Sudden death
Definition
. Sudden cardiac death (SCD) is defined as: “natural death due to cardiac causes, characterized by sudden loss of consciousness within one hour of the onset of symptoms; the presence of heart disease may be known, but the timing and mechanism of death is unpredictable.” The key concepts guiding the definition of sudden death are that the cause is non-traumatic and that the onset of death is immediate and unpredictable. When considering the problem of sudden death within heart diseases, the word “cardiac” was introduced into the term.
Sudden cardiac death: causes, prevention, first aid
The term “sudden cardiac death” usually refers to cases of death of persons who were in a stable condition, occurring within 1 hour from the onset of acute manifestations of the disease, in the absence of signs allowing for another diagnosis. In the problem of sudden death, the issue of circulatory arrest associated with cardiac arrhythmias is of greatest importance. Death associated with a sudden stop of blood circulation due to rhythm or conduction disturbances is called arrhythmic. The time of such death is calculated not in hours, but in minutes.
According to epidemiological studies, sudden circulatory arrest most often occurs in patients with coronary artery disease, which accounts for approximately 90% of sudden death. The remaining 10% of sudden arrhythmic death is associated with diseases that cause myocardial hypertrophy, myocarditis, alcoholic heart disease, mitral valve prolapse, cardiomyopathies, arrhythmogenic myocardial dysplasia, etc. It is known that sudden death can also occur in persons who do not have obvious signs of organic damage heart, resulting from the so-called idiopathic ventricular fibrillation.
The study of the causes and development factors of sudden death is one of the most pressing problems in cardiology. The importance of this problem is primarily due to the high frequency of sudden death. The significance of this problem is also due to the fact that the majority of those who suddenly die do not have severe organic changes in the heart that are incompatible with life. A significant proportion of patients with sudden circulatory arrest can be successfully resuscitated if they receive timely assistance.
Despite the advances made in the field of scientific medicine, in many cases it is not possible to identify potential victims of sudden arrhythmic death. In those who are at high risk of sudden circulatory arrest, the latter cannot always be prevented by available means. Therefore, the most important aspect of the fight against fatal arrhythmias is the timely implementation of resuscitation measures in the event of the development of circulatory arrest. Due to the fact that sudden arrhythmic death in most cases occurs outside of medical institutions, it is very important that not only medical workers, but also the general public are familiar with the basics of resuscitation care.
Sudden cardiac death
Sudden cardiac death (SCD) is defined as a natural death resulting from the cessation of effective cardiac function. As a rule, in this case, either ventricular fibrillation or primary cardiac arrest develops. The key concepts guiding the definition of sudden death are that the cause is non-traumatic and that the onset of death is immediate and unpredictable.
In almost 90% of cases, acute coronary death is caused by coronary heart disease. It also happens that before this, IHD did not manifest itself in any way, that is, it was asymptomatic. In some cases, the patient was bothered by angina attacks and arrhythmia. After a heart attack, the risk of sudden death increases several times.
Groups of people at high risk of SCD:
1. Patients who have undergone resuscitation due to cardiac arrest or ventricular fibrillation;
2. Patients with chronic heart failure and ischemia;
3. Persons with electrical instability in the conductive system;
4. Those diagnosed with significant cardiac hypertrophy.
In a quarter of all cases of sudden death of adults, there were no previous symptoms; it occurred without obvious reasons. Other patients noted a deterioration in their health one to two weeks before the attack in the form of: more frequent pain attacks in the heart area; increasing shortness of breath; a noticeable decrease in performance, feelings of fatigue and fatigue; more frequent episodes of arrhythmia and interruptions in cardiac activity. These signs can be considered harbingers of an impending threat; they indicate an exacerbation of existing heart problems, so it is advisable to consult a cardiologist when they appear.
Before cardiovascular death, pain in the heart area increases sharply, many patients manage to complain about it and experience severe fear, as happens with myocardial infarction. Psychomotor agitation is possible, the patient grabs the heart area, breathes noisily and frequently, gasps for air, sweating and redness of the face are possible. Nine out of ten cases of sudden coronary death occur outside the home, often against the background of strong emotional distress or physical overload, but it happens that the patient dies from acute coronary pathology in his sleep.
When ventricular fibrillation and cardiac arrest occur during an attack, severe weakness appears, dizziness begins, the patient loses consciousness and falls, breathing becomes noisy, and convulsions are possible due to deep hypoxia of the brain tissue.
Upon examination, pale skin is noted, the pupils dilate and stop responding to light, heart sounds cannot be heard due to their absence, and the pulse in large vessels is also not detected. In a matter of minutes, clinical death occurs with all its characteristic signs. Since the heart does not contract, the blood supply to all internal organs is disrupted, so within a few minutes after loss of consciousness and asystole, breathing disappears.
Since sudden cardiac death syndrome causes cardiac arrest and respiratory failure, the first step is to restore the functioning of life support organs. Emergency care should be started as early as possible and includes cardiopulmonary resuscitation and immediate transport of the patient to the hospital.
At the prehospital stage, the possibilities of resuscitation are limited; it is usually carried out by emergency specialists who find the patient in a variety of conditions - on the street, at home, at the workplace. It’s good if at the time of the attack there is a person nearby who knows her techniques - artificial respiration and chest compressions.
Sudden coronary death leads to irreversible changes in the cerebral cortex within 5-6 minutes. Therefore, emergency measures to restore blood flow must begin immediately and continue until the arrival of the medical team.
Every person needs to know the basics of cardiopulmonary resuscitation. Her tasks include checking and, if necessary, restoring the patency of the airways, starting artificial ventilation (mouth-to-mouth, mouth-to-nose), and chest compressions. According to the latest recommendations, a person without experience can skip the first two points and immediately begin cardiac massage. Several studies have shown that this approach is more effective and leads to improved survival.
Indirect cardiac massage should be performed as follows:
· Place the person on his back on a hard surface;
· Place your palms on the middle third of the sternum perpendicular to it;
· Start squeezing the chest without bending your elbows;
· The sternum should bend by 5 cm, and the frequency of movements should be about 100 per minute.
The effectiveness of resuscitation measures can be judged by the color of the skin.
Prevention of sudden coronary death is needed for people with chronic diseases of the cardiovascular system, which can cause an attack, as well as for those who have already survived it and were successfully resuscitated. To prevent a heart attack, a cardioverter defibrillator may be implanted, which is especially effective for serious arrhythmias. At the right moment, the device generates the impulse the heart needs and does not allow it to stop. Heart rhythm disturbances require medication support. Beta blockers, calcium channel blockers, and products containing omega-3 fatty acids are prescribed. Surgical prevention consists of operations aimed at eliminating arrhythmias. Nonspecific measures to prevent cardiac death are the same as for any other cardiac or vascular pathology - a healthy lifestyle, physical activity, giving up bad habits, proper nutrition.
GBUZ "Center for Medical Prevention" of the Ministry of Health of the Krasnodar Territory.
Causes
Epidemiology
. One of the leading causes of death in the adult population of developed countries is SCD due to coronary heart disease. In patients with sudden cardiovascular collapse, the rhythm of ventricular fibrillation is most often determined on the ECG (in 75-80% of cases), while bradyarrhythmias are the cause of SCD in a minimal number of patients. In 5-10% of cases of sudden cardiac death, patients do not have coronary heart disease or congestive heart failure. According to statistical data obtained annually in Western countries, the incidence of SCD varies from 0.6 – 1.28 per 1000 people per year. These studies only include data on those killed or resuscitated by emergency medical services; thus, official data are lower than the actual number of SCD cases in the general population.
Prevention of sudden cardiac death: general population and high-risk group. Among the adult population, the incidence of SCD is 1 in 1000 per year. Prophylactic interventions to reduce the risk of sudden cardiac death in this population appear to be neither practical nor cost-effective, since the costs include the remaining 999 per 1000 people per year who are not at risk for SCD. Thus, general principles of a healthy lifestyle are recommended in the general population.
Subgroups in which the annual risk of sudden cardiac death progressively increases are relatively few. It follows from this that promoting a healthy lifestyle among the population will naturally lead to a decrease in the number of patients with coronary heart disease, which in turn will reduce the number of cases of sudden cardiac death.
Causes of AHF
Automaticity of the heart - the ability to contract rhythmically can decrease due to heavy loads. Acute heart failure can manifest itself when the elasticity of the myocardial walls decreases due to inflammation caused by pathogenic bacteria and infections entering the patient’s blood after a viral disease (sore throat, meningitis, pneumonia, etc.). AHF can also be caused by diseases associated with impaired myocardial function.
In most cases, the patient's heart cannot eject the required volume of blood or accept the required amount into the ventricles. The main causes of acute heart failure:
- Diseases that reduce the contractile activity of the heart muscle: heart attack, myocarditis, surgery using an artificial respiration system.
- Weakening of the function of the heart muscle caused by impaired coronary circulation.
- Cardiac tamponade. Accumulation of fluid in the pericardial cavity, which leads to irregular contractions of the heart due to compression of the cavities.
- Hypertensive disease (hypertension), in which blood pressure rises above normal.
- Functional and morphological changes in the structure of heart valves and myocardium.
- Arterial hypertension, expressed as increased pressure in the system.
- Arrhythmia is a pathological condition that is accompanied by a violation of the heart rate, a change in the sequence and rhythm of heart contractions.
The following factors can also cause heart failure: focal brain damage due to stroke, electrical injury, brain injury, drug poisoning or ethyl alcohol intoxication.
Risk factors for sudden cardiac death in the population
| Non-modifiable risk factors | Modifiable risk factors |
| Age | Smoking |
| Male | Hypertension |
| Family history of coronary heart disease | Elevated LDL levels |
| Genetic factors | Diabetes |
| Obesity |
The heart did not hurt, but died suddenly: how to recognize ischemia in time?
Cardiovascular diseases have always been considered the main cause of mortality for humanity. It is surprising that many people still underestimate heart disease. Like, having cancer is the scourge of the 21st century. There is AIDS - the plague of the 21st century. There are road traffic injuries... This is what we need to fight. And my heart will ache and stop.
Although, if you look at the mortality statistics in Russia from various causes, 22% die annually from cancer, 3% from injuries (including road accidents), and less than 1% from AIDS. And the mortality rate from cardiovascular diseases in our country is 56%. That is, more than half of Russians die from heart disease! Almost 10 million people in our country, according to doctors, suffer from cardiovascular diseases.
We talked to specialists from the Voronezh Regional Clinical Center for Public Health and Medical Prevention about what are the main risk factors for cardiovascular diseases and what needs to be done to avoid heart disease.
What are the most dangerous cardiovascular diseases?
All cardiovascular diseases are divided into diseases of the heart, arteries and veins. The main danger is heart disease, and primarily coronary heart disease (CHD), since it is the main cause of mortality.
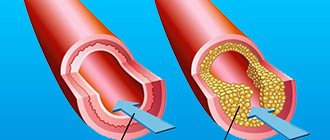
Coronary heart disease is a disease in which a person’s blood supply to the myocardium (heart muscle tissue) is disrupted due to pathologies of the coronary arteries
Many are accustomed to thinking that the manifestation of coronary artery disease is angina pectoris (a clinical syndrome characterized by a feeling of pain or discomfort in the chest). Most people think like this: if my heart hurts, then I’ll go to the doctor.
Indeed, in 50% of patients with coronary artery disease, angina pectoris is the first manifestation of the disease. But only 40–50% of patients with angina pectoris know about their disease. In the remaining 50–60% it remains unrecognized. People can live peacefully and not even suspect about the insidious disease. It may take many years before CAD causes sudden and catastrophic consequences.
It is important to understand that the first manifestation of coronary heart disease may be myocardial infarction or sudden death (according to the Framingham study of 5144 people - in men in 62%, in women in 46% of cases). The life of a man aged 60 is shortened by 9 years if he suffers a myocardial infarction, and by 12 if he suffers a stroke.
What are the risk factors for coronary heart disease?
Coronary heart disease is the end result of the interaction of a number of risk factors, which are divided into two groups - modifiable and non-modifiable risks.
Modifiable risks include those that a person can influence in some way - try to avoid them in his life, reduce or completely neutralize their impact. These are the majority of risks.
Unchangeable risks include risks that represent a certain reality, that is, conditions and circumstances that cannot be eliminated or influenced in any way. Fortunately, such risks are in the minority.
Below are the most significant risk factors that directly or indirectly affect the occurrence and development of IHD:
Lifestyle (modifiable risks):
- poor nutrition;
- smoking;
- excessive alcohol consumption;
- low physical activity;
- low social and educational status.
Biochemical or physiological factors (modifiable risks):
- high blood pressure;
- elevated cholesterol levels;
- elevated triglyceride levels;
- hyperglycemia/diabetes mellitus;
- obesity;
- thrombogenic factors;
- environmental pollution.
Individual characteristics (unchangeable risks):
- age (the older a person is, the higher the risk of developing IHD);
- gender (as statistics show, mortality from cardiovascular diseases in men under 65 years of age is 3 times higher than in women);
- heredity (early development of IHD in relatives).
What should you do to avoid IHD?
1. Analyze your lifestyle and, if there are these risks in it, try to get rid of them.
There are extremely effective things you can do right now. For example, quit smoking (if you smoke). Remember: quitting smoking reduces the risk of developing myocardial infarction by 36%! The risk of developing coronary heart disease (CHD) in a person who quits smoking within one year is reduced by 2 times compared to the same risk in a smoker, and after 15 years it is completely reduced to the level of the risk of a non-smoker.
2. Undergo a medical examination, which may identify risks associated with the physiological characteristics of the body.
Timely examination allows you to prevent the development of the disease, identify groups of people who need active preventive measures, increase the duration and improve the quality of life. In countries where primary prevention efforts have been active since 1970, cardiovascular morbidity has decreased significantly over the past 20 years. Thus, in the USA, Canada and the European Union, mortality from ischemic heart disease is more than 2 times lower, and from stroke – 5 times lower than in Russia.
The material was prepared within the framework of the national project “Demography”
Prevention of SCD: recommendations of the European Society of Cardiology
The European Society of Cardiology Specialist Group on Sudden Cardiac Death presents recommendations aimed at reducing the incidence of SCD. The recommendations are presented in tables and distributed as follows:
Class I:
Reliable evidence and/or consensus among experts that a given procedure or treatment is appropriate, beneficial and effective.
Class II:
Conflicting evidence and/or differences in expert opinion about the benefit/effectiveness of a procedure or treatment.
Class IIa:
evidence and/or expert opinion for benefit/effectiveness predominates.
Class IIb
: Benefit/effectiveness is not well supported by evidence and/or expert opinion.
In these guidelines, the terms “primary” and “secondary” prevention are used primarily in the context of ventricular arrhythmia. Therapy prescribed to prevent the development of sustained ventricular arrhythmias in patients without a history of episodes of life-threatening ventricular arrhythmias, but classified as at high risk for their development, refers to “primary” prevention. The therapy recommended for patients with cardiac arrest and syncope/hypotension secondary to paroxysmal ventricular tachycardia is “secondary” prevention.
What are the markers of SCD, what should you pay attention to?
- Sudden fainting (syncope) dizziness during exercise.
- Hypertrophic cardiomyopathy in relatives or a history of sudden death of relatives under 50 years of age.
- Severe left ventricular hypertrophy (>30mm).
- Unsustained ventricular tachycardia.
- Reduced blood pressure as a response to physical activity.
I. Myocardial infarction and heart failure
A. Risk stratification
Both non-invasive and invasive tests are used to determine the risk of SCD in patients with a history of myocardial infarction.
Risk stratification in patients who have had myocardial infarction
with/without development of HF
| Class | I | IIa | IIb |
| Demographic variability LVEF HR or BR sensitivity LV volume | ES unstable VT resting heart rate | Late potentials EPI Dynamics h. T Patency of the infarct-dependent artery |
LVEF – left ventricular ejection fraction; HR – rhythm variability
BR – baroreflex; ES – extrasystole; VT – ventricular tachycardia
HR – heart rate; h. T – T wave
B. Primary and secondary prevention of SCD in patients with a history of MI
Sudden cardiac death occurs most often among patients who have had a myocardial infarction. In this group, primary prevention includes drug treatment with beta blockers, aspirin, ACE inhibitors and cholesterol-lowering drugs. In patients with documented sustained VT or VF, the alternative is an implantable cardioverter-defibrillator (ICD) or amiodarone, and in selected cases, ablation or surgery. In patients with a history of myocardial infarction, a decrease in LVEF less than or equal to 40% (less than or equal to 5%) and clinically symptomatic paroxysms of non-sustained VT, or induced sustained or non-sustained VT by programmed electrical stimulation (EPS), the recommended treatment is CD implantation. For secondary prevention of SCD, the use of CD is recommended for those resuscitated after VF and patients with hemodynamically symptomatic VT paroxysms.
Primary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| History of MI | Beta blockers ACE inhibitors Cholesterol-lowering drugs Aspirin | Polyunsaturated fatty acids Amiodarone | |
| MI + LV dysfunction | Beta blockers ACE inhibitors Aldosterone receptor blockers | Amiodarone | |
| Hemodynamically asymptomatic VTs | Amiodarone Beta blockers | CD Ablation Surgical treatment | |
| LVEF less than or equal to 40% + paroxysms of non-sustained VT + inducible sustained VT with EPI | KD |
Secondary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| VF | KD | ||
| Hemodynamically symptomatic sustained VT | KD | Amiodarone Beta blockers |
II. Cardiomyopathies
Hypertrophic cardiomyopathy (HCM)
HCM is a relatively common cardiac disorder (incidence in adults approximately 1:500) in which sudden cardiac death is the most likely outcome at any age, but is most common in young, often asymptomatic patients. Implantation of a CD for the prevention of sudden cardiac death is strongly justified in patients who survive cardiac arrest (secondary prevention). Prophylactic use of KD is also possible in patients with two or more risk factors.
Hypertrophic cardiomyopathy
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Family history of SCD Syncope LV hypertrophy (VSD greater than cm) Unsustained VT Hypotension during exercise stress test | High risk of mutations |
| Primary prevention | KD | Amiodarone | |
| Secondary prevention | KD |
VSD – thickness of the interventricular septum
Arrhythmogenic right ventricular dysplasia (ARVD)
ARVD is one of the main causes of sudden cardiac death in the “pre-coronary” age group. Although the predisposing factors for SCD have not yet been sufficiently studied in large prospective studies, sudden cardiac death occurs more often in patients with significant changes in the right ventricle, as well as in those with LV involvement. In those resuscitated after SCD (secondary prevention), in patients with sustained VT and ineffective antiarrhythmic therapy, and in high-risk patients with documented paroxysms of VT, the most adequate treatment is CD implantation.
Arrhythmogenic right ventricular dysplasia
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT/VF Dilation of the RV RV dysfunction Inducible VT/VF with EPI | Family history of SCD Late potentials + LV dysfunction VT Inducible VT/VF with EPS | |
| Primary prevention | KD | Antiarrhythmic drugs | |
| Secondary prevention | KD |
RV – right ventricle; EPI – electrophysiological study
Dilated cardiomyopathy (DCM)
SCD is one of the most common mechanisms of death in DCM, especially in the early stages of the disease. Ejection fraction (EF) has been shown to be the most accurate predictor of outcome for both sudden cardiac death and death in advanced HF. The frequency of syncopal episodes is also considered one of the reliable risk factors for sudden cardiac death.
General therapeutic strategies aimed at reducing the risk of SCD in patients with DCM include the use of ACE inhibitors, beta blockers and aldosterone receptor antagonists, while amiodarone and CD implantation are used in individual cases. Several studies examining the role of antiarrhythmic drugs in patients with DCM have provided evidence (not statistically proven) that drug treatment recommended for patients who have had an MI with development of HF is equally effective in patients with DCM. The use of CDs for secondary prevention is considered acceptable; implantation of CDs is also recommended in high-risk patients for the primary prevention of sudden cardiac death.
Dilated cardiomyopathy
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Syncopations | Decreased EF Unsustained VT |
| Primary prevention | ACE inhibitors Beta blockers | KD Aldosterone receptor blockers | Amiodarone |
| Secondary prevention | KD ACE inhibitors Beta blockers | Aldosterone receptor blockers | Amiodarone |
Prevention of sudden death in patients with CHF
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
- Well, now I already see my friend, our friend - Professor Alexey Nikolaevich Turov. I would like to say that we are starting a new project - “Presentation of therapeutic basic schools in Russia.” And today, at the 33rd Internet session under the leadership of Professor Turov, we present... Well, in general, this school does not even need an introduction, but nevertheless. This is the Novosibirsk Research Institute of Circulatory Pathology named after Academician Meshalkin, which was created in 1957. The founder and first long-term leader was Academician Evgeniy Nikolaevich Meshalkin. In 2012, surgical high-tech treatment was carried out on 20 thousand patients. More than 70 thousand people were consulted. The bulk of the interventions were carried out using federal budget funds. And this institute is the largest executor of the state federal task in the profile of cardiovascular surgery.
Aleksey Nikolaevich is generally an innovator, a very passionate and enthusiastic person about medicine. You'll see it now. He represents the program, today he shaped it. Therefore, all the pros, all the cons – everything goes to him. I want to say that Alexey Nikolaevich is a Doctor of Medical Sciences, Associate Professor of the Department of Internal Medicine, Faculty of Medicine, Novosibirsk University, leading researcher at the Center for Surgical Arrhythmology at the Meshalkin Research Institute of Circulatory Pathology; popularizer of catheter technologies for heart rate correction, author of many electroanatomical mapping techniques, co-author of a new direction in the treatment of atrial fibrillation, ablation of the ganglion plexuses of the left atrium. And he was the initiator of the creation of the electrophysiological society.
Well, Alexey Nikolaevich, it’s almost 20 o’clock for you, and we’re listening to you with impatience, as usual.
Alexey Nikolaevich Turov , associate professor, doctor of medical sciences:
– Good afternoon, dear colleagues. Thank you very much for such a flattering introduction. And today we will begin to talk about the problem of sudden cardiac death. Today I would like to talk about this problem in relation to a very narrow category of patients, namely patients with heart failure.
Of course, there is no need to talk about how pressing the problem of sudden death is. The United States has the greatest statistics. And we see that in this country, sudden death is the number one killer. That is, it claims more than 450 thousand lives annually. And this is much more than the four leading causes of death combined: strokes, lung cancer, breast cancer and HIV infection. That is, this is really currently the number one problem not only in cardiology.
If we look at the structure of sudden cardiac death, we will see that 88% are still life-threatening arrhythmias, that is, sudden cardiac death can rightfully be equated in terminology to sudden arrhythmic death. If we now look at the structure of life-threatening arrhythmias, we will see that primary ventricular fibrillation develops very rarely. Bradyrhythmic death is also a fairly rare situation. Torsade de pointes tachycardias are rarely a cause of death. And the most common situation is rapid ventricular tachycardia, which, having begun, then transforms into ventricular flutter, then into large-wave ventricular fibrillation, then into small-wave ventricular fibrillation, and everything ends with secondary asystole.
We see that this entire process takes only a few minutes. And we also know that the success of resuscitation efforts is determined by time. Every minute the chances of saving a patient's life decrease by 10%. Therefore, if we started resuscitation measures by the ninth minute, then this probability is no more than 10%, and if we started resuscitation measures within the first minute, then this is the greatest chance of saving the patient. This is why resuscitators talk about the so-called “golden” first minute. Naturally, during the history of the development of cardiology, there were a lot of social aspects, social events, the task of which was precisely to bring medical care as close as possible, so that resuscitation was provided to the patient within the first minute.
Here are some of these social strategies. First of all, this is the territorial concentration of patients with cardiac pathology. This concept has been developed in some capitals, in some countries, where patients with severe cardiac pathology have benefits for settling in certain areas, which, as they say, are stuffed with specialized cardiological institutions. Then specialized help arrives within a few minutes.
Then, there are specialized highways on which the passage of cardiac intensive care vehicles is allowed, which are devoid of speed limits and traffic lights, and can reach speeds of more than 100 kilometers per hour. Again, in a matter of minutes a doctor can be in any area of the city. The so-called air medicine service, cardiological medicine, solves the problem of traffic jams even more.
Finally, in the United States in the late 1980s, so-called Early Defibrillation programs were actively developed. They were aimed at ensuring that the first person who saw another person fall would begin resuscitation using external automatic defibrillators. These are, as they say, smart devices that are able to independently recognize the state of the patient’s rhythm. And if this condition is life-threatening, they will perform cardioversion using special technology, according to a special algorithm. This program included awareness of the general population, mass placement of external automatic defibrillators in those places where the maximum outburst of emotions occurs: stadiums, airports, railway stations, film holdings, casinos, and so on; and a video surveillance system. All these social programs, of course, bring some great benefits. But nevertheless, we must not forget that all of them are designed for first aid to others so that the surrounding people detect a cardiac catastrophe. At the same time, we know that 40% of all sudden deaths occur without any witnesses. And 80% of all cases of sudden death occur not in society, but at home. And besides this, we also know that the time for defibrillation and the time for resuscitation still could not be reduced to this first, so-called “golden” minute.
If we use modern ambulance teams in large cities, then on average help begins at the 24th minute. If medical towns are the sixth minute. Specialized highways - the fifth minute, helicopters - the fourth minute. The Early Defibrillation program still begins to operate, starting from the second minute after the patient falls. And please note that only an implantable cardioverter-defibrillator, a fully automatically implanted device, allows you to deliver this first life-giving shock, the first shock, within the first 30 seconds. Therefore, they naturally have no alternative, not in terms of other social activities, not in terms of medications.
Therefore, nothing more can be said about implantable cardioverter defibrillators other than that they are a life-saving device. Currently, these devices have shrunk in size to virtually the size of pacemakers. And here we see an example of a printout from this device, when this device detected a dangerous, life-threatening arrhythmia, ventricular flutter. Delivered a 10 joule shock and restored sinus rhythm. Please note that all of this took only seven seconds. That is, a life-threatening, dangerous situation passed within seven seconds. Of course, we can no longer talk about any other alternative in terms of preventing sudden death, sudden arrhythmic death.
Which patients are at greatest risk for sudden death? Let's look at the most common Bigger risk stratification. Bigger divided the risk of sudden death into three classes. These are benign situations, potentially malignant situations and malignant situations. Please note that the basis was based on three factors. This is a lesion of the heart, this is the structure of the arrhythmia and the clinical picture that the patient has. Moreover, Bigger gave primary importance to the degree of heart damage. If it is absent, this is a benign class; if there is gross cardiac pathology, this is the second class. And if there is a complicated, severe cardiac pathology, reduced ejection fraction, severe hypertrophy, left ventricular aneurysm - this is the third class.
The structure of arrhythmia is of secondary importance. Thus, if a patient has sustained ventricular tachycardia, but at the same time he has a completely anatomically healthy heart, there is no cardiac pathology, then this patient still ends up in first class. That is, in the benign class for the risk of sudden death. And on the contrary, if the patient has only ventricular extrasystoles, single extrasystoles, but at the same time a low ejection fraction - below 40% - he nevertheless finds himself in the third class, that is, he has a malignant class for the risk of sudden death.
Thus, dear colleagues, it is the ejection fraction that is the main, most important risk factor for sudden death, in which all other other factors are already dissolved. And an ejection fraction below 30% increases the risk of sudden death by more than eight times.
We know that there are many cardiac drugs available. We know of numerous studies in which these drugs showed a decrease in mortality in patients with cardiac pathology: beta blockers, aspirin, statins, ACE inhibitors. But please look, despite the reduction in overall mortality, in all these studies the rate of sudden death is high. Half of the patients in these studies died suddenly. Therefore, it is no secret that, of course, there were studies in which cardioverter-defibrillators were studied in patients with heart failure, where the main target was not ventricular arrhythmia, but rather low systolic function of the left ventricle.
And the first such study was the Madit study. It involved 196 patients. All of these patients had previously suffered a myocardial infarction. Please note that they had non-sustained ventricular tachycardia. Unsustained ventricular tachycardia is an arrhythmia that exists for no more than 20 seconds. That is, this is an arrhythmia that was accidentally detected during daily monitoring. All patients had low ejection fraction. And these patients underwent an intracardiac electrophysiological study, during which monomorphic ventricular tachycardia was induced. And she was refractory to intravenous procainamide, a powerful antiarrhythmic drug.
It was clear that if such a malignant situation, then, of course, cardioverters should have a powerful preventive effect in terms of sudden death. Indeed, cardioverter defibrillators increased patient survival by 75% compared with traditional therapy.
The next study is the Mustt study. It had a somewhat confusing design. But what should interest us is that these, again, were patients who had suffered a myocardial infarction. But the ejection fraction has already been increased to 40%. Again, all patients underwent electrophysiological intracardiac testing. Ventricular tachycardia was induced in all. And after that, patients were randomized based on electrophysiological testing. Some patients received cardioverter defibrillators, and some patients received antiarrhythmic drugs based on intracardiac electrophysiological studies. These were a variety of drugs: Amiodarone, Sotalol, drugs of the first “A” class. And 46% received cardioverter defibrillators.
As a result, when five-year mortality was assessed, it turned out that therapy that was selected on the basis of intracardiac EPS reduced the five-year mortality of these patients. But when this therapy was divided into two branches, it turned out that implantation of EPS-based cardioverter-defibrillators actually halved the five-year mortality rate.
But please pay attention. Antiarrhythmic drugs, which were selected on the basis of EPI, on the contrary, increased five-year mortality. It was as a result of this study that the management of patients changed. And at present, intracardiac electrophysiological testing is not required for high-risk patients. As they say, the researchers concentrated as much as possible on a single factor, namely, the ejection fraction.
The next study, Definite, addressed non-ischemic heart failure for the first time. This is 458 patients with an ejection fraction below 35%. Again, let's see that the ventricular events were completely asymptomatic. As a result, arrhythmic mortality decreased by 80% under the influence of cardioverter defibrillators. But when overall mortality was assessed, it turned out that it also decreased by 35%, but these differences were not significant. Therefore, this study temporarily suspended the study of cardioverters in patients with non-ischemic etiology.
The next study is the Madit-II study, which again returned to post-infarction patients. Please note that the inclusion criterion does not have any arrhythmic criterion. This is a previous heart attack and low ejection fraction. The patients were divided into two groups. 742 patients received a cardioverter-defibrillator. As a result, patients in the cardioverter-defibrillator group had a 31% better survival rate compared to patients who received traditional therapy.
And finally, the last and largest study is SCD-HeFT. It included more than two thousand patients, long-term, multi-year observation. It, again, returned to any form of heart failure. This study included patients with both ischemic and nonischemic failure. The main criterion was low ejection fraction. And again, please note: at the time of inclusion there were no arrhythmic indications for implantation of cardioverter defibrillators and stimulators. The study took place at 168 sites in North America and New Zealand. Patients were divided into three groups: patients receiving placebo, amiodarone, or an implantable cardioverter defibrillator.
As a result, the five-year mortality rate was lowest in the implantable cardioverter-defibrillator group. So, cardioverter-defibrillators significantly reduced mortality in the group of these patients by 23%. But the effect of Amiodarone was completely unreliable. Moreover, such a positive effect of cardioverter-defibrillators was noted both in ischemic heart failure and also in patients with non-ischemic heart failure: they reduced mortality by 27%. In summary, this study definitively defined the indication as severe systolic dysfunction, regardless of its etiology.
What types of mortality are affected by cardioverters? First of all, of course, on arrhythmic mortality. They reduce the likelihood of death from life-threatening arrhythmias by 61% on average. As a result, cardiac mortality also decreases, because the final outcome of many cardiac accidents is also ventricular fibrillation. Finally, overall mortality also decreases by 31%.
This analysis of the Madit-II study shows who the ideal patient is for cardioverter implantation. This is a patient, regardless of age and gender, but this is a patient with the lowest ejection fraction, and at the same time with the lowest functional class of heart failure. That is, the ideal patient for a cardioverter-defibrillator is a patient who has extremely low left ventricular systolic function, but at the same time a mild clinical picture of heart failure, not terminal - a manifestation of heart failure.
What are the current indications for implantation of cardioverter-defibrillators in patients with heart failure? The first indication is ischemic heart failure with an ejection fraction below 40%. In this case, there is a certain postscript: no earlier than 40 days after myocardial infarction. Where did this addition come from? The Dynamit study was conducted in which cardioverter defibrillators were tried to be implanted in the early stages after myocardial infarction - before the 40th day. These were, again, patients with extremely low ejection fraction. But as a result, it turned out that the mortality rate in both groups - in patients with defibrillators and those without - was not different at all. That is, the tactic of installing defibrillators in the early stages after myocardial infarction did not justify itself.
If we are talking about non-ischemic etiology, non-ischemic heart failure, then this should be an ejection fraction below 35%.
And the third group are patients who are waiting for a heart transplant outside the hospital.
I would like to give one example. This is a 33-year-old young man who had dilated cardiomyopathy. Ejection fraction – 23%, functional class of heart failure – three. This patient did not initially have any arrhythmic indication for a defibrillator. That is, he had only a single ventricular systole; he never had any ventricular tachycardia. A cardioverter-defibrillator was implanted in him in 2005. Please note: 11 months passed before the device worked for the first time. And on the printout obtained from this device, we see the reason for the operation. The patient did experience rapid ventricular tachycardia at a rate of 220 beats per minute. And it was effectively stopped with a single discharge from the cardioverter-defibrillator. Subsequently, this patient was regularly monitored by us. He underwent a heart transplant. And this patient is currently alive.
Let's now turn to what would have happened if this patient had not had at that time, October 2, 2006, a cardioverter-defibrillator - a device that (I would like to emphasize again) was installed prophylactically in a patient who did not have any arrhythmic events.
But there is a group of patients for whom cardioverter implantation is not indicated. These are patients whose life expectancy in the satisfactory functional class is less than one year. The wording is very complex, it must be interpreted as follows. These are patients who have extracardiac pathology, very severe, multi-organ pathology, which does not allow predicting the preservation of quality of life for a long time. That is, these patients are likely to die from non-cardiac pathology.
The second group consists of patients with the fourth functional class of heart failure. Implantation of a cardioverter-defibrillator is not indicated in them due to the fact that these patients die mainly from heart failure, from cardiac accidents, compared to patients from milder functional classes, who die mainly from sudden cardiac death, from life-threatening arrhythmias .
Finally, cardioverter implantation is not indicated for patients if they require myocardial revascularization. This indication, again, was confirmed by a multicenter study. The CABG-PATCH study, which was conducted in the late 90s. It included patients with ischemic heart failure and low ejection fraction. It would seem that patients are suitable for cardioverter implantation. But these patients needed coronary artery bypass grafting. And they were divided into two groups. One group consists of patients with isolated coronary artery bypass grafting, the second group consists of patients who also underwent implantation of a cardioverter during bypass surgery.
As a result, please note: the two-year mortality rate was completely indistinguishable. That is, patients who are indicated for cardiac surgical correction of the disease do not need cardioverter implantation. They need to first correct the cause of severe systolic dysfunction.
Thus, dear colleagues, many doctors believe that cardioverter-defibrillators are always associated with some kind of life-threatening arrhythmias, ventricular tachycardia or sudden death is necessary - this is absolutely not the case. The main candidates for cardioverter implantation are patients at high risk of sudden death. If your patient has an ejection fraction below 40%, especially below 35%, he has a functional class of heart failure from first to third, it is impossible for him to undergo radical cardiac surgery, angioplasty, coronary artery bypass grafting, valve replacement, and so on, then this patient is absolutely implantation of a cardioverter-defibrillator is indicated.
Also, many doctors say: “This is a very expensive approach, it is not for our country. And our domestic patients will never receive a cardioverter-defibrillator.” This is absolutely not true. Let's look at this slide. One of the most important economic criteria is the Number Needed to Treat criterion: how many patients, how many years need to be treated in order to save one year of life for any patient. It turns out that cardioverter-defibrillators are the most convenient, most economically rational approach. They appear to be more cost-effective than ACE inhibitors, beta blockers, statins and amiodarone when it comes to preventing sudden cardiac death.
And we see that even in the United States, where the indications for implantable cardioverters are very expanded, these devices are funded significantly less compared to the huge field of pharmacotherapy for cardiac patients.
Let's look at the structure of indications for implantation of cardioverter-defibrillators. We see that it has changed over the years. In 1998, the largest category of patients with implantable defibrillators were patients who had previously experienced sudden death. Then, in the early 2000s, the largest category of patients were patients with ventricular tachycardia, that is, what is called an arrhythmic indication for implantation of devices. Finally, over the past four years, the largest category of patients has been high-risk patients who have not yet experienced any arrhythmic events.
I would also like to cite the experience of our own institution. This is the structure of our implantable cardioverter defibrillators. We see that only 3% are patients who previously suffered sudden death. A small number of patients with UIQT syndrome and hypertrophic cardiopathy. 34% of patients who have arrhythmic indications have ventricular tachycardia. And the largest number of patients are patients with severe systolic dysfunction.
And in our budget, in the budget of our country, budget funding for these devices is provided. And here is the code for high-tech medical care, which involves implantation of a cardioverter-defibrillator. Thus, any citizen of Russia has the right to receive this device for free. And only in relation to our institution, I would like to cite statistics: 450 new cardioverter-defibrillators are implanted in our clinic alone every year.
Thus, dear colleagues, summing up my speech. If you are seeing a patient with a low ejection fraction for whom radical cardiac surgery is not indicated or is not possible, then it is advisable to refer him to an interventional arrhythmologist. And this patient will be implanted with such a complex, smart device completely free of charge using government funding. Thank you for your attention.
III. Genetic pathology of ion channels
QT prolongation
Long QT syndrome is associated with a high risk of sudden cardiac death. Risk stratification is mainly based on the presence of syncope, Torsades de Pointe (VT) and a history of cardiac arrest. Primary prevention of SCD is generally based on treatment with beta blockers. CD implantation is recommended for secondary prevention, as well as in patients with VT/VF with a history of adequate treatment with beta blockers.
QT prolongation
| Class | I | IIa | IIb |
| Risk stratification | Torsade de pointes/VF/cardiac arrest Syncope Jervell–Lange-Nielsen syndrome QT prolongation | QT greater than 600 ms Development of VT/VF in childhood Prolongation of QT + AV block Macroscopically dynamic T waves Female gender Postpartum period | Family history of SCD Increased QT interval dispersion |
| Primary prevention | Avoid drugs that prolong the QT interval Beta blockers Avoid strenuous exercise | Sympathetic denervation of the LV pacemaker | |
| Secondary prevention | KD + beta blockers + avoid drugs that prolong the QT interval Avoid intense exercise |
ECS - electrical pacemaker
Brugada syndrome
Diagnosis of Brugada syndrome (BS) is based on the presence of spontaneous or inducible ST segment elevation in leads V1-V with or without right bundle branch block (RBBB). Risk stratification is still poorly defined, and the role of EPS in identifying patients with high-risk factors is debated. In survivors of cardiac arrest, CD implantation is recommended. Prophylactic use of KD in high-risk populations is strongly recommended, but this approach is limited by the lack of clearly defined risk criteria.
Brugada syndrome
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Syncope Family history of SCD | Inducible VT/VF during EPI |
| Primary prevention | CD in patients with syncope/VT | KD in asymptomatic patients with VT induced by EPI | |
| Secondary prevention | KD |
Catecholaminergic polymorphic ventricular tachycardia
To date, there is no precise definition of catecholaminergic polymorphic ventricular tachycardia (CPVT), since large-scale studies are not possible. This disease is associated with a high risk of sudden cardiac death at a young age, but criteria for stratification are lacking. Prevention of sudden cardiac death is based on the use of beta blockers; KDs are recommended for secondary prevention, since the significance of KDs for primary prevention has not been determined.
Catecholaminergic polymorphic ventricular tachycardia
| Class | I | IIa | IIb |
| Risk stratification | VF | Family history of SCD Unsustained VT/syncope in childhood | Syncopations |
| Primary prevention | Beta blockers | KD | |
| Secondary prevention | KD + beta blockers | Beta blockers |
IV. Valve pathology
Aortic stenosis
Among patients whose cause of death is aortic stenosis (AS), about 20% are sudden cardiac death. In the absence of symptoms, the survival rate of patients with AS is high even without valve replacement. The prognostic value of various hemodynamic and electrophysiological studies is limited. Asymptomatic patients with hemodynamically severe aortic stenosis should be under constant observation and, if symptoms develop, undergo immediate surgery. In patients with documented sustained ventricular tachycardia, cardiac implantation should be considered.
Aortic stenosis
| Class | I | IIa | IIb |
| Risk stratification | Syncope Angina | VT, including those induced by EPS Decreased exercise tolerance | Significant stenosis |
| Primary prevention | Surgery | Amiodarone | |
| Secondary prevention | KD |
Mitral valve prolapse
Mitral valve prolapse (MVP) generally has a favorable prognosis; There are suggestions about the risk of sudden cardiac death, but there is no evidence. Most cases of SCD are described in patients who have previously suffered syncope or cardiac arrest, a family history of SCD at a young age, with severe prolapse or myxomatous changes in the mitral valve leaflets. For patients surviving cardiac arrest, CD implantation is recommended.
Mitral valve prolapse
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Family history of SCD Severe prolapse or myxomatous changes in the leaflets | QT prolongation Frequent/group ES Inducible VT/VF with EPS Mitral valve regurgitation Late potentials |
| Primary prevention | |||
| Secondary prevention | KD |
Why do young people die?
The risk group includes not only older people. In approximately 5% of cases, sudden death due to heart disease occurs in young people. The following conditions provoke it:
- sharp and prolonged vasospasm;
- significant myocardial hypertrophy;
- physical and psycho-emotional overload;
- taking drugs, alcoholism and smoking;
- cardiomyopathy.
Almost half of the dead were obese, a quarter of them were smokers, and 10% had insulin-dependent diabetes mellitus. Approximately 5% had a family history of similar episodes.
Interesting Facts
Scientists conducted studies in which it was noted that death from heart failure at a young age was most often correlated with structural features of the musculoskeletal system. The dead were:
- high asthenics;
- with signs of discrepancy between the two front teeth;
- with curvatures of the sternum, spine and lower extremities.
Also at risk were young people who had disturbances in the structure of the cardiovascular system:
- increased tortuosity of the aorta;
- reduction in the diameter of the largest artery;
- drop-shaped or reduced in size heart.
Symptoms and diseases
A study of cases of mortality from cardiac pathology in young people showed that some time before death they had the following symptoms:
- headache and dizziness;
- loss of consciousness;
- pressure surges;
- rhythm and conduction disturbances;
- mitral valve prolapse;
- vegetative-vascular dystonia of the hypertensive type.
V. Pathology of the coronary arteries
Anomalous origin of the coronary arteries
SCD most often occurs in patients with an anomalous origin of the trunk of the left coronary artery from the right or non-coronary sinus of Valsalva. Therefore, special attention should be paid to young patients with chest pain similar in description to angina. Surgery is the most appropriate treatment option for patients at high risk of sudden cardiac death.
Anomalous origin of the coronary arteries
| Class | I | IIa | IIb |
| Risk stratification | VF | Young patients with angina or a positive stress test | |
| Primary prevention | Surgery | ||
| Secondary prevention | Surgery |
Myocardial bridges
The long-term prognosis for patients with the presence of myocardial bridges seems favorable, but in some cases this pathology can cause the development of tachyarrhythmias or sudden cardiac death. In symptomatic patients, quantitative coronary angiography, Doppler, and intravascular ultrasound are used to diagnose myocardial bridges. Drug treatment with beta blockers, surgery, angioplasty and coronary artery stenting are alternative treatments.
Myocardial bridges
| Class | I | IIa | IIb |
| Risk stratification | Symptomatic VT VF | Myocardial ischemia | |
| Primary prevention | Surgical treatment in patients with myocardial ischemia | Beta blockers | |
| Secondary prevention | Surgical treatment in patients with myocardial ischemia |
What are the causes of SCD in young athletes?
In 80% of cases, SCD occurs in athletes over 35 years of age and is due to atheromatosis of the coronary arteries. But, given the fact that in elite sports sudden death of very young athletes (<35 years old) has become increasingly common, the main focus of the study is directed specifically at them.
SCD is based on hereditary, congenital structural abnormalities, as well as abnormalities of the conduction system of the heart (electrical abnormalities).
The most common cause of sudden death in young athletes is cardiomyopathies. There are several types: hypertrophic cardiomyopathy, arrhythmogenic right ventricular hypertrophy, idiopathic left ventricular hypertrophy and dilated cardiomyopathy. Given that the first two species account for almost 50% (Bruckner et al 2013) of sudden death in young athletes reported in the literature, we will focus on them.
Hypertrophic cardiomyopathy. An inherited condition characterized by thickening of the heart muscle in the left ventricle. At maximum and submaximal loads, it disrupts the functioning of the conduction system of the heart, causing fibrillation.
Arrhythmogenic right ventricular cardiomyopathy: is also an autosomal dominant hereditary condition. This disorder predominantly affects the right ventricle, although in severe cases it may also affect the left ventricle. The condition is characterized by the replacement of myocardial cells with a connective-fatty structure, which, due to such anatomical changes, has a key effect on the conduction system of the heart and is fatal during severe chronic physical exertion.
Congenital abnormalities in the structure of the coronary arteries cause 1/5 of the incidents of sudden death among young athletes. Such abnormal connections between coronary arteries can be compressed by hypertrophied myocardium, causing acute ischemia. Sudden death in the setting of normal cardiac structure is primarily due to congenital ion channel defects and accounts for approximately 4% of sudden deaths in sports. Such conditions include long QT syndrome, Brugada syndrome, ventricular arrhythmias due to a sharp increase in catecholamines, short QT syndrome, WPW syndrome, severe electrolyte disturbances, hypothermia and hyperthermia, drugs (amphetamine, cocaine). Other causes include cardiac arrhythmias due to myocarditis due to infection.
Commodio cordis may be another cause of sudden death in young healthy people, resulting from blunt mechanical shock to the chest (in contact sports), which during the vulnerable phase of myocardial repolarization can cause fatal ventricular fibrillation.
VI. Wolff-Parkinson-White syndrome (WPW)
According to modern research, in patients with WPW syndrome, the incidence of sudden cardiac death is 0.15% per year. The main cause of SCD is the transition of atrial fibrillation with a rapid ventricular response to ventricular fibrillation. Survivors of resuscitation for sudden cardiac death are typically characterized by the absence of symptoms, shortened RR intervals (less than 250 ms) during paroxysmal atrial fibrillation, and the presence of multiple or posteroseptal accessory pathways. Electrophysiological study with atrial excitation and determination of RR intervals between preexcited QRS complexes has high sensitivity, but specificity and significance in determining a positive predictor are limited. In patients at high risk for SCD, catheter ablation is recommended, particularly in those resuscitated from ventricular fibrillation or in patients with symptomatic episodes of atrial fibrillation with a rapid ventricular response.
Wolff-Parkinson-White syndrome
| Class | I | IIa | IIb |
| Risk stratification | less than 250 ms cycle duration in AF less than 270 ms anterograde refractory period of additional pathways Multiple additional pathways | Cessation of pre-excitation during treatment with ajmaline | |
| Primary prevention | Ablation for atrial fibrillation and the presence of rapid conduction through accessory pathways | Ablation in asymptomatic patients with – family history of SCD – athletes | Amiodarone Antiarrhythmic drugs classes Ia and Ic |
| Secondary prevention | Ablation |
VII. Bradyarrhythmias
It has been established that bradyarrhythmias are the cause of sudden cardiac death in 15-20% of cases. Risk factors for bradyarrhythmic death include high-degree AV block with intraventricular conduction disturbances, but in the presence of structural changes in the heart, these factors may predispose to the development of tachyarrhythmias. Pacing is the treatment of choice in high-risk patients with bradyarrhythmia: it relieves symptoms and may reduce mortality.
Risk stratification for cardiac conduction disorders
| Class | I | IIa | IIb |
| Profound AV block | AV block III degree AV block II degree, type II Syncope Combination of heart disease with CHF | ||
| Congenital AV block of the third degree | Syncope QT prolongation Congenital heart disease | ||
| Chronic two- or three-fascicle blockade | Combination of heart disease with CHF | Syncope Conduction from the Hiss bundle to the ventricles 100 ms (HV interval 100 ms) Intraventricular blocks Blocks induced during EPI |
Out-of-hospital resuscitation
Survival after cardiac arrest varies from 5% to 60% depending on the characteristics of the cardiac arrest (ie, cardiac etiology or not; verified or not; ventricular fibrillation or not). The outcome of cardiopulmonary resuscitation (CPR) is influenced not only by the success of its implementation, but also by the patient’s condition before the start of CPR.
It is now generally accepted that time to electrical defibrillation is the single most significant determinant of survival after cardiac arrest.
The instructions for the automatic external defibrillator allow defibrillation in cases of out-of-hospital ventricular fibrillation or ventricular tachycardia to people of non-medical professions, often many minutes before the arrival of the ambulance team. This strategy is known in the West as “first responder defibrillation,” based on the principle of mutual aid.