A problem in which the blood does not clot well is called a bleeding disorder. It is caused by the fact that blood vessels do not normally become blocked when they are damaged.
When everything is fine, when there is bleeding at the wound site, the blood begins to thicken, which prevents large losses. But sometimes this complex mechanism fails, resulting in severe or prolonged bleeding.
When blood does not clot well, this does not always lead to external loss. It can also appear as bleeding under the skin or in the brain.
Causes
Bleeding disorders are divided depending on the etiology - acquired, genetically determined and congenital, as well as autoimmune.
Blood clotting disorders can be caused by hereditary pathologies, but not only. Genetic diseases can also influence the development of the disease. For example, a newborn baby may be diagnosed with hemophilia or von Willebrand disease.
Also, the disorder can be caused by a lack of vitamin K. In addition, such problems can be a consequence of cancer of the liver and other organs.
Most often, bleeding disorders occur due to infectious hepatitis or scarring, which usually occurs with cirrhosis.
Long-term use of strong antibiotics or drugs to treat blood clots can also cause bleeding problems.
Consequences of increased blood clotting
Under these conditions, the risk of blood clots is significantly increased. Inflammation of thrombosed veins leads to thrombophlebitis, accompanied by:
- pain;
- swelling;
- redness of the skin over the vein.
Blood clots in blood vessels lead to narrowing of their lumen and damage to tissue areas due to a lack of blood supply. When blood flow through a vessel is completely stopped due to a blood clot, an area deprived of blood supply appears in the tissue, which is called an ischemic focus. In this area, cells quickly die and the normal functioning of the organ is disrupted. Irreversible damage to the brain and heart are the most dangerous consequences of thrombosis. Another insidious complication is the detachment of a blood clot. Often the diameter of the blood clot is smaller than the diameter of the vessel, so the patient is unaware of its presence for a long time. However, with injuries and concussions of the body, at the beginning of taking medications that thin the blood, as well as when getting up on your feet after a long stay in bed (for example, after surgery), the clot can break off and continue to move through the bloodstream until it clogs the lumen of the vessel somewhere. It is because of such blood clots that a formidable and very dangerous complication develops - pulmonary embolism, which can result in the death of a person if medical assistance is not provided in time. They can only be detected by carrying out certain studies, including a general blood test for blood clotting.
Symptoms
Main symptoms of the disease:
- Skin rashes. Depending on the cause of poor coagulation, both small pinpoint hemorrhages (petechiae) and extensive hematomas may appear on the skin.
- Nosebleeds.
- Hemorrhages in the mucous membranes of the mouth, nose, and intestines. The latter option can lead to the appearance of blood in the stool.
- Hemorrhages in the brain. Occurs with fragility of blood vessels and low blood clotting.
- In the event of an injury, cut, or bruise, the bleeding does not stop for a long time.
- Hemorrhages in joints, muscles and internal organs can be observed with the hereditary disease hemophilia. Bruises (hematomas) can form even with minor mechanical damage.
Hypocoagulation: symptoms, why the pathology is dangerous
Nosebleeds for no reason, bleeding of mucous membranes when brushing your teeth, spontaneous appearance of bruises and bleeding from your finger that you cannot stop for longer than usual - all these are still harmless signs of reduced coagulability.
The real danger awaits carriers of the pathology during surgical operations, increased blood pressure, after childbirth, and even routine tooth extraction at the dentist.
Diseases associated with blood hypocoagulation
| Name | Pathogenesis – mechanism of occurrence and development | Why is pathology dangerous? | How is it diagnosed? |
| Thrombocytopenia | A decrease in the number of platelets in plasma (less than 150 × 10 * 9 g/l), associated with a violation of their production or rapid decay. The pathology can be congenital, more often acquired due to bone marrow damage, deficiency of vitamins B9 and B12, severe infections, and splenomegaly. | Risk of massive blood loss, internal, uterine bleeding, miscarriage, hemorrhagic stroke. Prohibition on physical activity, restriction of vital activity. | Clinical blood test Hemostasiogram |
| Thrombocytopenic purpura, ITP (Wergolf's disease) | An autoimmune disease that occurs in a chronic form and is more common in young women. With ITP, the amount of IgG on the surface of platelets increases 10 times. The appearance is provoked by viruses, bacteria, and taking certain medications. | Ophthalmic hemorrhages, decreased visual acuity. Skin hemorrhages - petechial rash, purpura. Uterine bleeding, spontaneous abortion, stroke. | Titer for antibodies to platelets General blood test Coagulogram |
| Hemophilia | Inherited with the maternal X chromosome in an autosomal recessive manner. There are 3 forms of the disease, the most common is classical hemophilia A. | Hemorrhages in muscles, internal organs, and joints, and associated disability. | Thromboelastography, APTT Tests for antihemophilic globulin and D-dimer Prothrombin test Coagulogram |
| von Willebrand disease | Associated with a mutation in the hemostasis gene located on chromosome 12. There are 4 forms of pathology - from mild, with asymptomatic carriage, to severe, with gastric, uterine and other types of bleeding. | Genetic risk of bleeding from any organs, premature birth, hemorrhagic stroke - bleeding in the brain with increased blood pressure. | Study of the activity and properties of von Willebrand factor Activity of ADAMTS 13, 8th coagulation factor |
To treat hypocoagulable conditions, corticosteroids and immunosuppressants are used, and the missing antihemophilic globulin (coagulation factor VIII) or platelet concentrate is administered.
Treatment
For treatment of this condition to be effective, the causes of the disease must be determined. It is very important to promptly identify and treat the main disorders - liver pathologies or oncological lesions.
Additional therapy methods include:
- injection of vitamin K;
- drugs to improve clotting;
- transfusion of frozen blood plasma;
- Other medications include hydroxyurea and oprelvekin, which help eliminate platelet problems.
The patient's diet should include foods high in calcium, folic acid, vikasol, and amino acids.
These include dairy products: cheese, cottage cheese, kefir. Fish and meat will also help eliminate the symptoms of pathology. It is equally important to eat leafy vegetables - green onions, spinach, cabbage.
Bleeding disorders
Some people are terribly afraid of the sight of a cut finger, especially their own, but this fear is irrational. A healthy person simply cannot bleed through even fairly large cuts, since nature has provided us with an excellent blood clotting mechanism. But how can you tell if clotting has worsened?
Who clots the blood
The hemostasis system (stopping bleeding) consists of two parts - vascular-platelet and coagulation, also known as plasma.
The vascular-platelet unit acts as follows: at the moment of injury, damaged cells of the vessel wall release a number of special substances that activate platelets. As a result, platelets become entangled with each other, forming a loose mass, and acquire the ability for adhesion (sticking to the damaged area of the vessel) and aggregation (sticking together into piles). This is how a primary loose thrombus is formed. For capillary bleeding (cut finger) it is enough, but in large vessels where blood moves at high speed, such a design will simply be “knocked out” by the pressure.
Therefore, a coagulation link is necessary - this is the actual coagulation. Coagulation factors (FCs) are constantly present in the blood plasma, and in such quantities that it would be enough for almost all the blood at once (this suggests a plot for a horror film). But, like platelets, PS are in an inactive state until the wounded vascular wall emits its biochemical “cry for help.” Once activated, coagulation factors form a three-dimensional network of fibrin, the task of which is to wrap the primary thrombus, strengthening it and firmly fixing it on the damaged area.
Irregularities in the work of the first link
Since the first link has two components, problems can arise with any of them. Decreased coagulation of platelet origin can have two reasons: a decrease in the number of platelets or their genetic inferiority. Increased fragility of the vascular wall (also, as a rule, genetically determined) also leads to bleeding.
Any of these options will make itself felt by easily occurring bruises that appear “from nowhere,” that is, with such light blows that a person does not even remember; Frequent nasal, gingival, and, in women, uterine bleeding are also typical.
Types of laboratory tests for clotting
The content of the article
The blood clotting test includes the following indicators:
- Fibrinogen levels
This substance is a protein produced by the liver. In a healthy person, fibrogen is 2-4 g/l. - Antithrombin III.
This is a hemocoagulation regulator. The antithrombin index is 75-125% in adults, 80-120% in children older than one month, and 30-80% in newborns. - Prothrombin index (PTI)
. The percentage ratio of hemocoagulation time in a particular person with a similar indicator in the control sample. Normally, PTI is 93-107%. - Thrombin time.
In healthy people it ranges from 14 to 20 seconds. During this period, prothrombin must be transformed into thrombin. The results may vary with the use of certain medications, such as aspirin or warfarin. The thrombin time (PT) test shows how well a person's blood clots. - Activated partial thromboplastin time (aPTT)
. The indicator is used to monitor the hemocoagulation process in patients prescribed heparin and in the diagnosis of DIC syndrome. Normally, this figure is 29-39 seconds. - Period (time) of bleeding.
Indicates how quickly the blood will stop if the integrity of small vessels is violated. To do this, a puncture is made on the patient's finger and the time is noted. Normally it is 2-3 minutes. - Clotting time.
Determined by the time interval between blood sampling and clot formation. In healthy people, this process takes from 2 to 5 minutes. - D-dimer
. This is a substance formed as a result of the decomposition of fibrin. Normally, this figure should be no more than 250 mcg/l (0.25 mcg/ml).
The bleeding must stop
Blood as an organ
1. Purves, William K. Life: The Science of Biology.
— 7th. — Sunderland, Mass: Sinauer Associates, 2004. The human body is made up of dozens of organs, most of which have a specific shape and size. But there is one, the main one - it does not have clear boundaries, but the work of all other systems of the body depends on its condition. This is our blood, which consists of plasma and formed elements - red blood cells, platelets and leukocytes. Plasma is the liquid part of the blood that contains water and substances suspended in it: proteins and other compounds.
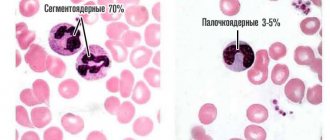
Formed elements of blood
2. Turgeon ML Clinical Hematology: Theory and Procedures. — Lippincott Williams & Wilkins, 2004.
Erythrocytes (red blood cells) are the most numerous of the formed elements. Red blood cells contain a special protein - hemoglobin, which ensures the main function of red blood cells - oxygen transport. It is hemoglobin that gives red blood cells and blood in general their red color.
Figure 1. Formed elements of blood
Platelets (blood platelets) are fragments of giant cells in the bone marrow. Together with plasma proteins, they ensure rapid clotting of blood flowing from a damaged blood vessel, which stops bleeding and thereby protects the body from blood loss.
Leukocytes (white blood cells) are part of the body's immune system. They can extend beyond the blood vessels into the tissue. The main functions of leukocytes are participation in immune reactions and protection against foreign bodies or substances. Under normal conditions, there are much fewer leukocytes in the blood than other formed elements.
Balance of blood coagulation and anticoagulation systems
3. Colman RW Hemostasis and thrombosis basic principles and clinical practice / Ed. G. I. Kozints and V. A. Makarov. — Philadelphia: Lippincott, 1993.
In the human body, as in any living system, a natural balance of various indicators is constantly maintained. In the case of blood, this is the continuous maintenance of balance between coagulation and anticoagulation factors, since one of the main conditions for optimal life activity is maintaining blood in a liquid state and timely restoration of damaged walls of blood vessels.
4. Human physiology. Ed. Pokrovsky V. M., Korotko G. F. 2nd ed., revised. and additional - M.: 2003.
On the one hand, microscopic clots constantly form in the bloodstream, which do not manifest themselves in any way. On the other hand, certain proteins with the opposite effect continuously control the formation of even the smallest fibrin networks, which could at any moment become larger, which would consequently lead to the development of thrombosis.
Factors that disturb this delicate balance, such as even minor damage to the wall of a blood vessel, lead to an acceleration of blood clotting time and the formation of larger blood clots that are visible to the naked eye. Therefore, it is not surprising that an artificial heart valve can also disrupt the natural balance of the coagulation and anticoagulation systems.
Measuring blood clotting requires a simple clotting time test to calculate the international normalized ratio (INR) using an automated clotting analyzer.
The lower the INR, the faster the blood clots, that is, the “thicker” it is. The higher the INR, the longer the blood clots, that is, the “thinner” it is and the higher the risk of bleeding.
A blood clotting test will allow you to select the most optimal dosage of anticoagulants.
Who needs to determine blood clotting?
To reduce the risk of developing vascular accidents and unexpected bleeding, it is necessary to periodically monitor the state of the blood coagulation system using a laboratory method. This is especially important for:
- people over 40 years old;
- women during and after menopause;
- women during pregnancy;
- people who regularly take blood thinners (aspirin);
- patients suffering from varicose veins;
- those preparing for surgery, etc.
The doctor must prescribe blood clotting tests if hemophilia is suspected (usually this disease is detected in early childhood and young adulthood) or when treating an existing thrombosis with fibrinolytic therapy and anticoagulants.
1.What is hemophilia and its causes
Hemophilia
is a blood disorder in which the blood does not clot properly. Typically, this occurs because a person with hemophilia lacks a certain clotting factor. This means it can be difficult to stop bleeding. Moreover, this can apply to both ordinary bleeding from wounds and falls, and bleeding during some operations. It also happens that some people with hemophilia begin to bleed internally for no apparent reason.
There are two main types of hemophilia:
- Hemophilia A
is caused by the absence of active blood clotting factor VIII. According to statistics, approximately 1 in 5,000 male infants are born with type A hemophilia. Blood clotting factor VIII is a plasma protein. The greater the deficiency, the more severe the symptoms of hemophilia. - Hemophilia B
(Christmas disease) is caused by a lack of active blood clotting factor IX in the body. This form of hemophilia is less common and is diagnosed in about 1 in 30,000 male infants.
Hemophilia is usually inherited and almost always affects men. In very rare cases, a person can develop hemophilia without a family history. This is called acquired hemophilia, and it occurs in both men and women.
Causes of hemophilia
Hemophilia, both type A and B, occurs due to a defect in a pair of chromosomes that affects the presence of a certain blood clotting factor in the body and how it works. In the case of acquired hemophilia, the blood clotting factor stops working as it should because it begins to be attacked by antibodies that the body itself produces.
A must read! Help with treatment and hospitalization!
conclusions
Quite often, increased blood viscosity is a result of poor nutrition. Therefore, you should be attentive to your diet and adjust it as necessary. Sometimes, simple dietary restrictions can protect a person from stroke, heart attack and other serious pathologies.
It is best to contact a specialist who will assess the person’s condition and help create a nutrition plan.
But the cause of increased blood viscosity is not always a food problem. It is often one of the pathological mechanisms of complex diseases such as diabetes or other metabolic disorders. In this case, contacting a nutritionist is not enough; you need to make an appointment with an endocrinologist. Only he will be able to correctly assess the situation and adjust the treatment.