© Author: A. Olesya Valerievna, candidate of medical sciences, practicing pathologist, teacher at a medical university, especially for SosudInfo.ru (about the authors)
Brain death means a complete and irreversible cessation of its vital activity, when the heart continues to beat and breathing is maintained through artificial ventilation (ALV).
Unfortunately, the number of patients who have irreversible events in the brain is large. Their treatment is carried out by resuscitation specialists, ensuring the maintenance of the main life support systems - breathing and circulation. From a medical and ethical point of view, it is always difficult to establish the fact of irreversibility of brain death, because this means declaring a person dead, although his heart continues to contract.
The brain lives after a person’s death for about five minutes, that is, after cardiac arrest, it is still able to maintain its activity for some time. During this period, it is very important to have time to carry out resuscitation, then there will be a chance for a full life. Otherwise, irreversible neuronal death will be fatal.
For relatives and friends, the issue of recognizing a sick relative as non-viable due to brain death is very difficult: many believe that a miracle will happen, others believe that doctors are not making enough efforts to “revive” the patient.
There are frequent cases of litigation and disputes when relatives consider the disconnection of the ventilator to be premature or erroneous. All these circumstances force us to objectify the data of symptoms, neurological and other types of examinations, so that an error is excluded, and the doctor who turned off the ventilator does not act as an executioner.
In Russia and most other countries, brain death is identified with the death of the whole organism, when maintaining the vital functions of other organs through medication and hardware treatment is impractical, which distinguishes brain death from a vegetative state and coma.
As already mentioned, under normal conditions, brain death occurs 5 minutes after breathing and heartbeat stop, but at low temperatures and various diseases this period can be lengthened or shortened. In addition, resuscitation measures and treatment can restore cardiac activity and provide ventilation of the lungs, but brain function cannot always be returned to its original state - comas, a vegetative state, or irreversible death of nervous tissue are possible, requiring different approaches from specialists.
Brain death established through clear criteria is the only reason when a doctor has the right to turn off all life support devices without the risk of being held legally liable. It is clear that such a formulation of the question requires compliance with all diagnostic algorithms for this condition, and an error is unacceptable.
Stages of diagnosing brain death
To accurately determine whether the brain is alive or whether irreversible and incompatible changes have already occurred in it, clear recommendations have been developed that should be followed by every specialist who encounters a patient in serious condition.
Diagnosis of brain death includes several stages:
- Accurate determination of the cause of the pathology.
- Exclusion of other brain changes that are clinically similar to his death, but under certain conditions can be reversible.
- Establishing the fact of cessation of activity of the entire brain, and not just its individual structures.
- Accurate determination of irreversibility of brain damage.
Based on clinical data, a doctor has the right to make a diagnosis of brain death without using additional instrumental diagnostic methods, since the developed criteria make it possible to determine the pathology with absolute accuracy. However, in our time, when the conclusion about any disease is based on a variety of objective results, instrumental and laboratory tests are involved in the diagnostic process.
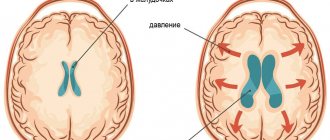
brain perfusion on MRI is normal (left), with brain death (center), with a vegetative state (right)
Additional examinations are not excluded from diagnostic algorithms for brain death, but are not strictly required. Their purpose is to speed up the establishment of the fact of brain death, especially in clinically complex cases, although it is quite possible to do without them. In Russia, only electroencephalography and angiography of the carotid and vertebral arteries are allowed as the only reliable ones in determining signs of irreversibility of brain disorders.
Prevention of the development of intravital extreme coma
Since this condition occurs secondary to other pathologies and diseases, measures to prevent it mainly come down to timely diagnosis and adequate treatment of the causative disorders.
It is important for the patient to follow the doctor’s recommendations, undergo the necessary examinations on time, and not violate the rules for taking prescribed medications.
In some cases, when there are serious reasons to fear the development of life-threatening conditions, it would be appropriate for the attending physician to pay attention to drugs that activate brain activity (for example, nootropic drugs).
Of course, this will not eliminate such a threat, but it may somewhat reduce it, or increase the time during which the patient can receive help.
Features and criteria for declaring brain death
In medicine, the concepts of clinical and biological death refer to the entire body, implying the reversibility or irreversibility of changes occurring. Applying this parameter to nervous tissue, we can speak of clinical brain death in the first 5 minutes after breathing stops, although the death of cortical neurons begins already in the third minute. Biological death characterizes a total disorder of brain activity that cannot be reversed by any resuscitation or treatment.
The need to assess the state of the brain usually arises in comatose and similar conditions, when the patient is unconscious, contact with him is impossible, hemodynamics and heart function may be unstable, breathing is usually supported by a device, the pelvic organs are not controlled, there is no movement and sensitivity, reflexes and muscle tone fades away.
Reanimation
The consequences of brain death are irreversible. Just because a person is unconscious does not mean that he needs to perform resuscitation measures (ventilation, cardiac massage).
Cardiac massage is strictly contraindicated if the victim’s heart is beating, even abnormally. In this case, massage can, on the contrary, interfere with the correct contraction of the heart muscles.
Mouth-to-mouth or mouth-to-nose breathing, as well as chest compressions, are performed only if there is no heartbeat. Such events can save a person's life. If you ensure the supply of oxygen to the body and improve blood circulation, irreversible necrotic changes will not occur. Body functions can be completely restored.
If a pregnant woman is injured, it is important to monitor not only her vital signs, but also the condition of the fetus. The patient must be taken to the hospital as quickly as possible, since the child may die due to injury and stress.
It is extremely important to thoroughly master resuscitation techniques. Any of us can master them and, if necessary, save a person’s life.
Assessment of causes of brain death
A doctor has the right to begin diagnosing biological brain death only when the causative factors and mechanisms of changes in nervous tissue are precisely known. The causes of irreversible brain disorders can be primary, caused by direct damage to the organ, and secondary.
Primary brain damage leading to brain death is provoked by:
- Severe traumatic brain injuries;
- Hemorrhages, both traumatic and spontaneous;
- Cerebral infarctions of any nature (atherosclerosis, thromboembolism);
- Oncological diseases;
- Acute hydrocephalus, edema;
- Previous surgical operations inside the skull.
Secondary irreversible damage occurs due to pathology of other organs and systems - cardiac arrest, shock, severe hypoxia against the background of systemic circulatory disorders, severe infectious processes, etc.
An important diagnostic step is the exclusion of all other pathological conditions that could manifest symptoms similar to brain death, but which, nevertheless, are potentially reversible with proper treatment. Thus, the diagnosis of brain death should not even be assumed until a specialist makes sure that there are no influences such as:
- Intoxication, drug poisoning;
- Hypothermia;
- Hypovolemic shock due to blood loss, dehydration;
- Coma of any origin;
- The effect of muscle relaxants, anesthetics.
In other words, an indispensable condition when diagnosing brain death will be the search for evidence that the symptoms are not caused by drugs that depress the nervous tissue, poisoning, metabolic disorders, or infections. In case of intoxication, appropriate treatment is carried out, but until its signs are eliminated, a conclusion about brain death is not considered. If all possible causes for the lack of brain functioning are excluded, then the question of its death will be raised.
When monitoring patients with brain disorders potentially associated with other causes, the rectal temperature is determined, which should not be less than 32 C, the systolic blood pressure is not less than 90 mm Hg. Art., and if it is lower, vasopressors are administered intravenously to maintain hemodynamics.
Clinical data analysis
The next stage in diagnosing brain death, which begins after establishing the causes and excluding other pathologies, will be the assessment of clinical data - coma, absence of brainstem reflexes, inability to spontaneously breathe (apnea).
Coma is a complete absence of consciousness. According to modern concepts, it is always accompanied by total atony of the muscular system. In a coma, the patient does not react to external stimuli, does not feel pain, changes in the temperature of surrounding objects, or touch.
Brainstem reflexes are determined in all patients without exception with possible brain death, while the following signs are always taken into account to verify the diagnosis:
- There is no response to sufficiently intense pain effects in the areas of exit of the branches of the trigeminal nerve or the absence of other reflexes, the arcs of which close above the cervical part of the spinal cord;
- The eyes do not move, the pupils do not react to a light stimulus (when it is clearly established that there is no effect of medications that dilate them);
- Corneal, oculovestibular, tracheal, pharyngeal and oculocephalic reflexes are not detected.
The absence of oculocephalic reflexes is determined by turning the patient's head to the sides with raised eyelids: if the eyes remain motionless, then there are no reflexes. This symptom is not assessed for cervical spine injuries.
checking oculocephalic reflexes
connection of oculocephalic and oculovestibular reflexes with brain stem vitality
To determine oculovestibular reflexes, the patient's head is raised, and cold water is pumped into the ear canals using a thin catheter. If the brain stem is active, the eyeballs will deviate to the sides. This symptom is not indicative of injury to the eardrums with a violation of their integrity. Pharyngeal and tracheal reflexes are checked by displacing the endotracheal tube or inserting a bronchial suction catheter.
One of the most important diagnostic criteria for brain death is the inability to breathe independently (apnea). This indicator is the final one at the stage of clinical assessment of brain functioning and can be determined only after checking all of the above parameters.
To determine whether a patient is able to breathe on his own or not, it is unacceptable to simply disconnect him from the ventilator equipment, since sudden hypoxia will have a detrimental effect on the already suffering brain and myocardium. Disconnection from the equipment is carried out on the basis of an apneic oxygenation test.
An apneic test involves monitoring the gas composition of the blood (the concentration of oxygen and carbon dioxide in it), for which a catheter is installed in the peripheral arteries. Before disconnecting the ventilator, ventilation of the lungs is carried out for a quarter of an hour under conditions of normal CO2 content and high oxygen pressure. After these two rules are observed, the ventilator is turned off, and humidified 100% oxygen is supplied to the trachea through the endotracheal tube.
If spontaneous breathing is possible, then an increase in the level of carbon dioxide in the blood will lead to activation of the stem nerve centers and the appearance of spontaneous respiratory movements. The presence of even minimal breathing serves as a reason to exclude brain death and immediately return to artificial ventilation of the respiratory system. A positive test result, that is, absence of breathing, will indicate irreversible death of the brain stem structures.
How does a doctor feel when he disconnects a person from the machines and takes away his organs?
Photo from vitals.nbcnews.com
- And another question, maybe not for you. If a person dies on the table, and you understand that he is a potential donor. That is, he died, but his organs can be removed and transplanted into someone else.
— I went to heart sampling several times.
I remember two months ago I went to a Moscow hospital. The guy is twenty-three years old, he was simply beaten near the metro, but they hit him with something so hard that his head was broken into two parts. They found his relatives, they signed permission to harvest his organs. A child needed a kidney, a woman and a man needed a liver - they divided it into two parts, a thirty-year-old man needed a heart. And now all the documents are signed, the patient is connected to the machines, and you stand on the fence, see this open skull and begin to put yourself in this guy’s place.
If you just came, the device turned off - that’s all. After all, brain death has already been declared, and you know that in 2-3 days irreversible changes will occur throughout the body. People with their heads cut into two parts cannot live. But I have to check all the documents again and again and sign that I agree to the fence. And then very carefully conduct the dynamics - so that God forbid the heart does not suffer from hypoxia, asystole. After all, the heart must be taken “alive”, warm.
I sometimes have dreams: the patient wakes up and says: “Why are you taking my heart?”
In general, this organ harvesting can be more difficult than even unsuccessful resuscitation. Because there you were doing something, fighting death, and here you have a living corpse lying. Nothing can be done, absolutely. Yesterday he lived, and then he was hit, or there was an accident, or a KAMAZ ran over him - there were many cases.
Screenshot from youtube.com
And when you turn off the devices, you shake all over, because you understand: “The person was just there, and now he’s gone.” And they begin to take away his organs.
And then you drive around the city with this heart with flashing lights. Then they went to save a thirty-year-old man. He served in the army, fell ill with a sore throat, and developed severe cardiomyopathy: his heart collapsed, only a transplant could save him. I also made a call from the clinic where the organs were taken away that I was bringing a heart, and the doctors made a skin incision in the patient and began to isolate the old heart. Not a minute is wasted here.
And then you see the same heart in another person, it works like your own, and the patient with a mask on his face after surgery shows you with a gesture: “I’m fine!” And here you switch things up a little, because, yes, one died, but thanks to him the life of the other was saved.
That time five people were saved, they will continue to live, continue their family line. And you understand that this is humane towards them - we did not let them die. And about the donor - again you think about fate: well, who really knew that he would go to the metro...
Observation and proof of irreversibility of pathology
In the absence of breathing, we can talk about the loss of vital activity of the entire brain; the doctor can only establish the fact that this process is completely irreversible. The irreversibility of brain disorders can be judged after a certain period of observation, depending on the cause of the pathology that caused the death of the nervous tissue.
If primary brain damage has occurred, then to establish brain death, the duration of observation must be at least 6 hours from the moment when the symptoms of the pathology were first recorded. After this period, a repeat neurological examination is performed, and the apnea test is no longer necessary.
Previously, it was recommended to observe the patient for a minimum of 12 hours, but now in most countries of the world the time has been reduced to 6 hours, since this time interval is considered sufficient to diagnose brain death. In addition, reducing observation time plays an important role when planning organ transplantation from a brain-dead patient.
In case of secondary damage to the nervous tissue, a longer observation is required to make a diagnosis of brain death - at least a day from the moment of the initial symptoms of the pathology. If there is reason to suspect poisoning, the time is increased to 72 hours, during which neurological monitoring is carried out every 2 hours. If the results are negative, brain death is declared after 72 hours.
Based on the stated diagnostic criteria, during observation of the patient, undoubted signs of brain death are recorded - the absence of reflex and brainstem activity, a positive apneic test. These parameters are considered absolutely indicative and reliable, not requiring additional examination, and therefore are used by doctors all over the world.
Additional examinations
Of the additional examinations that may affect the diagnosis, electroencephalography (EEG) and angiography are permitted. EEG is indicated for those patients for whom it is difficult to determine reflexes - in case of injuries or suspected injuries of the cervical spinal column, ruptured eardrums. An EEG is performed after all tests, including apnea. In brain death, it shows the absence of any electrical activity in the nerve tissue. If the indicators are questionable, the study can be repeated or using stimuli (light, pain).
non-collapsed cerebral vessels are normal on angiography
If EEG is indicated in clinically complex cases and does not affect the duration of general observation, then panangiography of the carotid and vertebral arteries is designed to shorten this time as much as possible. It is carried out at the final diagnostic stage and confirms the irreversibility of the cessation of brain activity.
For example, in case of possible intoxication, the patient should be observed for at least three days, but brain death can be determined early if, immediately after the appearance of signs of loss of its functions, the main arteries of the brain are examined twice with an interval of at least half an hour. In the absence of contrasting of the arteries, we can talk about a total and irreversible stop of cerebral blood flow, and further observation becomes impractical.
Video: example of an EEG to confirm brain death
Clinical diagnosis of biological brain death is labor-intensive, requires constant monitoring and maintenance of vital functions, so for many years the search has been underway for another method that would allow us to establish a reliable diagnosis with no less accuracy than the clinic. However, no matter how hard the experts try, none of the proposed methods is comparable in accuracy and reliability to a clinical assessment of the state of the brain. Moreover, other techniques are more complex, less accessible, invasive or not specific enough, and the result is greatly influenced by the experience and knowledge of the doctor.
The desire to speed up the process of ascertaining brain death is largely due to the rapid development of a new branch of medicine - transplantology. Considering the diagnosis of brain death from this position, we can say that the price of a conclusion about brain death may be not one, but several lives - both of the potential donor and of other people in need of organ transplants, therefore haste or non-compliance with the observation algorithm is unacceptable.
When deciding to declare brain death, the doctor must remember the ethical side of the issue and the fact that the life of any person is priceless, therefore strict compliance of his actions with the established rules and instructions is mandatory. A possible mistake increases the already high degree of responsibility, forcing you to repeatedly play it safe and doubt, double-check and weigh every step.
The diagnosis of brain death is established jointly by a resuscitation specialist and a neurologist, and each of them must have at least five years of work experience. If additional examination is necessary, specialists of other profiles are involved. Transplantologists and other persons involved in the collection and transplantation of organs cannot and should not participate in or influence the process of diagnosing brain death.
After diagnosis...
Once brain death has been confirmed by all clinical data, doctors have three options. In the first case, they can invite transplantologists to decide on the issue of organ collection for transplantation (this mechanism is regulated by the legislation of a particular country). In the second, talk to your family, explain the essence of the pathology and the irreversibility of brain damage, and then stop artificial ventilation. The third option, the most economically unprofitable and impractical, is to continue maintaining the functioning of the heart and lungs until they decompensate and the patient dies.
***
The problem of brain death with intact cardiac activity is not only of a medical nature. It has a significant moral, ethical and legal aspect. Society as a whole knows that brain death is identical to the death of the patient, but doctors have to make serious efforts, tact and patience when talking with relatives, deciding on transplantation issues and determining the final option of their actions after making a diagnosis.
Unfortunately, cases of distrust in doctors, unjustified suspicions of unwillingness to continue treatment, and accusations of negligence in their duties are still common. Many people still think that with a superficial assessment of the patient’s condition, the doctor will simply turn off the ventilator without making sure that the pathology is irreversible. At the same time, delving into the diagnostic algorithms, one can imagine how long and difficult the path to the final diagnosis is.
“What if he wakes up as a vegetable?”
Photo from health.usnews.com
— As far as I know, the same quantitative standards exist for resuscitation - according to the instructions of patients, it is necessary to resuscitate a certain number of minutes. What in practice?
- Six months ago there was a case when we resuscitated 245 minutes - and in general, according to the standards - half an hour.
Such a long resuscitation is a unique case, it is generally unrealistic. A young guy with a very severe heart defect. He was being prepared for surgery, and suddenly he began to die. We first gave him a closed cardiac massage, then an open one - the surgeons opened the chest. As a result, he came to life. Yes, then I was sick - there was cerebral edema, decompensation, multiple organ failure, respiratory failure. But he still had heart surgery, he was transferred to the ward and discharged, everything is stable there.
- So, according to your words, I understand that it is necessary to resuscitate until the last minute?
— We say, “until the victory.”
— Did you understand in your mind at that time that a guy could wake up like a vegetable, for example?
— Somewhere they understood, of course. But the guy, firstly, is young - he is nineteen years old. And we just felt that we had to go to the end - we administered special drugs in liters. But we saw from the monitors that there is hope. We see sinus rhythm - with disturbances, but we understand that we can fight it later, there are such drugs. They understood that all the regulations had already been exceeded, but they went on until the victory. And the boy was eventually saved.
It’s just that each specialist does his own thing. For example, a journalist is at war, and bullets fly past him. And he writes. You save. After all, nothing is known in advance exactly: what will happen to this person. What if everything will be fine?
- Go on the attack.
- Yes. You see, medicine is not mathematics.
It happens, for example: a patient is brought in and the operation of coronary artery bypass surgery went perfectly - literally from the incision to the skin suture. Male, safe, fifty years old, three shunts. After the operation, we are transported to the intensive care unit - suddenly there is asystole. Death.
Or vice versa - patients with severe cerebral edema, who were turned on, were pummeled with shocks, burned through the skin right to the bone and pumped to the point of broken ribs - they simply broke the sternum, but pumped the heart so that “the head would not fly off.” And in the end they had operations, post-resuscitation plastic surgery - and they came back, and everything was fine.
“There is an opinion that the doctors themselves, who imagine the resuscitation process and the possible consequences of severe diagnoses, ask: “Don’t pump me out.”
- I haven’t encountered anything like this. I saw something else. For example, an operation begins, and you put the patient under anesthesia, explain to him what will happen now - he will be tied to the table, he will fall asleep, and you explain what will happen when he wakes up. And several times patients, especially older ones, asked: “If I die, don’t open me up.”
I remember there was an incident - it was just some kind of mysticism, now I remember it, I still can’t wrap my head around it. The patient was engaged in making monuments.
And so he lies down on the table and says: “If I die, don’t open it. But in general, I’ve already knocked out a monument for myself, with a photograph, the full date of birth, but I didn’t sign the date of death.”
And I stand there, I have goosebumps: “What is he saying?” I thought I would cancel the operation altogether now. But then he calmed down and decided: “Okay, the person is just worried.”
This patient underwent surgery. Everything went perfectly, although it was hard - she walked for twelve hours. They bring him to the intensive care unit, he wakes up, everything is normal. And suddenly - once - cardiac arrest. We resuscitate him for an hour and a half, but he dies. The monument came in handy.
— How do doctors cope with the fact that they have done everything, and the person died? It turns out that what depends on the doctor?
- When this happens, then you think about it all the time, you replay the situation. Moreover, there can be several operations a day: you can leave with one and immediately go to pump a child who is dying in front of you.
Here it is important to repeat to yourself: you are not omnipotent, probably this is the fate of a person. And you shouldn’t give yourself any slack as a specialist – a surgeon, resuscitator or anesthesiologist. But sometimes I cry. You start thinking about life: “Why did he die so young?” You were with him, you went through some kind of hell, you tried to snatch him from death, but you couldn’t. These thoughts are in my head all the time. I don't know the answers.