At risk
- Patients with acute myocardial infarction, especially in the first hour of the development of a heart attack (it should be noted that sudden death that occurs in the early (acute) phase of myocardial infarction, verified clinically or at autopsy, is regarded as “death from a heart attack.” However, according to its mechanisms , clinical picture and complex of necessary resuscitation measures, it fully corresponds to sudden cardiac death that develops in other forms of coronary heart disease, and is therefore discussed in this section).
- Patients with heart failure
- Patients with a history of myocardial infarction, especially those with cardiomegaly and congestive heart failure
- Patients with coronary heart disease with high grade ventricular arrhythmias
- Patients with coronary heart disease who have several main risk factors: arterial hypertension, left atrial hypertrophy, smoking, disorders of carbohydrate and fat metabolism, etc.
- Patients with any heart disease accompanied by severe myocardial hypertrophy (for example, HCM, aortic stenosis, etc.)
- Patients with cardiogenic shock of any origin (other than acute MI)
- Patients with cardiac tamponade of any origin (for example, with exudative pericarditis, etc.)
- Patients with pulmonary embolism
- Patients with long QT syndrome and other channelopathies
Medical Internet conferences
Introduction
Diseases of the cardiovascular system occupy one of the leading places in the structure of morbidity among the population of Russia and determine the level of its mortality, temporary and permanent disability. In 50% of cases, deaths from such a common disease as coronary heart disease (CHD) are sudden, primarily arrhythmogenic in nature [1].
Sudden cardiac death (SCD) is a nonviolent death characterized by sudden loss of consciousness within one hour of the onset of acute symptoms. SCD is among the pressing problems of our time. In the Russian Federation, according to estimated data, the incidence of SCD is 450 - 600 thousand people annually. In European countries, about 2,500 people die from SCD every day, and 2–5% of cases occur in medical institutions. About 1/3 of patients with IHD die suddenly, but most often SCD is recorded during the first year after the development of myocardial infarction (MI) [2-5].
Estimates for the United States are largely based on retrospective death analyzes and emergency department databases (200,000 to 450,000 BCCs per year). This explains the frequency of 0.1–0.2% per year among the population over 35 years of age [6]. The most unfavorable areas with regard to the epidemiology of IHD were observed in the European part of Russia and Siberia. In the south of Russia, IHD was detected 3–4 times less frequently [7].
In one of the regions of the globe - the eastern part of Finland - the highest incidence of sudden coronary death (SCD) in the world is registered, this is due to a deficiency of magnesium and selenium in the soil and drinking water. Magnesium is known for its antispasmodic effect on smooth muscle. The biological effect of selenium is associated with its antioxidant properties, mediated through the enzyme glutathione peroxidase; selenium is included in the prosthetic group.
According to the Framingham Study, more than half of deaths from a primary heart attack in people aged 45 to 74 years are sudden. SCD is the leading cause of death in men aged 20–64 years and accounts for 32% of all deaths [8]. About 50% of all deaths from SCD are sudden and unexpected and occur within a very short time of the onset of changes in the patient's clinical status [9].
Risk factors for SCD
The most important risk factors for SCD are the presence of malignant ventricular arrhythmias and decreased left ventricular contractility. Of the ventricular arrhythmias, the most dangerous are atrial fibrillation and ventricular flutter, which cause circulatory arrest [10].
Risk factors for SCD: family history of coronary heart disease, older age, male gender, increased levels of total cholesterol, low-density lipoproteins, arterial hypertension, smoking and diabetes mellitus, as well as alcohol abuse.
Age
As is known, the atherosclerotic process begins in childhood. Autopsy data confirm that atherosclerosis progresses with age. Even at a young age, coronary heart disease is one of the 10 leading causes of death in the United States. At the age of 55 - 65 years, the cause of death for males is coronary heart disease.
Floor
In one of the large studies, at the age of 30 - 39 years, atherosclerosis of the coronary arteries was detected in 5% of men and in 0.5% of women, at the age of 40 - 49 years, the frequency of atherosclerosis in men is three times higher than in women, at the age of 50 - 59 years in men it is twice as high; after 70 years, the frequency of atherosclerosis and ischemic heart disease is the same in both men and women. In women aged 40–60 years, atherosclerotic changes occur 3 times less frequently than in men. This is due to the fact that normal ovarian function “protects” women from atherosclerosis. In postmenopausal women, estrogen levels decrease and, at the same time, low-density lipoprotein levels increase.
Genetic factors
People whose parents or family members have symptomatic coronary heart disease are at increased risk of developing the disease. The associated increase in relative risk varies widely and may be up to 5 times higher than in individuals whose parents and close relatives did not suffer from cardiovascular disease. Hereditary factors contribute to the development of dyslipidemia, arterial hypertension, diabetes mellitus, obesity, leading to the development of heart disease.
Smoking
Smoking has been proven to be one of the risk factors for SCD. Smoking is of great importance not for the immediate, but for the long-term prognosis. Smoking affects both the development of atherosclerosis and the processes of thrombus formation. Cigarette smoke contains nicotine and carbon monoxide, which have a negative effect on the functioning of the cardiovascular system.
Mechanisms of increased risk:
- increased myocardial oxygen demand;
- reduces the oxygen transport function of the blood, as well as the delivery of oxygen to the heart due to the formation of carboxyhemoglobin;
- disrupts aerobic metabolism in the myocardium;
- has a negative inotropic effect.
- reduces plasma high-density lipoprotein cholesterol levels;
- increases platelet adhesiveness and the tendency to thrombus formation.
Previous myocardial infarction
MI is an important risk factor for SCD. Potential risk of SCD in the first 72 hours from the onset of MI. The highest risk of SCD is observed in patients with MI in the period of the first three days to 8 weeks, if the course of MI was complicated by ventricular tachycardia, atrial fibrillation, paired, volley, early ventricular extrasystoles. In the post-infarction period, important predictors of sudden cardiac death are impaired myocardial contractile function and heart rhythm (ejection fraction <30% and ventricular extrasystoles with a frequency of 10 - 30 per hour). The combination of these factors increases the risk of sudden cardiac death by up to 20% per year. The presence of a left ventricular aneurysm, its pronounced hypertrophy, as well as ventricular fibrillation that occurred in the acute period of myocardial infarction also increases the risk of SCD.
Left ventricular myocardial dysfunction
Decreased contractile function of the left ventricular myocardium is one of the main risk factors for sudden cardiac death. A reduction in ejection fraction of less than 40% is critical. After the onset of congestive heart failure of various origins, the risk of SCD is very high and can be 35–40% [11].
Genetic basis of SCD
A number of recent studies pay much attention to the genetic determinants of the development of VCS [12, 13]. SCD may be caused by inherited genetic abnormalities that affect the synthesis of proteins involved in the formation and operation of ion channels and pumps responsible for electrophysiological processes occurring on the cell membrane. These diseases include some congenital variants of the long QT interval syndrome (Jervell-Lange-Nielson syndrome, Romano-Ward syndrome, Brugada syndrome, hypertrophic and dilated cardiomyopathies, arrhythmogenic dysplasia of the right ventricle, catecholergic polymorphic ventricular tachycardia). These are the most well-known hereditary diseases today, associated with a defect in one gene (monogenic diseases), predisposing to the development of SCD [14-16].
The causes of SCD in patients with Marfan syndrome are aortic dissection and rupture. About 2% of deaths are associated with aortic rupture and dissection [17,18].
Patients with aortic rupture account for no more than 7% of the total number of patients with aortic dissection. One of them, which included 500 people who survived cardiac arrest, showed that a family history of SCD is an independent risk factor for SCD, increasing its likelihood by 1.75 times [19].
BCC formula
Rhythm disturbances also play a role in the genesis of SCD, but they are by no means the only ones. In addition, there must be disability of the heart muscle, and there must also be exposure to a factor that leads to the occurrence of SCD.
BCC formula: BCC = substrate + trigger factor.
The substrate is an anatomical and electrical abnormality associated with acquired or congenital heart disease. Trigger factors include: metabolic, ischemic, mechanical influences. This formula may help identify patients at increased risk of developing SCD and thereby reduce the incidence of SCD.
Diagnosis of SCD
According to the monograph by V.G. Kudryashova [20] “Sudden cardiac arrest”, the main “symptoms - harbingers” of cardiac arrest are:
- Sudden pallor or cyanosis of the skin, especially the face;
- Acute arterial hypotension (blood pressure below 60 mm Hg);
- Sudden rare bradycardia (heart rate less than 40 per minute);
- Supraventricular and ventricular tachycardia (heart rate more than 120 per minute, occurring in paroxysms);
- Ventricular extrasystoles: single or group extrasystoles, allorhythmias of the bigeminy type;
Group extrasystole creates all the conditions for the development of VF; there are situations when even a single ventricular extrasystole can cause VF.
The clinical manifestations of this complication are almost always the same:
- Absence of pulse in the central arteries (carotid or femoral).
- Loss of consciousness and development of convulsive syndrome (after 10 - 20 seconds).
- Stopping breathing (after 15 - 30 seconds).
- Bilateral mydriasis (after 60 - 90 seconds) [20].
SCD and physical activity
Two aspects of this problem are of interest: the development of complications during functional tests and rehabilitation of patients [21]. Death from SCD is recorded in patients who can perform light exercise. According to a retrospective analysis of the parameters of the frequency spectrum R - R - distribution, when conducting a stress test in the group of patients who had SCD, but the study did not reveal structural changes in the myocardium, they did not differ from the values in the group of conditionally healthy individuals. In addition to ST segment depression, prolongation of the QRS complex was also found as a risk factor for the development of ventricular fibrillation [22].
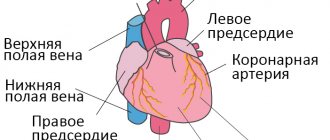
Pathomorphological changes in SCD
In the majority of people who suddenly die from coronary artery disease, significant stenosis of two or three coronary arteries is detected. Damage to one vessel is rarely detected - mainly in people under 40 years of age. The atherosclerotic process affects extramural arteries; intramural ones are rarely affected. At the same time, in patients who have suffered from arterial hypertension for a long time, the lumen of the intramural arteries usually decreases due to hypertrophy of the muscle fibers of the media and proliferation of the internal elastic membrane of the wall.
Occlusive thrombosis of the coronary arteries is detected in 10–15% of cases. In the majority of sudden deaths, morphological examination does not reveal acute changes in the vessels of the heart. In a histological study of cross sections of the coronary arteries, Z. I. Yanushkevicius et al. found fresh occlusive lesions in 84 cases. In 52% of cases, fresh thrombosis was combined with an organized thrombus, and ulcerations, ruptures of the atheromatous plaque, and parietal and occlusive thrombi were detected [23].
Prevention of SCD
Preventive measures are carried out in patients with an increased risk of SCD. Since SCD is a multifactorial syndrome, various directions are used for its prevention, ensuring an adequate level of reperfusion, limiting the scar zone, modulating neurohumoral influences, stabilizing the atherosclerotic plaque, antiarrhythmic and antifibrillatory activity. There are directions in the prevention of SCD - these are drugs without their own electrophysiological activity, today these include ACE inhibitors, aldosterone receptor blockers and lipid-lowering drugs containing a high concentration of gamma-3 polyunsaturated fatty acids. Another direction is associated with the use of drugs that have certain electrophysiological properties, including beta blockers and amiodarone [24].
The prophylactic use of antiarrhythmic drugs is based on the ability of the drugs to suppress ventricular arrhythmias that contribute to the initiation of VF and to increase the electrophysiological stability of the myocardium [25].
Primary prevention
Primary prevention of SCD is carried out with the aim of preventive measures in patients with identified predictors of SCD development [23].
Angiotensin-converting enzyme inhibitors (ACEIs)
The effectiveness of ACEIs has been studied in patients who have recently suffered a myocardial infarction (MI). Treatment with ACE inhibitors leads to a reduction in the incidence of progression of heart failure and mortality from it, as well as the risk of SCD. It should be noted that the degree of reduction in the incidence of SCD under the influence of ACEs ranges from 30 to 54%.
ACE inhibitors prevent SCD by affecting cardiac remodeling, electrolyte balance, and hemodynamic disturbances. The value of ACE inhibitors for reducing the risk of death and major cardiovascular complications in patients with chronic heart failure, asymptomatic left ventricular systolic dysfunction and in patients with acute myocardial infarction has been identified in many randomized clinical trials [26-30].
Aldosterone receptor blockers
Increased activity of the RAAS in congestive heart failure leads to increased levels of angiotensin 2 and aldosterone. It has been proven that the use of spironolactone in combination with diuretics, ACE inhibitors and digoxin was associated with a reduction in mortality and the incidence of SCD.
Thrombolytic and antithrombotic agents
It has been proven that thrombolytic therapy in the acute period of MI reduces the risk of death by 18 - 50%. The beneficial effect of thrombolysis is to some extent associated with a reduction in the incidence of SCD. The effect of thrombolytic therapy increases to 25% if, in the early period of a heart attack, patients are simultaneously prescribed aspirin orally. Long-term treatment with aspirin after MI causes a 25% reduction in overall mortality. Although this fact is supported by pooled data rather than the result of a single study, the widespread use of aspirin is also justified by its beneficial effect on the risk of non-fatal recurrent heart attack and stroke. Long-term anticoagulant therapy is inferior to antithrombotic agents in preventing death, but not cardiovascular complications.
Beta blockers
According to the Carvedilol Or Metoprolol European Trial (Comet), the absolute reduction in mortality over 5 years in the group of patients taking carvedilol was 5.7% greater compared to patients taking metoprolol. From the MERIT-HF study, it is clear that in the metoprolol CRXL group, cases of SCD were less common than in the placebo group, RR 0.59 (0.45-0.78). The Post hoc analysis from the MUSST study demonstrated that beta blockers were observed in patients with and without tachycardia, but the incidence of arrhythmogenic death or cardiac arrest was not significantly affected by beta blocker use. According to studies, in ischemic cardiomyopathy, up to half of the entire viable myocardium can remain in a state of hibernation. And it is beta blockers that solve the problem of “awakening” and actively involving areas of hibernating myocardium in the functioning, which was demonstrated in an experiment in which the use of beta blockers in combination with ACE inhibitors in patients with the presence of viable myocardium in areas of impaired contractility was accompanied by an increase in ejection fraction left ventricle, reducing the degree of dilatation of the left ventricle, the severity of decompensation and areas of asyrnergy. The MERIT HF study (Metoprolol CRXL Randomized Intervention Trial in Congresive Heart failure) aimed to resolve the issue of the effect of the lipophilic beta blocker metoprolol on overall mortality. The study included 3991 patients. The leading characteristics of the patients were: low ejection fraction, old age, previous myocardial infarction, moderate or moderate heart failure. This study showed that metoprolol reduced not only the incidence of sudden death, but also the incidence of death from progression of heart failure (the risk of death was reduced by 41% to 49%). The number of side effects in the metoprolol group was 13.9%, and in the placebo group - 15.3%. The clinical significance of this study was that it put an end to a 25-year-old debate: should beta blockers be used in the treatment of patients with heart failure? It has been established that the lipophilic beta1 blocker metoprolol is a new standard in the treatment of heart failure from the point of view of evidence-based medicine. When taken once daily, metoprolol significantly improved survival in patients with chronic heart failure and reduced ejection fraction: there was a 34% reduction in total mortality, a 38% reduction in cardiovascular mortality, a 41% reduction in sudden death and a reduction in deaths from circulatory failure - by 49% [31-33].
Amiodarone
This is an antiarrhythmic drug that has the properties of drugs of classes I, II, III, IV. Amiodarone is not thought to have an effect on survival in patients with heart failure and low left ventricular ejection fraction, but some studies have shown that amiodarone reduces the incidence of SCD and increases left ventricular ejection fraction. Despite its side effects, such as thyroid damage, pulmonary toxicity, hepatotoxicity, neuropathies (due to iodine ions), etc., amiodarone remains the most commonly used drug for tachyarrhythmias. Other antiarrhythmic drugs, such as sotalol, can be used to prevent ICD shock (implantable cardiodefibrillator shock) in cases where amiodarone is not effective, not tolerated, or its use is contraindicated due to side effects. According to the DIAMOND - CHF (Danish Investigations of Arrhythmia and Mortality on Dofetilide Congresive Heart Failure) study, there was no difference in SCD between patients randomized to dofetilide and those randomized to placebo. Clinical studies of dofetilide were limited due to drug-drug interactions and the presence of renal failure in patients. Despite significant suppression of ventricular ectopic activity, the class IC antiarrhythmic drugs flecainide and encainide increased overall and arrhythmogenic mortality in patients with ischemic cardiomyopathy. To evaluate the effect of amiodarone on overall mortality in patients with congestive heart failure (CHF) and asymptomatic ventricular arrhythmias, 674 patients (mean age 66 years, 99% men) with CHF, cardiomegaly, frequency ventricular extrasystoles 10 per hour or more and left ventricular ejection fraction 40%. In the amiodarone group, 131 (39%) patients died, in the placebo group - 143 (42.3%), overall survival at 2 years was 69.4% in the placebo group. The number of cases of SCD was 15–19%. At 6 months, the amiodarone group showed a greater increase in left ventricular ejection fraction than the placebo group (33.7% vs. 29.2%). The incidence of asymptomatic ventricular arrhythmias in patients in the group was lower than in the placebo group. In patients with chronic heart failure and asymptomatic ventricular arrhythmias, amiodarone suppresses arrhythmias and improves left ventricular function, but does not reduce the risk of sudden death or increase survival [31].
Calcium antagonists
This group of drugs slows the heart rate, reduces the risk of myocardial infarction, but does not affect overall mortality. At the same time, the use of drugs that cause increased heart rate in the same groups of patients is accompanied by an increase in overall mortality.
Secondary prevention
The main means of secondary prevention of SCD in patients who have previously suffered circulatory arrest due to ventricular tachycardia or VF, or who have bouts of sustained ventricular tachycardia, use implantable cardiac defibrillators (ICDs). With the development of the problem of treating cardiac arrhythmias using implantable devices, the question arose about the need to apply an electrical discharge with the device to eliminate life-threatening arrhythmic episodes, but the creation of an implantable device is associated with great technical difficulties. For about eleven years, such devices have been improved and research has been carried out on their implantation in dogs. At the Johns Hopkins Medical Center in Baltimore, with the participation of M. Mirowski, and M. Mower, doctors V. Gott, P. Reid, M. Weisfeldt, L. Watkins in February 1980 first implanted an ICD in a patient who suffered from paroxysms of ventricular tachycardia. In Russia, for the first time at the National Center for Agricultural Agricultural Sciences named after A.N. Bakulev of the Russian Academy of Medical Sciences, an operation was performed to implant an ICD, performed by academician L.A. Boqueria in 1990. The introduction of ICVD into clinical practice over the past decades has caused a revolution in the treatment of life-threatening arrhythmias. These studies demonstrated the superiority of this approach compared with standard treatment options in reducing the incidence of SCD and overall mortality. The results of three randomized trials that examined the effectiveness of ICD in the prevention of SCD in high-risk patients, approximately 80% suffered from coronary heart disease (half of the cases had a history of myocardial infarction), 10% had non-ischemic cardiomyopathy, and 5% had no signs of heart disease.
One study (AVID) found a significant 31% reduction in mortality with the use of defibrillators. Recently, the results of three studies were pooled into a single database (a total of 934 patients received an ICD and 934 patients received amiodarone). The most clear advantage of ICDs over amiodarone was the reduction in the relative risk of death over 6 years of follow-up. Clinical trial data also supported the use of ICP therapy in patients with chronic heart failure and low left ventricular ejection fraction [34-37].
Invasive electrophysiological study (EPS): role in the prognosis of SCD
EPI is an invasive study that allows you to record endocardial electrograms of various parts of the heart using special electrodes - catheters. The electrodes are inserted into the heart cavity using the Seldinger technique, most often through the left femoral vein.
During EPI, the initial cycle duration (DC), the recovery time of the sinus node function, the sinoatrial node conduction time, the intraatrial conduction time of excitation (P - A4), the intranodal conduction (A4 - H) are determined, the conduction time is assessed according to the intraventricular conduction system of His - Purkinje (H - V), effective refractory period of the right atrium, antegrade and retrograde effective period of the AV junction, functional refractory period of the AV junction, effective refractory period of the right ventricle.
Today, invasive EPS is a generally accepted and widely used method for diagnosing and identifying risk factors for SCD associated with life-threatening arrhythmias [30].
Conclusion
Diseases of the cardiovascular system occupy one of the leading places in the structure of morbidity among the population of Russia and determine the level of its mortality, temporary and permanent disability. At the same time, SCD accounts for about half of all deaths. In 50% of cases, deaths from such a common disease as coronary heart disease (CHD) are sudden, primarily arrhythmogenic.
Sudden cardiac death is a disease of the cardiovascular system, which is one of the causes of death in most economically developed countries of the world.
Sudden cardiac death is one of the pressing problems of our time. Currently, many different studies are being conducted to study this problem.
Based on randomized trials, programs have been created aimed at preventing sudden cardiac death for patients and doctors.
Nowadays, sudden cardiac death is being actively prevented by implantable cardiac defibrillators. The introduction into clinical practice over the past decades has caused a revolution in the treatment of life-threatening arrhythmias. These studies demonstrated the superiority of this approach compared with standard treatment options in reducing the incidence of sudden cardiac death and overall mortality. The problem remains unresolved; various activities are ongoing to understand and resolve this issue. When treating patients with cardiovascular diseases, the main efforts of doctors should be aimed at actively preventing sudden cardiac death with the help of drugs that have maximum effectiveness and safety.
Symptoms of sudden cardiac death (SCD)
- Sharp weakness
- Dizziness
- Loss of consciousness, possible appearance of tonic contractions of skeletal muscles, noisy breathing
After 2.5–3 minutes. breathing stops completely. It should be remembered that after about 3 minutes. from the moment of onset of ventricular fibrillation or asystole, irreversible changes occur in the cells of the cerebral cortex. It is precisely in connection with such sudden changes in SCD that it is necessary to establish a diagnosis in a timely manner and carry out a number of preventive measures (prescription of pharmacological drugs, endovascular treatment, interventional treatment in the scope of implantation of a cardioverter-defibrillator).
Manifestations and course of coronary death
Autopsies of patients who died suddenly usually reveal damage to the coronary arteries by atherosclerotic plaques. In this case, the lumen of the vessel narrows by 70% or more. Very often, on the damaged surface of the vessel there is a thrombus that has completely stopped blood flow in a fairly large area of the heart muscle. Usually, signs of myocardial infarction cannot be identified, since too little time has passed since the onset of the disease. Histological examination can reveal signs of incipient necrosis and cell restructuring.
Due to electrical instability of the myocardium, life-threatening arrhythmia occurs (asystole or ventricular fibrillation). Blood flow stops, including through the cerebral arteries. In this regard, the person quickly loses consciousness and falls. Noisy wheezing breathing and foam at the mouth may appear. After a few minutes, the muscles will begin to twitch involuntarily. The skin becomes pale, cyanosis of the lips and limbs is observed. The pulse and breathing stop completely, the pupils dilate and stop responding to light.
Diagnosis of SCD
- To confirm the diagnosis, additional diagnostic methods are needed:
- Taking an electrocardiogram (ECG)
- Carrying out stress tests (treadmill test or test on a bicycle ergometer, myocardial scintigraphy with stress)
- 24-hour ECG recording is performed (Holter ECG monitoring)
- According to indications, a contrast study of the arteries of the heart is required - multispiral computed coronary angiography on an outpatient basis or selective coronary angiography in a hospital setting.
- In some cases, it is necessary to conduct a genetic study to exclude hereditary channelopathies
- Sometimes it is necessary to resort to invasive electrophysiological testing for the purpose of provocative tests and pharmacological testing
Preventing an emergency: what needs to be done?
Considering the main causes of sudden cardiogenic death, prevention consists of measures aimed at early diagnosis and proper treatment of diseases of the heart, blood vessels, and associated pathological conditions. Also, special attention should be paid to preventing the occurrence of such pathologies:
- Atherosclerosis and dyslipidemia, maintaining proper nutrition, reducing the amount of fatty foods, and alcohol intake.
- Obesity, metabolic syndrome due to diabetes, reducing the consumption of sweets, simple carbohydrates, saturated fats.
- Cardiac pathology, reducing salt intake, quitting smoking.
Additionally recommended:
- Timely treatment of malignant arrhythmia, progressive angina.
- In the presence of cardiac pathology, regular examination with ECG, EchoCG, Holter monitoring.
- Hospitalization to the clinic for primary deterioration of the condition.
Algorithm for helping the victim
With VCS, the condition develops extremely rapidly. Resuscitation is required if a person has no consciousness, breathing or pulse, and dilated pupils do not respond to light. Determining signs of life and calling an ambulance must be done within 10-15 seconds, otherwise it will not be possible to save from cardiac arrest. The order of execution according to the standard cardiopulmonary resuscitation scheme according to the SAV algorithm:
- Restoration of blood circulation using indirect cardiac massage.
- Ensuring access to the airways and their patency.
- Restoring oxygen access using artificial respiration.
Early initiation and adherence to recommendations increases the risk of rescue after cardiac arrest. Algorithms of action are presented in more detail in the article “Rules for performing cardiopulmonary resuscitation.”
Medical resuscitation includes recording heart activity on a cardiogram, defibrillation if indicated, intubation and artificial ventilation with oxygen supply, catheterization, cardiac massage and coronary angiography under the control of the patient's condition.
Blood clot separation
“The rupture of a blood clot, or thromboembolism, is a serious complication of a large number of diseases,” notes the therapist. However, she says, there are certain risk factors that lead to such a problem. Among them:
- major surgical interventions;
- major trauma;
- long-term immobilization, i.e. a person being in a forced immobile state;
- oncopathology;
- Chemotherapy and radiation therapy, as well as treatment drugs, all cause blood to thicken and increase the risk of developing blood clots.
Compression can also have a negative impact when compression occurs by a hematoma or tumor. Those who have already had thromboembolism previously are at risk of developing such a pathology, and age is also a negative factor. Pregnancy, taking a number of contraceptives, and a number of infectious pathologies can also cause malfunctions in the blood coagulation system. To check the condition of the circulatory system, it is enough to take a coagulogram.
“If the patient suddenly experiences shortness of breath and a feeling of lack of air, you should consult a doctor as soon as possible. Also, sometimes the doctor may be alerted to something on the cardiogram. This is an acute emergency situation that requires immediate intervention,” the therapist advises. At the same time, the rupture of a blood clot often causes sudden death in people of working age.
Catch it if you can. How to detect and destroy a blood clot Read more
Central sleep apnea
Usually they talk about two types of sleep apnea (apnea). It can be obstructive, that is, caused by obstruction (blockage) of the upper respiratory tract. The second type is central sleep apnea, which is caused by a decrease in the formation of an impulse in the central nervous system that stimulates the respiratory muscles, notes Tatyana Shalygina, general practitioner, cardiologist . The specialist notes that some people may experience both mechanisms of respiratory arrest at the same time.
“The cause of this form of pathology is left ventricular heart failure. It occurs against the background of a disruption in the flow of impulses from the central nervous system to the respiratory muscles. In general, apnea is closely related to the cardiovascular system, the respiratory system and normal sleep, and therefore to the nervous system too,” notes the therapist.
People with this pathology complain of difficulty falling asleep, insufficient and intermittent sleep, and drowsiness during the day due to the fact that they were unable to rest at night. There are also those who wake up with a feeling of lack of air, shortness of breath, which are alleviated if the person takes the necessary semi-sitting position or adds several pillows under the head.
Also among the reasons for the development of central sleep apnea are:
- cerebrovascular accidents;
- renal failure;
- staying at high altitude.
“This condition is fraught with consequences such as myocardial ischemia, angina pectoris, arrhythmia, from which a person can also wake up at night. Often, such patients may experience convulsive contractions of the muscles of the lower extremities during sleep, which can cause poor sleep. As a result, a vicious circle is formed,” says Tatyana Shalygina.
To identify the problem and isolate it from the list of other similar ones, a person is recommended to undergo polysomnography. This is a simple and popular study now. Based on the results, therapy using CPAP machines is already prescribed. The problem cannot be ignored, as it can lead to death.
Killer snoring. Why are night trills dangerous? Read more