the fact of sinoatrial block (failure to conduct an impulse from the sinus node to the atria) due to the absence of ECG events. An indirect sign is an increase in RR quite exactly twice as compared to the previous one and the absence of a P wave at the moment of the pause. Sinoatrial blockade differs from the Holter recording of pronounced sinus arrhythmia according to the rhythmogram (after the blockade, RR becomes the same, and with sinus arrhythmia it decreases gradually.
↓Presumably an episode of sinoatrial block (look at the heart rate numbers at the top of the picture).
↓Another presumptive episode of sinoatrial block (look at the RR duration numbers at the top), after which first-degree atrioventricular block occurred (prolongation of the PR interval).