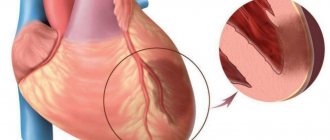
Extensive myocardial infarction (AMI) is one of the types of acute heart failure, which is accompanied by complete blockage of one of the heart vessels and a large area of myocardial necrosis.
The scientific name of the disease is non-Q wave myocardial infarction (MI) or non-ST segment elevation myocardial infarction. Let's consider the main reasons for the development of AMI, features of its manifestation, diagnosis, treatment, prognosis, chances of survival, and ways to reduce mortality.
There are several types of infarction, differing in the location of the area of necrosis:
- MI of the lateral wall of the left ventricular myocardium;
- MI of the posterior/anterior wall of the left ventricular myocardium;
- MI of the lower wall of the left ventricle myocardium (diaphragmatic);
- Right ventricular MI.
Causes of the disease
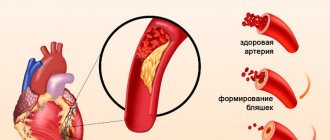
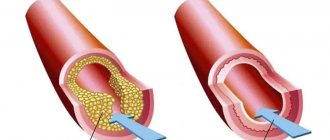
The cause of an extensive heart attack is thrombosis, which usually develops as a complication of atherosclerosis - the formation of an atherosclerotic plaque on the wall of a vessel.
When such a formation reaches a large size, it can rupture or become damaged, which provokes the formation of a blood clot. The thrombus clogs the lumen of the vessel, and the heart muscle cells stop receiving oxygen. This provokes the death of myocardial elements. The larger the area nourished by the clogged vessel, the more cells will die. If the patient is taken to the hospital quickly, doctors are able to remove the clot and reduce the area of necrosis.
Indirect causes of a large heart attack are called risk factors. They themselves do not cause AMI, but increase the likelihood of developing pathology. These include:
- older age;
- male gender;
- hereditary predisposition;
- violation of fat metabolism;
- arterial hypertension;
- obesity;
- diabetes;
- poor nutrition;
- passive lifestyle;
- smoking;
- alcohol abuse.
Diet after stenting
The diet after stenting includes foods rich in vitamins and fiber, but sharply limits the content of animal fats and the content of quickly digestible carbohydrates.
It is not recommended to eat fatty lamb, beef, pork, butter, lard, mayonnaise and spicy seasonings, sausages, cheese, caviar, pasta from non-durum wheat, chocolate, sweets and baked goods, white bread, coffee, strong tea, alcohol and beer, carbonated sweet drinks.
It is recommended to consume fresh vegetables and fruits, fresh juices, boiled poultry, fish, cereals, durum pasta, cottage cheese, fermented milk products, and green tea.
Symptoms, diagnosis of AMI
There are two types of symptoms of a major heart attack:
- typical;
- atypical.
Typical manifestations of AMI include:
- weakness;
- chest pain;
- shortness of breath;
- the pulse is usually rapid, but may be irregular;
- blood pressure may rise and then fall.
Some features distinguish chest pain in the pre-infarction state from attacks of ordinary angina:
- the pain is very intense, lasts 30-60 minutes;
- radiates to the neck, shoulder, jaw and scapula;
- does not go away after taking nitroglycerin tablets.
Atypical signs of the disease in their symptoms resemble other diseases: bronchial asthma, an attack of acute pancreatitis, stroke. Atypical pain is characterized by less severe chest pain.
Diagnosis of AMI involves instrumental examination:
- ECG;
- Ultrasound of the heart;
- determination of myocardial infarction markers in the blood (troponin, troponin-1, CPK, AST, LDH);
- general blood analysis;
- angiography of the coronary vessels.
Stages
An extensive heart attack develops in stages. Doctors identify five stages in the evolution of a dangerous disease:
- Pre-infarction state (prodromal period). This stage lasts from several hours to a month, for each patient individually. The patient has regular angina pectoris.
- The next stage is the most acute. It lasts approximately 30 minutes to 2 hours. A person experiences severe chest pain and breaks out in a cold sweat. In addition to this, the heart rate decreases or increases, and blood pressure decreases.
- The acute period of a heart attack is from 3 to 10 days. During this time, a patch of dying tissue forms in the heart muscle, pain dulls, arrhythmia and high body temperature appear.
- In the area of tissue death, a scar is formed, pain completely disappears, heart rhythm and blood pressure return to normal - all these are symptoms of the subacute stage of the development of a heart attack. The duration of this period is 4-5 weeks.
- The last stage of the disease is called post-infarction, the duration is from 3 months to six months. The characteristic symptoms of this period are an increase in the density of scar tissue and the adaptation of the “engine” to changed working conditions.
Features of treatment
Extensive myocardial infarction requires emergency treatment. The sooner the patient receives help, the greater the likelihood of a favorable outcome. There are two methods of treating AMI: medication and surgery. They can be combined with each other.
The goal of drug therapy is to prevent re-formation of a blood clot, dissolve an existing blood clot, reduce cardiac stress, improve blood supply to the myocardium, and eliminate the symptoms of a heart attack. For this, the patient is prescribed the following drugs and procedures:
- Painkillers, sedatives. Relieves pain and promotes vasodilation. The drugs of choice are nitroglycerin, morphine, fentanyl + droperidol.
- Oxygen therapy. The procedure is necessary for patients with insufficient oxygen saturation of arterial blood and acute heart failure.
- Antiplatelet agents, anticoagulants. Prevents recurrence of thrombosis. The drug of first choice is aspirin.
In addition, clopidogrel, ticagrelor, heparin, and bivalirudin are prescribed for AMI. - Thrombolytics. They destroy an existing blood clot and improve the prognosis. To treat a heart attack, one of four drugs is used: streptokinase, tenecteplase, alteplase, purolase.
- Beta blockers. They reduce the myocardial oxygen demand, reduce ischemia of the heart muscle, limit the affected area, and prevent the development of arrhythmia. The drugs of choice are esmolol, metoprolol, propranolol.
- Inhibitors of the renin-angiotensin system. Improves prognosis due to a positive effect on heart function. Representatives of the group are valsartan, captopril, ramipril, spironolactone.
Surgical treatment for extensive myocardial infarction allows you to quickly restore normal blood flow. Emergency techniques include percutaneous coronary intervention. This is a low-impact surgical procedure during which the doctor widens the narrowed area using a miniature catheter inserted through a large vessel. The end of the catheter is equipped with a balloon. Inflating and deflating it allows you to expand the lumen of the artery.
This procedure is called ballooning. If, after dilatation, the doctor installs a miniature frame (stent) inside the vessel, the operation is called stenting. Percutaneous coronary intervention is effective if less than 12 hours have passed since the onset of the attack.
Ultraviolet irradiation of blood
This method of treating the consequences of myocardial infarction, used in CBCP, also improves the quality of life after this disease. Does not require any surgical intervention in the patient's body. In this case, no blood is drawn: a special needle connected to a UV emitter is inserted into the patient’s vessel. The device affects a small volume of blood with low-power radiation, which is not felt at all by the patient.
Under the influence of UV radiation, a photochemical reaction occurs in the blood and plasma, as a result of which their composition and functionality improves. It is possible to achieve a significant reduction in blood viscosity (eliminate the risk of blood clots), activate metabolism, improve oxygen delivery to heart tissue, and dilate blood vessels.
Ultraviolet irradiation of blood attracts, first of all, its restorative effect. If you want to “rejuvenate” your heart without resorting to surgery, this method opens up wide possibilities for you.
Consequences, complications
The experience of MI does not pass without a trace. Heart muscle cells cannot reproduce. During the recovery period, the tissue defect is covered with connective tissue that is unable to perform the functions of the myocardium. Therefore, the heart cannot work at full strength. However, the consequences of a large heart attack can be much more serious. There are 6 groups of complications (6):
- ischemic: failure of reperfusion (failed percutaneous coronary intervention), post-infarction angina, recurrent infarction;
- mechanical: cardiac arrest, cardiogenic shock, myocardial rupture, disruption of the conduction system of the heart (sinus, atrioventricular nodes);
- arrhythmias: ventricular, atrial;
- thrombosis, embolism: of cerebral vessels or peripheral arteries;
- inflammatory: pericarditis;
- psychological: depression.
Prognosis, chances of survival
With extensive myocardial infarction, the prognosis is always unfavorable. The quality and life expectancy of a person will depend on the general state of health, timeliness and completeness of medical care.
About 5% of patients die during hospitalization. Over the course of a year, 36.7% of people will be hospitalized again with a heart attack, and 9% will die (5). According to other data, the overall mortality rate from heart attack is about 30%.
Factors influencing prognosis (4).
| Have a beneficial effect on the prognosis | Have an adverse effect on the prognosis |
| Fast medical assistance | Elderly age |
| Normal left ventricular function | Diabetes |
| Short-term, long-term treatment with aspirin, beta blockers, ACE inhibitors | Previous vascular diseases |
| Delayed or failed restoration of blood flow | |
| Left ventricular dysfunction (the most powerful indicator of poor outcome) | |
| Congestive heart failure | |
| Depression | |
| Increased levels of C-reactive protein (CRP factor) | |
| Characteristic changes in the cardiogram |
How to reduce mortality?
Extensive heart attack is a serious pathology leading to disability and death. People who survive an AMI are more likely to have relapses, each of which can be fatal.
You can improve your prognosis by seeking help with your first heart attack in a timely manner, following the recommendations of doctors. The goal of rehabilitation is to reduce the risk of complications and improve a person’s quality of life.
First aid
Full treatment is provided only to those admitted to the hospital less than 6 hours after the onset of the first pain. After this period, the use of certain medications no longer affects the prognosis. Therefore, if there is a suspicion that a person has had a heart attack, it is necessary to immediately call an ambulance.
Before the specialists arrive, the patient is provided with a flow of fresh air and the collar is stretched. The ideal position is half-sitting. The person is given an aspirin tablet to chew and swallow. Then a nitroglycerin tablet is placed under his tongue. In total, you can take up to 3 tablets with an interval of 5 minutes. The pain will not completely disappear, but the prognosis will improve significantly.
With the exception of aspirin and nitroglycerin, it is not recommended to give the patient other drugs. Ambulance workers will provide full medical assistance to the person.
Medicines
After a major heart attack, patients are prescribed medications that must be taken independently. Some of them will be canceled after a while, while others will be taken for life. The purpose of prescribing medications is to prevent complications and relapse of the disease.
List of recommended drugs for the prevention of complications of myocardial infarction (1).
| Medicine | Recommendations |
| Aspirin | Prescribed to all patients for life |
| Clopidogrel | Take for 1 year except in cases of high risk of bleeding |
| Beta blockers | In case of left ventricular failure, prescribed for life (ejection rate less than 35%) |
| ACE inhibitors, angiotensin 2 receptor antagonists | In case of left ventricular failure, they are prescribed for life (ejection rate less than 35%). Can be used in patients with normal left ventricular function |
| Veroshpiron | In case of left ventricular failure (ejection rate less than 35%), no impairment of kidney function, it is prescribed for life. |
| Statins (atorvastatin, rosuvastatin, simvastatin) | If there are no contraindications, they are prescribed to all patients for life. Target LDL level is less than 1.8 mmol/l |
Elimination of risk factors
Poor nutrition, a sedentary lifestyle, alcohol abuse, excess weight, and a negative psychological attitude significantly increase the likelihood of complications and death. Therefore, after discharge, patients are advised to reconsider their usual rhythm of life.
Smoking
Quitting smoking is recognized as one of the most effective preventive measures. Components of tobacco smoke contribute to blood clots. When you quit smoking, the likelihood of dying in the coming years decreases by 35-43% (1). People who are unable to cope with the addiction on their own are advised to seek help from specialists. Some medical institutions have special programs to help you quit smoking.
Psychological help
Depressed mood and fear of death are quite common among heart attack survivors. What helps to cope with a depressed state is doing what you love, communicating with loved ones. Persistent blues are a possible sign of depression. Such patients should consult their doctor. He will write a referral to a psychologist or recommend courses that teach people who have experienced a heart attack how to cope with stress.
Physical rehabilitation
Lack of physical activity has an extremely negative impact on the patient’s quality of life and prognosis. Lack of regular exercise has been shown to increase mortality by 26% (1). Therefore, physical rehabilitation of the patient begins from the first days after myocardial infarction (2). Regular exercise slows down the progression of atherosclerosis, improves heart function, reduces the risk of blood clots, and helps a person return to normal life faster.
After discharge from the hospital, it is necessary to maintain physical activity on your own. It is recommended to walk for at least 30 minutes/day, 5 days/week (3), do household chores, and do simple work in the garden. A history of AMI is not an absolute contraindication to more serious physical activity. On the contrary, they may be useful for some patients. However, before starting training, you should consult your doctor. Perhaps the planned load is unacceptable for you.
Weight loss
{banner_banstat9}
Body mass index more than 30 kg/m2, waist circumference more than 102 cm (men), 88 cm (women) are considered unhealthy indicators. Excess weight does not increase the likelihood of death, but it does influence other risk factors that increase mortality (1,3). Diet and physical activity are the safest ways to normalize weight.
Pressure control
Normalizing blood pressure (BP) reduces the likelihood of complications and relapses. It is recommended to maintain blood pressure at a level of up to 140/90 (1.2), and for patients with diabetes mellitus and kidney disease - up to 130/90 mm Hg. Art. (1). Reducing blood pressure is achieved through diet, lifestyle changes, and taking antihypertensive medications.
Treatment of type 2 diabetes mellitus
Type 2 diabetes increases the risk of developing cardiovascular disease. Treatment of the disease involves proper nutrition, an active lifestyle, and taking metformin or other medications that normalize sugar levels. A good result is considered to be achieving a glycated hemoglobin level of 7% or lower.
Flu prevention
Regular flu can cause serious cardiovascular complications with possible death. Therefore, all people who have experienced myocardial infarction are recommended to get vaccinated against the influenza virus annually and be especially careful during epidemics.
Further employment
{banner_banstat10}
There are types of work that are contraindicated for people who have survived a myocardial infarction. All of them are associated with increased stress on the heart or the inability to quickly provide medical care. These include:
- night or daily work;
- shifts longer than 8 hours;
- work that requires constant standing or involves continuous long walking;
- work away from populated areas;
- work associated with difficult working conditions: high humidity, high/low temperature;
- high-altitude work;
- working with toxic substances;
- work on board an airplane, helicopter.
After a heart attack, people also cannot work as air traffic controllers, railway control panels, power plants, public transport, or trucks. After all, a sudden repeated attack could lead to the death of a large number of people.
Ignoring doctors' recommendations when choosing a place to work increases the likelihood of death.
Goals and objectives of rehabilitation
Healed tissue has limited functionality, which leads to circulatory failure. The main goal of recovery after myocardial infarction is to adapt the body to new conditions. Program objectives:
- restoration of the cardiovascular system;
- psychological preparation of the patient, including the mindset for long-term rehabilitation in compliance with all doctor’s recommendations;
- prevention of possible complications - myocarditis, rhythm disturbances, aneurysm;
- general strengthening, preparing the patient’s body for stress, restoring physical indicators;
- return to work and a full life.
Prevention of MI
The only way to prevent the development of a large heart attack is to control risk factors for the development of the disease and seek medical help in a timely manner. It is important to eat right, be physically active, have a healthy weight, not smoke, and not abuse alcohol.
If you suffer from diabetes, hypertension, coronary heart disease, or have thyroid problems, do not start the disease. Visit your doctor on time and follow his instructions. Ignoring medical recommendations and undisciplined pill taking significantly increase the chances of developing AMI.
It is also necessary to undergo regular medical examinations and tests. Determining cholesterol and sugar levels, measuring blood pressure, and monitoring ECG help identify diseases at the earliest stages and take timely measures to prevent progression.
Medications after stenting
After stenting, it is imperative to take medications prescribed by the cardiologist, such as Plavix or Zilt, and aspirin, to prevent blockage of the stented vessels by a blood clot. The treating cardiologist will select the duration of administration and dosage individually.
And also, in the presence of concomitant diseases, for example hypertension - drugs that lower blood pressure, cholesterol-lowering drugs for high cholesterol levels in the blood, and other necessary medications that were taken before heart stenting.