1.What is heart failure?
Heart is a serious and, unfortunately, very common disease. This disease is one of the main reasons for hospitalization in people over 65 years of age.
Heart failure does not mean the heart stops working. Rather, it means that the heart becomes weaker than usual and pumps blood less well. In heart failure, blood moves through the heart and body at a slower rate. As a result, the heart cannot pump enough oxygen and nutrients
to meet the body's needs.
The heart responds to this by stretching the chambers
so more blood can pass through them, and this helps for a while.
But over time, the walls of the heart muscle weaken, unable to work at such a strenuous rhythm. This affects the kidneys, which cause the body to accumulate more fluid and salt. Fluid can accumulate in the arms, legs (ankles and feet), lungs and other organs, leading to edema. This condition is also called congestive heart failure .
A must read! Help with treatment and hospitalization!
Symptoms of chronic heart failure
Main symptoms:
- shortness of breath at rest and on exertion,
- swelling of the legs, legs, feet, anterior abdominal wall.
- enlarged liver and pain in the right hypochondrium.
- decreased exercise tolerance.
Classes of CHF
According to the New York Heart Association methodology, there are 4 classes of CHF.
Class 1 – there are heart diseases, but they do not limit daily activity.
Class 2 – heart disease leads to a slight limitation of physical activity. There are no symptoms at rest; normal physical activity causes fatigue and shortness of breath.
Class 3 – significant limitation of physical activity.
Class 4 – restriction of any physical activity; symptoms appear at rest.
The class of heart failure can be determined using the SHOKS questionnaire (scale for assessing the clinical condition of the patient) as modified by Mareev V.Yu. A particular class of CHF is assigned depending on the number of points that are assigned based on the results of answers to questionnaire questions.
2.What causes the disease?
Heart failure can be caused by many factors and pathological processes occurring in the heart, including:
- Cardiac ischemia
. Coronary heart disease (CHD) is a disease of the arteries that supply blood and oxygen to the heart, in which blood flow to the heart muscle is reduced. As a result, the heart lacks oxygen and nutrients. - Heart attack
. A heart attack can occur when a coronary artery suddenly blocks and stops the flow of blood to the heart muscle. All or part of the heart muscle is no longer supplied with oxygen and may become damaged. A heart attack can cause an area in the heart that then does not function properly. - Cardiomyopathy
, or damage to the heart muscle. The causes of cardiomyopathy can range from problems with the arteries or circulation, infections, or alcohol or drug abuse. - Common factors leading to fatigue
. This may include high blood pressure, heart valve disease, thyroid disease, kidney disease, diabetes, or congenital heart defects. All this can lead to heart failure. In addition, heart failure can result from a combination of several of these conditions.
Visit our Cardiology page
Causes of chronic heart failure
Chronic heart failure is the final outcome of any heart disease.
A short list of nosologies that can lead to the development of CHF:
- hypertonic disease;
- coronary heart disease: previous myocardial infarction;
- cardiomyopathies (hereditary and acquired);
- myocarditis of various etiologies;
- acquired heart defects;
- pericardial disease (constrictive pericarditis);
- tachyarrhythmias (fibrillation, atrial flutter).
3.What are the types and stages of heart failure?
What are the types of heart failure?
Systolytic dysfunction
, or
systolic heart failure , occurs when the heart muscle does not contract strongly enough to allow normal flow of oxygenated blood throughout the body.
Diastolic dysfunction , or diastolic heart failure, occurs when the heart beats normally, but the ventricle—the main chamber responsible for pumping blood—does not relax, reducing the amount of blood that can enter the heart and increasing blood pressure in the lungs.
Stages of heart failure
In 2001, the American Heart Association and the American College of Cardiology developed stages of heart failure. For each stage, characteristic signs were identified and treatment recommendations were developed. Doctors also noted that heart failure can progress, and the process can move from one stage to another.
The stages of heart failure according to this classification are as follows:
Stage A.
This includes people at high risk of developing heart failure, including those with high blood pressure, diabetes, coronary heart disease, alcohol abuse, or a family history of heart failure. In addition to drug therapy, regular exercise, quitting smoking and alcohol, and therapy aimed at treating high blood pressure and lipid metabolism disorders are recommended for this group.
Stage B.
This includes patients diagnosed with left ventricular systolic dysfunction, but only those without symptoms of heart failure. The diagnosis in this case was usually made based on the results of an ejection fraction less than 40% and echocardiogram results. Treatment methods for this group of patients are similar to the previous ones, however, in some cases it may be necessary to surgically treat the coronary artery and heart valves.
Stage C.
This group includes patients with systolic heart failure who exhibit symptoms of the disease. The most characteristic symptoms of heart failure are shortness of breath, rapid fatigue, and decreased physical activity. Additional treatment at this stage may include taking diuretics, a salt-free diet, limiting fluid intake, and in especially severe cases, surgical treatment using pacemakers and implantable cardiac defibrillators.
Stage D
This is the most serious stage, when patients continue to have systolic heart failure and characteristic symptoms even after complex treatment. In addition to the therapy used in the previous stages, the patient may need a heart transplant, surgical treatment, and special drug therapy, including those associated with the continuous administration of intravenous narcotic drugs.
About our clinic Chistye Prudy metro station Medintercom page!
Chronic heart failure (CHF) is a disease in which the heart is unable to pump enough blood to supply the body with oxygen. It can occur as a result of many diseases of the cardiovascular system, among which the most common are coronary heart disease, hypertension, rheumatoid heart defects, and endocarditis. A weakened heart muscle is unable to pump blood, releasing less and less of it into the vessels.
Heart failure develops slowly and in the initial stages appears only during physical activity. Characteristic symptoms at rest indicate a severe stage of the disease. As CHF progresses, it significantly worsens the patient’s condition, leading to decreased performance and disability. The result can be chronic liver and kidney failure, blood clots, and strokes.
Timely diagnosis and treatment can slow down the development of the disease and prevent dangerous complications. An important role in stabilizing the condition is given to a correct lifestyle: weight loss, low-salt diet, limiting physical and emotional stress.
Synonyms Russian
Congestive heart failure, heart failure.
English synonyms
Heart failure, congestive heart failure.
Symptoms
Clinical manifestations of heart failure depend on its duration and severity and are quite varied. The development of the disease is slow and takes several years. If left untreated, the patient's condition may worsen.
The main symptoms of chronic heart failure include:
- shortness of breath during physical exertion, when moving to a horizontal position, and then at rest;
- dizziness, fatigue and weakness;
- lack of appetite and nausea;
- swelling of the legs;
- accumulation of fluid in the abdominal cavity (ascites);
- weight gain due to edema;
- fast or irregular heartbeat;
- dry cough with pinkish sputum;
- decreased attention and intelligence.
General information about the disease
By contracting, the heart ensures continuous circulation of blood through the vessels. Together with the blood, oxygen and nutrients are supplied to all organs and tissues, and the end products of metabolism, including fluid, are removed. This is achieved by alternating two phases: contraction of the heart muscle (called systole) and its relaxation (diastole). Depending on which phase of cardiac activity disrupts its functioning, we speak of systolic or diastolic heart failure.
- Systolic heart failure is a consequence of weakness of the heart muscle and is characterized by insufficient ejection of blood from the chambers of the heart. Its most common causes are coronary heart disease and dilated myocardiopathy. More often observed in men.
- Diastolic heart failure occurs when the heart muscle loses its ability to stretch. As a result, much less blood enters the atria. The most common causes: arterial hypertension, hypertrophic myocardiopathy and stenotic pericarditis.
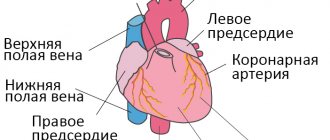
The human heart can be roughly divided into right and left halves. Pumping blood into the lungs and saturating it with oxygen is ensured by the work of the right parts of the heart, and the left ones are responsible for delivering blood to the tissues. Depending on which departments fail to cope with their task, they speak of right ventricular or left ventricular heart failure. When the functioning of the left sections is impaired, shortness of breath and cough come to the fore. Right-sided failure manifests itself as systemic edema.
To select the necessary medications, it is very important to determine the mechanism of heart failure and its type.
Who is at risk?
The presence of at least one of the following risk factors is sufficient for the development of chronic heart failure. The combination of two or more factors significantly increases the likelihood of disease.
Patients at risk include:
- high blood pressure;
- coronary heart disease;
- myocardial infarction in the past;
- heart rhythm disturbances;
- diabetes mellitus;
- congenital heart defect;
- frequent viral diseases throughout life;
- chronic renal failure;
- alcohol addiction.
Diagnostics
The diagnosis of chronic heart failure is made based on the medical history, characteristic symptoms and results of laboratory and other tests.
Laboratory research
- There are most often no changes in the general blood test. In some cases, moderate anemia may be detected.
- The erythrocyte sedimentation rate (ESR) may be elevated, especially when heart failure is the result of rheumatic heart disease or infective endocarditis.
- A general urinalysis is important to diagnose renal complications and exclude the renal origin of edema. One of the possible manifestations of chronic heart failure is high levels of protein in the urine.
- Total protein and protein fractions in the blood may be reduced due to their redistribution into the edematous fluid.
- Blood glucose. Important for excluding diabetes mellitus as a risk factor for heart failure.
- Cholesterol, high and low density lipoproteins. There is a clear relationship between elevated cholesterol levels and the development of atherosclerosis, coronary heart disease, and hypertension. High levels of cholesterol and lipoproteins in heart failure may indicate a more severe course of the disease.
- Sodium and potassium in the blood. In chronic heart failure, their level in the blood serum can change significantly due to edema. Monitoring blood composition is especially important when prescribing diuretics.
- Brain natriuretic propeptide (NT-proBNP) is a protein produced in the heart muscle in response to excessive stretching and overload. It circulates in the blood for quite a long time and can be easily determined during laboratory testing. The stronger the cardiac overload, the more active its secretion, therefore, an increase in the level of brain natriuretic propeptide in the blood reflects the severity of heart failure and helps to predict the disease. In addition, the higher the NT-proBNP level, the more severe the cardiac dysfunction. That is why this analysis is considered the “gold standard” in the diagnosis of chronic heart failure.
Additional Research
The scope of additional examination is determined by the attending physician.
- Chest X-ray. X-ray images allow you to assess the position and size of the heart, exclude or confirm concomitant changes in the lungs.
- Electrocardiography (ECG). Shows heart rhythm disturbances, as well as the consequences of a myocardial infarction.
- An echocardiogram allows you to differentiate systolic and diastolic heart failure, see the work of all parts of the heart, evaluate its size, muscle thickness, and examine the valves. The most important parameter is the ejection fraction. It reflects the efficiency of the heart and is expressed as the percentage of blood volume entering the aorta during contraction and remaining in it. Normally, this figure corresponds to 60-70%; in case of heart failure, it can decrease to 40%. The lower the ejection fraction, the more severe the degree of cardiac dysfunction. An indicator below 35% indicates a high risk of rhythm disturbances.
- Load tests. Designed to study the heart's response to increased physical activity.
- Coronary angiography. An X-ray examination in which a special contrast agent is injected through a catheter directly into the vessels of the heart. Helps establish the diagnosis of coronary artery disease.
Treatment
Heart failure is a chronic disease in which patients require constant medication. Properly selected therapy can slow down the progression of the process, and most often improve the condition. In some cases, surgical treatment is required.
An effective treatment method is the placement of pacemakers, or artificial heart rate regulators.
In the treatment of chronic heart failure, lifestyle also matters:
- complete cessation of alcohol and smoking,
- weight control,
- following a salt-free diet rich in protein and vitamins
- walks in the open air.
Prevention
- Lifestyle that prevents coronary heart disease:
- blood pressure control,
- regular physical activity,
- hardening procedures,
- normalization of metabolism (loss of excess weight, control of cholesterol levels, limited salt intake),
- quitting smoking, alcohol, coffee.
Clear and consistent implementation of the cardiologist’s recommendations can significantly slow down the pathological process and improve the patient’s quality of life.
Recommended tests
- Erythrocyte sedimentation rate (ESR)
- General blood analysis
- General urine analysis with microscopy
- Total protein in urine
- Serum albumin
- Total protein in whey
- Protein fractions in whey
- Total bilirubin
- Serum creatinine
- Urea in serum
- Rheumatoid factor
- C-reactive protein, quantitative (highly sensitive method)
- Potassium, sodium, chlorine in serum
- Serum calcium
- Serum magnesium
- NT-proBNP (quantitative)
4.Diagnosis of the disease
A special test called ejection fraction (EF) . It helps determine how well the heart pumps blood with each beat and can be used to diagnose both systolic and diastolic dysfunction. Ejection fraction as a percentage measures the amount of blood pumped with each beat.
In patients with systolic heart failure, the ejection fraction is less than 40%. Other diagnostic tests such as an echocardiogram or cardiac ultrasound can show how the heart is dilating and not pumping out enough blood with each beat.
Patients with diastylic heart failure have a normal ejection fraction test and their heart is pumping well, but an echocardiogram will show that the heart is not filling sufficiently during the relaxation phase that occurs between beats.
For timely diagnosis of heart failure, it is recommended to consult a cardiologist and periodically undergo a comprehensive cardiac examination.
Methods for diagnosing chronic heart failure
The central place in the diagnosis of CHF is occupied by instrumental diagnostic methods: chest radiography, ECG and echocardiography.
Laboratory diagnostics for CHF, in addition to the standard examination (general blood count, blood biochemistry - lipid profile assessment), may include an indicator such as brain natriuretic peptide, or BNP (brain natriuretic peptide) - a peptide hormone that is produced by heart cells in response for excessive stretching. This analysis is prescribed only by a doctor if necessary and has interpretation features.
If necessary, to clarify the nature of CHF, an MRI of the heart with contrast can be performed - to exclude myocarditis - or coronary angiography (if coronary artery disease is suspected).
X-ray of the chest organs
X-ray of the chest organs shows the presence of congestion in the pulmonary circulation, fluid in the pleural cavities, which indicates the presence of heart failure (this is what causes shortness of breath in CHF).
More information about the diagnostic method
ECG
An ECG often reveals left bundle branch block or scar changes in the myocardium after a myocardial infarction, as well as cardiac arrhythmias, which can cause heart failure.
More information about the diagnostic method
Echocardiography
According to echocardiography (ultrasound of the heart), you can see the size of the heart chambers, zones of hypokinesis, aneurysms, and other reasons that lead to the appearance of heart failure. The main indicator that doctors focus on is the ejection fraction (a value expressed as a percentage), which reflects the capabilities of the heart and is an indicator of the efficiency of its work.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.