What is arrhythmia?
The heart works like a pump and ensures continuous blood circulation.
This is necessary to deliver blood enriched with oxygen and nutrients to every cell of the body. In the right atrium of the heart there is the sinus node (SU), the “commander-in-chief” of the heart rhythm. The sinus node generates electrical impulses, under the influence of which the right and left atria first contract, then the right and left ventricles. Other parts of the myocardium can also generate electrical impulses, but in a healthy heart they are suppressed by the sinus node and do not disturb the heart rhythm.
The correct heart rhythm is considered to be sinus rhythm, in which the heart rate (heart rate) is from 60 to 80 beats/min. An arrhythmia is any heart rhythm that differs from normal sinus rhythm.
Heart rate is determined in a state of physical and emotional rest, since this indicator may increase during sports or excitement. It should also be noted that the normal heart rate is a relative value and depends on the individual characteristics of a person. For example, a rapid heart rate can be observed during pregnancy, a slow heart rate in athletes.
Treatment of atrial fibrillation (atrial fibrillation)
There are several ways to treat atrial fibrillation (atrial fibrillation) and restore sinus rhythm. These are oral administration of antiarrhythmic drugs, intravenous administration of antiarrhythmic drugs, and cardioversion (electrical pulse therapy, EIT). If the doctor restores the rhythm in a clinic or at the patient’s home, they most often start with intravenous medications, then take pills. The procedure is carried out under ECG control, the doctor observes the patient for 1-2 hours. If restoration of sinus rhythm does not occur, the patient is hospitalized in a hospital. In the hospital, drugs can also be administered intravenously, but if time is limited (the duration of the attack is approaching the end of the second day) or the patient does not tolerate the paroxysm well (a decrease in blood pressure is observed, etc.), EIT is more often used.
Cardioversion is performed under intravenous anesthesia, so the electrical shock is painless for the patient. The success of rhythm restoration depends on many factors: the duration of the attack, the size of the heart cavities (in particular, the left atrium), sufficient saturation of the body with an antiarrhythmic drug), etc. The efficiency of EIT is close to 90-95%.
If paroxysm of atrial fibrillation lasts more than two days, restoring the rhythm is possible only after special preparation. The main steps are taking blood thinning medications under the control of a special analysis (INR) and conducting transesophageal echocardiography (TEE) before EIT to exclude blood clots in the cavities of the heart.
Types of arrhythmia
There are several options for classifying arrhythmias. Depending on the heart rate there are:
- tachycardia (heart rate exceeds 90 beats/min);
- bradycardia (heart rate less than 60 beats/min).
The main classification of arrhythmias is based on what physiological property of the myocardium is impaired - automaticity, excitability, conductivity.
- Violation of myocardial automatism.
Automaticity is the ability of the heart to contract rhythmically without external stimulation under the influence of impulses arising within itself.
Arrhythmias in which the automaticity of the heart is impaired and the sinus node acts as the driver of the heart rhythm are called “nomotopic.” For example, such arrhythmias include sinus tachycardia, sinus bradycardia, and sinus node syndrome. Often nomotopic arrhythmias are diagnosed in absolutely healthy people and are physiological.
Arrhythmias in which the automaticity of the heart is impaired and the pacemaker is located outside the sinus node are called “ectopic” or “heterotopic”. With ectopic arrhythmias, the center of automatism moves to the sections underlying the SG with the formation of abnormal rhythms. Ectopic arrhythmias include:
- atrioventricular rhythm - the pacemaker is the AV node (atrioventricular node);
- migration of the supraventricular pacemaker - gradual displacement of the pacemaker from the sinus node to the AV node;
- idioventricular rhythm - ventricular rhythm.
- Impaired cardiac excitability.
Cardiac excitability is the ability of the myocardium to be excited under the influence of external influences.
Arrhythmias in which the excitability of the heart is impaired include:
- extrasystoles - the appearance of extraordinary contractions of the entire heart or its individual chambers. Depending on the location of the extrasystoles, there are sinus, atrial, nodal, ventricular;
- paroxysmal tachycardia - heart rhythm disturbances, which are characterized by palpitations with a heart rate of 140-220 beats/min. The most common form of this type of arrhythmia is atrial. Less common are atrioventricular and ventricular paroxysmal tachycardias.
- Impaired cardiac conduction.
Conductivity is the ability of the heart to conduct electrical impulses from the point of their origin to the contractile part of the myocardium. If cardiac conduction is impaired, various blockades may occur:
- SA blockade is a violation of myocardial conduction between the sinus node and the atrium;
- interatrial blockade - slow passage of impulses between the atria;
- AV block - arrhythmias in which the transmission of impulses from the atria to the ventricles slows down;
- intraventricular blockade - disruption of the conduction of the His bundle.
Also, arrhythmias in which cardiac conduction is disrupted include Wolff-Parkinson-White syndrome, a congenital heart pathology characterized by the presence of additional conduction pathways, which leads to premature excitation of the ventricles.
- Mixed arrhythmias.
With mixed arrhythmias, several physiological properties of the heart are disrupted. For example, such arrhythmias include ectopic rhythms with exit block and atrioventricular dissociations. One of the most common mixed arrhythmias is atrial fibrillation, in which chaotic electrical activity of the atria is observed with a pulse frequency of 350-700 beats per minute.
Epidemiology of paroxysmal atrial fibrillation
Atrial fibrillation and flutter are the most common and dangerous types of heart rhythm disturbances and occur in 0.4–1.0% of cases in the population [1, 2].
The incidence of atrial fibrillation/flutter increases with age. According to the Framingham Study, the incidence of atrial fibrillation (AF) doubles every 10 years of life: 0.55% in patients aged 50–59 years and 8.8% in patients aged 81–90 years [3]. Over the past 20 years, there has been a trend towards an increase in the incidence of AF, especially among men. In addition, there has been an increase in the number of hospitalizations for MA; in the USA, for example, this parameter increased 2.5 times over the period from 1985 to 1999 [4, 5]. The negative impact of atrial fibrillation/flutter was also studied: the risk of thromboembolic complications increased by 4–5 times, the mortality rate by 1.5–2.0 times [6, 7]. This pathology can lead to the development and progression of heart failure and a decrease in quality of life. Among patients hospitalized for cardiac arrhythmias, AF occurs in 34%, atrial flutter – in 4% of cases.
As a rule, at the very beginning, MA is paroxysmal. The prevalence of AF paroxysms varies, according to various sources, in the range of 22–65%. Of these, in 35–78% of cases, the paroxysmal form of arrhythmia becomes persistent [8].
Definition, classification of paroxysms of flickering
The term “paroxysmal atrial fibrillation” refers to a rhythm disturbance associated with chaotic contraction of individual groups of atrial muscle fibers, lasting no more than 7 days with the possibility of spontaneous relief. The frequency of atrial waves can reach up to 600 beats/min. Due to the variability of atrioventricular conduction under these conditions, partly due to the hidden conduction of some impulses, the ventricles contract randomly. In the absence of additional disturbance of atrioventricular conduction, the ventricular rate is about 100–150 beats per minute (tachysystolic atrial fibrillation). It is believed that the electrophysiological basis of atrial fibrillation is multiple small circles of impulse circulation in the atrial myocardium. Attacks of atrial fibrillation, especially the normo- and bradysystolic forms, often do not cause pronounced hemodynamic disorders and may not be accompanied by a noticeable deterioration in the patient’s condition and well-being.
In terms of prescribing differentiated therapy, it is noteworthy to distinguish two forms of paroxysmal MA: with a predominance of the tone of the parasympathetic nervous system (“vagal” paroxysmal MA) and with a predominance of the tone of the sympathetic nervous system (“adrenergic”, “catecholamine” paroxysmal arrhythmia) [9].
Definition, classification of flutter paroxysms
Atrial flutter is a regular contraction of the atria at a rate of about 250–350 beats per minute. The ventricular rhythm may be regular or irregular. The frequency and regularity of the ventricular rhythm during atrial flutter is determined by atrioventricular conduction, which can change. Atrial flutter occurs 10–20 times less frequently than paroxysmal fibrillation. Sometimes atrial fibrillation and flutter alternate in one patient. The term “atrial fibrillation” was proposed by G.F. Lang to designate atrial fibrillation and flutter due to the commonality of some pathogenetic and clinical features, however, in the diagnosis, arrhythmia must be specifically designated as fibrillation or flutter.
With the paroxysmal form of flutter, the frequency of paroxysms can be very different: from once a year to several times a day. Paroxysms can be triggered by physical activity, emotional stress, hot weather, drinking too much, alcohol, and even intestinal upset. Paroxysms sometimes go away on their own, but sometimes drug treatment is required. Some people with MA do not feel it, while others notice a slight irregularity in their heart rhythm. You may also experience dizziness, pressure, and chest pain.
Atrial flutter, being one of the forms of AF, differs little in clinical manifestations from atrial fibrillation, but is characterized by somewhat greater persistence of paroxysms and greater resistance to antiarrhythmic drugs. There are regular (rhythmic) and irregular forms of this arrhythmia. The latter is clinically more similar to atrial fibrillation. In addition, there are two main types of atrial flutter: 1 – classic (typical); 2 – very fast (atypical) [10].
Pathogenesis of atrial fibrillation/flutter
It was found that AF is predominantly an atrial tachyarrhythmia, which begins and forms in the left atrium, where several microreentry circles occur. Atrial flutter, on the other hand, usually occurs in the right atrium - in its lower part. The macroreentry circle, which underlies atrial flutter, is located mainly in the area (bridge) of the right atrium connecting the mouth of the inferior vena cava and the tricuspid valve annulus. Naturally, in our time, methods of treating paroxysms of atrial fibrillation and atrial flutter - these two related, but still different atrial tachyarrhythmias - should be considered separately.
Diagnosis of atrial fibrillation/flutter
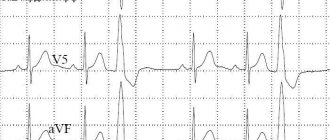
In AF, the electrocardiogram (ECG) shows no P wave, diastole is filled with small waves of irregular configuration and rhythm, more noticeable in lead VI. Their frequency is 300–600 beats per minute (usually not counted). Ventricular complexes follow an irregular rhythm and are usually not deformed. With a very fast ventricular rhythm (more than 150 beats/min), blockade of the leg, usually the right one, of the atrioventricular bundle is possible. Under the influence of treatment, as well as in the presence of atrioventricular conduction disturbances along with atrial fibrillation, the ventricular rate may be lower. At a frequency of less than 60 beats/min, we speak of the bradysystolic form of atrial fibrillation. Occasionally, atrial fibrillation is combined with complete atrioventricular block. At the same time, the ventricular rhythm is rare and regular. In persons with paroxysms of atrial fibrillation, when recording an ECG outside the paroxysm, especially soon after it, a more or less pronounced deformation of the P wave is often detected.
With atrial flutter, the ECG reveals regular atrial waves without diastolic pauses, having a characteristic sawtooth appearance, more clearly expressed in lead AVF. Atrial waves fill the ventricular diastole, they are also superimposed on the ventricular complexes, slightly deforming them. Ventricular complexes can follow rhythmically - after every second (then the ventricular rhythm is about 120-160 beats / min), third, etc. atrial wave, or arrhythmically, if the ratio of atrial and ventricular contractions is not constant. With a frequent ventricular rhythm, a violation of intraventricular conduction is possible, more often - blockade of the right leg of the atrioventricular bundle. With a frequent and regular ventricular rhythm, flutter is difficult to distinguish by ECG from other supraventricular tachycardias. If it is possible to temporarily reduce atrioventricular conduction (using carotid sinus massage, digoxin or 5 mg verapamil), the ECG picture becomes more characteristic.
Treatment of atrial fibrillation
When treating patients with atrial fibrillation and flutter at the prehospital stage, the feasibility of restoring sinus rhythm should be assessed. The absolute indication for restoration of sinus rhythm during the development of paroxysmal AF is the development of pulmonary edema or arrhythmogenic shock. In this case, emergency cardioversion should be performed prehospital.
Contraindications to restoring sinus rhythm at the prehospital stage include:
- the duration of paroxysm of atrial fibrillation is more than two days;
- proven dilatation of the left atrium (antero-posterior size 4.5 cm, according to echocardiography);
- presence of blood clots in the atria or a history of thromboembolic complications;
- development of paroxysm against the background of acute coronary syndrome (in the presence of stable hemodynamics);
- development of paroxysm against the background of pronounced electrolyte disturbances;
- decompensation of thyrotoxicosis;
- severe chronic hemodynamic disorders and some others.
In such cases, treatment should be aimed at stabilizing hemodynamics, preventing thromboembolism and controlling the heart rate in order to maintain it within 60–90 beats/min.
The drug of choice for heart rate control is cardiac glycosides, particularly digoxin. Further tactics are determined in the hospital. Persistent normosystolic form of AF without signs of heart failure does not require antiarrhythmic therapy at all [11].
It is known that 50–60% of recently developed (less than 48 hours) paroxysms of AF cease spontaneously. S. Ogawa et al. [12] in the J-RHYTHM study found that parameters such as mortality and the number of complications when stopping paroxysms of atrial fibrillation do not depend on the chosen treatment tactics (lowering the heart rate or restoring sinus rhythm). Similar results were obtained in their study by SH Hohnloser et al. [13].
Starting to characterize the methods of drug treatment of paroxysms of AF, we consider it necessary to emphasize that an antiarrhythmic drug has not yet been synthesized that can eliminate paroxysms of atrial fibrillation in every patient. The doctor must have a set of various effective drugs in order to be able to adequately replace one drug with another. Typically, treatment of AF paroxysm begins with an intravenous infusion of potassium chloride solution, often together with digoxin. Potassium chloride itself often eliminates paroxysms of AF after 3–5 infusions. In addition, an increase in plasma potassium concentration by 0.5–1.5 µm/l creates a favorable background for the subsequent action of other antiarrhythmic drugs.
In case of failure with the use of cardiac glycoside and potassium chloride or in the presence of contraindications to the use of cardiac glycosides, procainamide is administered. If necessary, this can be done earlier, for example, after 1-2 infusions of potassium chloride solution. According to the observations of various authors, the results of treatment of AF with procainamide are noticeably improved if it is administered to patients 20–30 minutes after intravenous infusion of a solution of potassium chloride and cardiac glycoside. In this way, sinus rhythm was restored in 65% of patients who did not respond at the prehospital stage to a sufficiently large dose of procainamide (up to 15 ml of a 10% solution) administered intravenously [14].
Effective antiarrhythmic drugs that are recommended for clinical use for the purpose of conversion of atrial AF are the IC class drugs propafenone and flecainide. They are effective when administered intravenously and orally. Sinus rhythm in patients with AF is restored 2–6 hours after oral administration. According to a placebo-controlled study by Yu.A. Bunina et al. [15], the effectiveness of propafenone in AF (single oral dose of 600 mg, observation for 8 hours) is about 80%. However, several randomized controlled studies emphasize the limited ability of intravenously administered propafenone to convert atrial flutter (no more than 40%). Our observations also indicate a rather low effectiveness of propafenone in the oral treatment of atrial flutter.
The use of class IC antiarrhythmics is contraindicated in patients with acute myocardial ischemia (unstable angina, myocardial infarction). A meta-analysis showed that antiarrhythmics of classes IC, IA and III have approximately the same effectiveness in stopping AF. However, no evidence was found of any effect of these drugs on the survival and quality of life of patients [16].
If a paroxysm of AF is preceded by an increase in sinus rhythm, if the paroxysm occurs in the daytime under the influence of stressors, physical or emotional stress, it must be assumed that the basis of such paroxysm is a hypersympathicotonic mechanism. Verapamil, diltiazem and β-blockers are first-line drugs for emergency intravenous reduction of heart rate, because these antiarrhythmics are highly effective and quickly (within 5-10 minutes) exert their effect. With intravenous digoxin, a sustained slowdown in ventricular rate is achieved much later (after 2–4 hours). For patients with a high risk of systemic embolism (atrial fibrillation/flutter lasting more than 2 days), in order to reduce the heart rate, amiodarone is a reserve drug, after the use of which it is possible to restore sinus rhythm and, consequently, the appearance of “normalizing” thromboembolism [17].
A number of international recommendations [18, 19] note that the relief of paroxysmal fibrillation/flutter in patients with heart failure or a left ventricular ejection fraction of less than 40% should be carried out with amiodarone. Other antiarrhythmics should be used with caution or not be used due to the relatively high risk of developing arrhythmogenic effects and negative effects on hemodynamics. A meta-analysis of the results of placebo-controlled studies of cardioversion of AF with amiodarone showed late relief of arrhythmia paroxysms: a significant difference in effectiveness between amiodarone and placebo was noted no earlier than 6 hours after their intravenous use. Taking this into account, after an intravenous “loading” dose of amiodarone is administered, it is then advisable to continue its intravenous infusion for 6–2 hours.
In a study by R.D. Kurbanova et al. [20] found that a course of treatment with a saturating dose of amiodarone helps restore sinus rhythm in 30% of patients with dilated cardiomyopathy complicated by AF. At the same time, long-term treatment with amiodarone helps maintain sinus rhythm in the next 6 months and compensates for heart failure. A meta-analysis also showed that treatment with amiodarone facilitates the procedure for restoring sinus rhythm and has a positive effect on patient survival [21].
In the study by S.A. Filenko [22] found that in patients with coronary heart disease, the paroxysmal form of AF occurs in the sympathetic and mixed types. In a study of drugs that have an anti-relapse effect on paroxysmal fibrillation, it was shown that amiodarone is the most effective, and in patients with paroxysmal AF of the sympathetic type, metoprolol also turned out to be effective.
S.A. Starichkov et al. [23] studied patients with arterial hypertension (AH) suffering from AF. Analysis of the results showed that the use of a combination of amiodarone and metoprolol for hypertension makes it possible to reduce the doses of antiarrhythmic drugs used and contributes not only to more effective control of blood pressure levels, but also to the prevention of AF paroxysms in 71% of patients. The use of β-blockers, both as monotherapy and in combination with amiodarone, leads to normalization of heart rate variability and has a positive effect on the processes of myocardial remodeling in various chambers of the heart.
It is known that blockade of type 1 angiotensin II receptors, in addition to lowering blood pressure, can lead to a decrease in myocardial remodeling and hypertrophy, normalization of electrolyte balance, and has indirect anti-ischemic and anti-adrenergic effects [24]. In the study by Yu.G. Schwartz et al. [25] treatment with losartan in patients with a combination of paroxysms of AF and hypertension was accompanied by a significant decrease in the frequency of arrhythmia paroxysms, in contrast to patients treated with nifedipine and atenolol. The authors believe that the likely mechanism for the positive effect of losartan on the course of AF paroxysms is a direct effect on the myocardium. Even J. Mayet [26] suggested that regression of left ventricular hypertrophy is associated with the antiarrhythmic effect of antihypertensive therapy.
One promising avenue for the treatment of arrhythmias is the use of omega-3-polyunsaturated fatty acids (ω-3-PUFA). In 2005, a study was published showing that consumption of fatty fish rich in long-chain ω-3-PUFA may reduce the risk of AF [27]. The authors explained this antiarrhythmic effect of ω-3-PUFA by reducing blood pressure and improving left ventricular diastolic function.
I.V. Antonchenko et al. [28] found that one of the possible mechanisms of the protective effect of ω-3-PUFA in patients with paroxysmal AF is reverse electrical remodeling of the atrial myocardium. The addition of ω-3-PUFAs to relief therapy reduces the number of episodes of AF and the time of their relief. However, the electrophysiological effects of using ω-3-PUFA at a dose of 1 g/day occur no earlier than the 20th day of administration.
The treatment tactics for paroxysms of atrial flutter largely depend on the severity of hemodynamic disorders and the patient’s well-being. This arrhythmia often does not cause severe hemodynamic disturbances and is little felt by the patient even with significant ventricular tachysystole. In addition, such paroxysms are usually difficult to stop with intravenous administration of antiarrhythmics, which can even cause a deterioration in the patient’s condition. Therefore, in these cases, emergency treatment is usually not required.
Speaking about drug treatment of this arrhythmia, it should be borne in mind that, according to the authors of the “Sicilian Gambit” concept [29], paroxysms of type I atrial flutter are better controlled by class IA drugs (quinidine, procainamide, disopyramide). However, when using drugs of this class there is a risk of paradoxical acceleration of the ventricular rate, so it is better to first use verapamil or beta-blockers. Paroxysms of type II atrial flutter are better controlled by class I3 drugs, in particular amiodarone. Domestic authors note the high effectiveness of nibentan in relieving paroxysms of fibrillation and especially atrial flutter [30].
It has now been proven that mental disorders worsen the course of arrhythmias, in particular AF, by complicating clinical manifestations and reducing quality of life. There is also an opinion that patients with depressive disorders have a violation of the autonomic regulation of heart rhythm (decreased parasympathetic and increased sympathetic tone), which increases the risk of AF.
In the study by B.A. Tatarsky et al. [31] the addition of Afobazole was accompanied by a pronounced anxiolytic effect without severe sedation, effective correction of autonomic disorders, and the absence of drug dependence and withdrawal syndrome. It was found that Afobazole treatment of patients with paroxysmal AF without pronounced structural changes in the heart was accompanied by a decrease in the frequency of paroxysms, the duration of arrhythmia episodes, and easier tolerability; there was a tendency to transform into an asymptomatic form.
The effectiveness of nibentan in relieving paroxysmal atrial fibrillation and atrial flutter is more than 80% [32]. Nibentan and ibutilide should be used only in specialized departments under ECG control (contraindicated in patients with heart failure, prolonged QT interval and sick sinus syndrome).
In patients with Wolff–Parkinson–White syndrome, the frequency of ventricular contractions during fibrillation/flutter, as a rule, is higher than in patients without ventricular preexcitation syndrome, and reaches 220–250 beats per minute or more, and tachycardia with abnormal rhythm and wide QRS complexes. The use of verapamil, diltiazem, and cardiac glycosides is contraindicated in Wolff–Parkinson–White syndrome, because, by reducing the refractoriness of the Kent bundle, they can increase the heart rate and even cause ventricular fibrillation. Atrial fibrillation/flutter is treated with drugs that impair conduction along the accessory atrioventricular conduction pathway. International recommendations for the treatment of patients with AF [19] suggest primarily using intravenous procainamide or ibutilide for this purpose.
Conclusion
In conclusion, it must be emphasized that the goal of antiarrhythmic therapy, like any other, is not only to eliminate and prevent paroxysmal arrhythmias, but also to improve the life prognosis, as well as reduce the mortality of patients, and for this it is very important to prevent the negative hemodynamic and proarrhythmic effects of the drugs used . The development of “antiarrhythmic drugs of the future” to provide sinus rhythm control must be based on a combination of efficacy and safety of therapy. Drugs with improved electrical, structural, and triggering properties are likely to reduce mortality and complications in patients with atrial fibrillation/flutter in the future.
Information about the authors: Volkov Viktor Evgenievich – candidate of medical sciences, researcher at the Federal State Institution RKNPK. Email; Yulia Vladimirovna Dotsenko – Candidate of Medical Sciences, researcher at the Federal State Institution RKNPK. Kiryushina Irina Evgenievna – doctor geneticist of the Federal State Institution RKNPK
Causes of heart rhythm disturbances
As a rule, arrhythmia is not the main pathology, but a consequence of other diseases. Causes of heart rhythm disturbances may include:
- sleep apnea syndrome is a disorder of the respiratory system, which is accompanied by temporary cessation of breathing at night, followed by the release of adrenaline and an increase in heart rate;
- arterial hypertension - syndrome of high blood pressure;
- coronary heart disease - a discrepancy between the myocardial need for oxygen and its delivery;
- heart failure - weakening of the pumping function of the heart;
- congenital and acquired heart defects.
- cardiomyopathies - pathologies of the myocardium associated with its mechanical or electrical dysfunction;
- myocarditis - inflammation of the heart muscle;
- myocardial surgery;
- previous heart attack;
- hyperthyroidism - hyperfunction of the thyroid gland;
- lung diseases;
- diabetes;
- infections.
There are arrhythmias that are based on genetic pathologies. For example, the arrhythmia can be caused by congenital long QT syndrome, which leads to ventricular tachycardia.
Risk factors for arrhythmia include:
- physical inactivity or, conversely, excessive physical activity;
- obesity;
- smoking, alcohol abuse;
- chronic lack of sleep;
- hormonal changes in the body. For example, in women, arrhythmia is often diagnosed after the onset of menopause;
- uncontrolled use of drugs that have an arrhythmogenic effect.
The main reasons for the development of MA are:
1. diseases of the cardiovascular system:
- hypertonic disease
- heart defects
- previous heart attacks
- previous myocarditis (inflammatory heart disease)
- toxic (alcoholic) cardiomyopathy
2. diseases of the bronchopulmonary system:
- bronchial asthma
- chronic obstructive pulmonary disease
- pneumonia
3. diseases of the gastrointestinal tract:
- peptic ulcer
- erosive gastroduodenitis
- HP infection (Helicobacter pylori gastroduodenitis)
- cholelithiasis
- chronic pancreatitis
- inflammatory bowel diseases
4.endocrine disorders:
- thyroid disease (thyrotoxicosis)
- diabetes
5. infections (ARVI, influenza, sepsis)
6. bad habits:
- alcohol abuse
- drug use
- heavy smoking
7.violation of the work and rest regime (work without days off and holidays, frequent business trips)
8.exacerbation of any concomitant pathology
9.oncological diseases, especially after courses of radiation and chemotherapy
10. combination of factors
AF can be detected when recording an electrocardiogram, when measuring blood pressure (the “arrhythmia” icon flashes on the tonometer screen), or the patient himself feels an unusual heartbeat.
If AF is detected, the patient should immediately contact an arrhythmologist or cardiologist. He will be offered an outpatient examination or, if necessary, hospitalization.
The optimal time to seek medical help is within 48 hours from the moment of the development of MA, since in this case it is possible to restore the rhythm as quickly, effectively and safely as possible.
In the latter case, artificial restoration of sinus rhythm with the help of drugs is called drug cardioversion. In the case when the heart rhythm is restored using an electric current (defibrillator), we talk about electrical cardioversion
One way or another, any form of this disease needs treatment. The global cardiological community has long developed a strategy for the management of such patients and identified the main goals of treating patients with atrial fibrillation.
How does arrhythmia manifest?
Arrhythmia may be accompanied by the following symptoms:
- a feeling of interruptions in the work of the heart;
- a feeling of somersault, a jolt in the heart;
- accelerated heartbeat;
- suffocation;
- dizziness;
- general weakness, fatigue;
- exercise intolerance.
The most severe manifestations of arrhythmia are presyncope and loss of consciousness, which are most often associated with a very high heart rate (more than 200 beats/min).
In addition, there are “silent” arrhythmias that are asymptomatic. They are usually diagnosed by electrocardiography.
How is arrhythmia diagnosed?
The main and simplest method for diagnosing arrhythmia is 12-lead ECG
In addition, to detect heart rhythm disturbances, the following are used:
- electrocardiography with physical activity (for example, on a treadmill);
- daily ECG monitoring - continuous recording of an electrocardiogram for a day or more;
- echocardiography is an ultrasound research method aimed at identifying morphological and functional changes in the heart;
- transesophageal electrical stimulation (TEES). During the examination, a special electrode is inserted into the lumen of the esophagus and placed in close proximity to the atria. Next, electrical stimulation of the heart is performed in a certain mode, which leads to physiological tachycardia. In this way, it is possible to quickly and accurately detect the source of the arrhythmia.
How is cardiac arrhythmia treated?
There are several methods for treating arrhythmia:
- drug therapy. The patient can be prescribed both drugs that have antiarrhythmic properties and drugs that do not directly affect the electrophysiological properties of the myocardium. The latter are called upstream therapy. It includes ACE inhibitors, angiotensin II receptor antagonists, statins, corticosteroids, polyunsaturated fatty acids and other drugs. Upstream therapy is aimed at eliminating the causes that lead to arrhythmia: inflammatory processes, high blood pressure, myocardial remodeling;
- implantation of a pacemaker - a medical device that affects the heart rhythm. Most often, a pacemaker is used for slow heart rate and AV block;
- radiofrequency ablation of the heart (RFA) is a surgical intervention during which an electrode is used to destroy the focus of pathological excitation of the myocardium or areas of abnormal impulse conduction.
Attacks of atrial fibrillation - how to prevent?
To prevent paroxysms of atrial fibrillation from reoccurring, the patient must constantly take an antiarrhythmic drug. For the purpose of prevention. Today there are many antiarrhythmics; the choice of drug must be made by the doctor. A patient with atrial fibrillation requires observation by a cardiologist, during which regular examination is carried out (for example, echocardiography once a year, or 24-hour Holter monitoring, if necessary, to assess the effectiveness of treatment), and treatment correction. The selection of drug therapy is always, for any disease, a very painstaking task that requires literacy and perseverance on the part of the doctor and understanding and diligence on the part of the patient. Not only the effectiveness, but also the tolerability of treatment can vary from person to person.
The ineffectiveness of drug therapy for atrial fibrillation may be an indication for surgical treatment. In the left atrium (near the confluence of the pulmonary veins) there are zones in which electrical impulses are generated that can trigger atrial fibrillation. Increased electrical activity in these areas can be detected using a special electrophysiological examination (EPI). A special catheter is inserted into the heart cavity, the information obtained allows you to create an electrical “map” and determine trigger (“trigger”) areas. The examination is carried out under local anesthesia and is quite safe for the patient. After identifying the “trigger” areas, an operation is performed - radiofrequency ablation of trigger zones (RFA). The catheter uses high-frequency current to destroy these areas and disrupt the initiation of the arrhythmia. In four out of five cases, atrial fibrillation does not return.
Possible complications and prognosis
First of all, the prognosis of the disease depends on the type of arrhythmia. If the rhythm disturbance is not associated with organic damage to the heart, then it may not cause any particular harm to health. For example, such arrhythmias include supraventricular extrasystoles.
However, there are also very dangerous types of arrhythmias. One of them is atrial fibrillation, which can cause myocardial infarction and heart failure.