TREATMENT FOR VASCULITIS IS AVAILABLE AT BRANCHES:
Treatment of vasculitis in the Primorsky region
Address: St. Petersburg , Primorsky district, st. Repisheva, 13
Treatment of vasculitis in the Petrograd region
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
The disease is usually accompanied by complications. Intestinal bleeding may occur from the gastrointestinal tract. Vasculitis can also cause liver damage. In the cardiovascular system, disorders such as cardiomyopathy and disruption of the heart valves can form. The most dangerous consequence of vasculitis is stroke. In the excretory system, a possible complication is glomerulonephritis.
2. Reasons
Allergic arteriolitis is considered a polyetiological disease, the causes and risk factors of which include acute and chronic infections (and the localization of the trigger focus can be almost any, but more often it is the nasopharynx and/or oral cavity), as well as circulatory disorders, for example, with varicose veins or chronic heart failure. Some authors describe the mechanism of development of Reiter's vasculitis as infectious-allergic, others emphasize the role of immune or autoimmune factors.
Visit our Allergology page
Vasculitis - Causes and risk factors
Vascular inflammation is believed to be initiated by immune processes (associated with hypersensitivity reactions to antigens). For example, some diseases classified as systemic small vessel inflammation are associated with the presence of antineutrophil cytoplasmic antibodies. Allergic vasculitis is provoked by allergic reactions of the body. Cerebral vasculitis can occur as a complication of an infectious disease, tumor, or as a result of isolated damage to the blood vessels of the brain.
Vasculitis - types
1. Systemic vasculitis of small vessels (arterioles, capillaries and veins)
- Wegener's granulomatosis is a necrotizing vasculitis affecting the respiratory tract, eyes, kidneys and other organs.
- Microscopic polyangiitis - necrotizing vasculitis with damage to the lungs and kidneys, without the formation of granulomas
- Eosinophilic granulomatous vasculitis (Churg-Strauss syndrome)
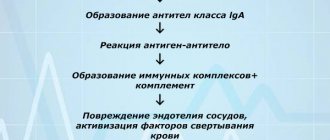
- Hemorrhagic vasculitis associated with the deposition of IgA immunoglobulins (Henoch-Schönlein purpura) is characterized by damage to the skin, intestines and kidneys, accompanied by arthritis and arthralgia. This type of vasculitis most often occurs in children aged 4-7 years.
- Cutaneous leukocytoclastic vasculitis - isolated vasculitis without systemic involvement
2. Systemic vasculitis of medium vessels (visceral vessels, mesenteric, renal arteries, etc.)
- Polyarteritis of the arteries is a focal lesion of the arteries, which occurs with rupture of aneurysms and bleeding; infarction of organs and tissues is possible.
- Kawasaki disease is a vascular inflammation with mucocutaneous lymphatic syndrome that can affect the coronary arteries.
3. Systemic vasculitis of large vessels (aorta and large branches)
- Giant cell arteritis (Horton's disease) is a granulomatous arteritis, combined with polymyalgia rheumatica (pain in the shoulder and pelvic girdle), in patients over 50 years of age.
- Takayasu arteritis is a progressive inflammation of the aorta that often occurs in young women.
4. Mixed vasculitis (Behcet's syndrome)
In addition, vasculitis is divided into:
- Primary - the cause of the disease is unknown
- Secondary - changes in blood vessels are caused by other diseases (for example, rheumatoid arthritis, systemic lupus erythematosus) or are a side effect of medications
Hemorrhagic vasculitis in children
Schönlein-Henoch disease (hemorrhagic vasculitis, rheumatic purpura, allergic purpura) is a disease from the group of systemic vasculitis with predominant damage to the microvasculature of the skin, joints, gastrointestinal tract and kidneys.In 1837, Schonlein described a disease characterized by rashes on the skin of the legs (purpura), as well as pain and swelling of the joints. The author noted that rashes of small hemorrhagic spots and pain in the joints are wavy in nature, and called this symptom complex purpura rheumatics. In 1868, Henoch reported on 4 sick children who, along with joint pain and skin purpura, had colicky abdominal pain, vomiting with blood, and intestinal bleeding. He described this syndrome under the name purpura abdominalis. Somewhat later, Henoch drew attention to the damage to the kidneys during this suffering. In 1887, Henoch described another form - purpura fulminans. In this form, skin rashes, joint and abdominal syndromes were especially acute. Rapidly developing, they gave a threatening clinical picture, which almost always ended in death. Until 1890, purpura rheumatics, purpura abdominalis and purpura fulminans were considered to be separate and distinct diseases. This was explained by the diversity of the clinical picture and the lack of generalized material. Only in 1890, von Dusch and Gohe summarized the cases of this disease and came to the conclusion that it is one disease with different clinical symptoms and called it Schönlein-Henoch disease (HSD).
HSP is the most common disease in childhood from the group of systemic vasculitis. It is common in France, Great Britain, Japan, Finland, Singapore and Taiwan. People of the Negroid race and the South American population are less likely to get sick. In Russia it occurs in 23-26 people per 10 thousand children. The disease can begin at any age. However, children under 3 years of age rarely get sick. The maximum number of cases of HSP occurs at the age of 4-12 years.
Etiology. BSH remains unclear. Some authors associate the occurrence of the disease with various infections (viral or bacterial), others attach greater importance to the allergic mood of the body, which in the presence of foci of chronic infections (chronic tonsillitis, caries, tuberculosis, etc.) leads to a decrease in the reactivity of the child’s body. The onset of HSP is possible 1-4 weeks after a sore throat, acute respiratory viral infection, scarlet fever or other infectious disease. In a number of patients, the development of the disease is preceded by vaccination, drug intolerance, food allergies, trauma, and cooling. The listed factors are more likely to be permissive than etiological.
The disease is based on overproduction of low-molecular-weight circulating immune complexes, activation of the complement system, increased vascular permeability, damage to the endothelium of microcirculatory vessels with subsequent involvement of the hemostatic system in the process, leading to platelet hyperaggregation and hypercoagulation, that is, the development of systemic microthrombovasculitis.
As a rule, the disease begins acutely. The clinical picture of HSP is characterized by various combinations of typical syndromes: cutaneous hemorrhagic, articular, abdominal and renal, and rarely - pathology of other organs. About 50% of patients at the onset have an increase in temperature to low-grade levels; higher fever is possible in patients with abdominal syndrome. The onset of the disease is often polysyndromic, less often monosyndromic (skin lesions). Moreover, a monosyndromic onset does not mean that the subsequent process will not be systemic in nature.
In most children, HSP begins with typical skin rashes - these are small-spotted or maculopapular, symmetrically located hemorrhagic elements that do not disappear with pressure. The rash is localized on the extensor surfaces of the extremities, around the joints, and on the buttocks. Rashes on the skin of the face, torso, palms and feet are less common. The intensity of the rash varies - from single to multiple elements with a tendency to merge. In severe cases of the disease with a pronounced exudative component, individual elements with necrosis may appear. Depending on the course of the disease, the rash may recur. When it fades, pigmentation remains, in place of which, with frequent relapses, peeling appears. A typical hemorrhagic rash is a pathognomonic, obligatory symptom of HSP. In some cases, patients experience angioedema (usually on the face, hands, feet).
Joint damage is the second characteristic symptom of HSP, observed in 2/3 of patients. Usually it appears simultaneously with a hemorrhagic rash in the 1st week of illness, or at a later date. The nature of joint damage varies from short-term arthralgia to arthritis. Large joints are predominantly affected, especially the knees and ankles. Periarticular edema develops with joint deformation and pain; joint pain lasts from several hours to several days. There is no permanent deformation of joints with impairment of their function.
Abdominal is the third most common clinical syndrome of HSP. It may appear simultaneously with damage to the skin and joints, or may precede skin and joint changes, and then early diagnosis of HSP is difficult. The clinical picture of abdominal syndrome is different. Some patients complain of moderate abdominal pain, which is not accompanied by dyspeptic disorders, does not cause much suffering and resolves on its own or in the first 2-3 days from the start of treatment. In others, abdominalgia is paroxysmal in nature, occurs suddenly like intestinal colic, and does not have a clear localization. Painful attacks can be repeated many times during the day and last up to several days. Children complain of nausea, vomiting, unstable stools, and sometimes fever. In rare cases, against the background of this clinical picture, episodes of intestinal and gastric bleeding are observed. With abdominal syndrome, complications are possible in the form of intussusception, intestinal obstruction and intestinal perforation with the development of peritonitis, requiring surgical intervention. Currently, with timely use of complex therapy, these complications are rare. However, children with abdominal syndrome should be observed simultaneously by a pediatrician and a surgeon in order not to miss life-threatening complications.
Kidney damage in HSP is observed less frequently than other clinical manifestations of the disease, however, it is the involvement of the kidneys in the pathological process that determines the prognosis of the disease and casts doubt on the possibility of a complete recovery of the child. Renal syndrome is more often detected in those children in whom HSP debuted polysyndromously and in the initial period of the disease abdominal syndrome of varying severity was noted. It develops at the onset of the disease or occurs at subsequent stages of relapse. Kidney damage can be different - from transient microerythrocyturia and trace proteinuria, which quickly disappear during therapy, to a pronounced picture of glomerulonephritis (Schönlein-Henoch nephritis). When the latter develops, most children are diagnosed with a hematuric form of glomerulonephritis, less often - a nephrotic variant of glomerulonephritis with hematuria. The most difficult prognosis is the mixed form of nephritis, since it is it that leads to the early development of chronic renal failure. When observing patients, it seems that in some cases long-term, persistent hematuria is caused not only by changes inherent in HSP, but also by the background against which it develops - dysplasia of the renal tissue, anomaly of the renal vessels. In this regard, in some patients, especially in children with high blood pressure, in terms of examination in order to clarify the cause of hematuria, it is advisable to use a morphological study of kidney tissue and Dopplerography of intrarenal vessels.
Significantly less often with BSH, damage to other organs is detected. Pulmonary syndrome can occur against the background of the manifestation of clinical symptoms of the disease in the form of a cough with a small amount of sputum and streaks of blood, sometimes shortness of breath. On auscultation, moist rales and crepitus may be heard. Cardiac changes in HSP are rare. Hemorrhagic pericarditis and endocardial hemorrhages have been described. As a rule, these changes are reversible. More often in children, against the background of moderate and severe disease, a systolic murmur of a functional nature appears. Damage to the central nervous system is caused by vasculitis of the vessels of the brain, meninges and usually appears at the height of skin changes. Children complain of headaches, dizziness, and irritability. Meningeal symptoms are rare. In some cases, boys with HSP experience damage to the testicles - swelling, pain; often bilateral.
Changes in laboratory parameters are nonspecific. In the acute period of the disease, neutrophilic leukocytosis, increased ESR, dysproteinemia with increased levels of alpha-2-globulins, increased nonspecific indicators characterizing inflammation - DPA, seromucoid, C-reactive protein, titers of antistreptolysin O and antihyaluronidase are possible. Immunological changes in the form of increased levels of immunoglobulin A, increased circulating immune complexes and cryoglobulins, decreased levels of immunoglobulin G, complement activity, and in rare cases, positive antinuclear factor, latex test can be detected in patients with chronic recurrent forms of the disease and Henoch-Schönlein nephritis . Laboratory manifestations of hypercoagulation (increased levels of fibrinogen, soluble fibrin monomer complexes, induced platelet aggregation, inhibition of fibrinolysis) are most pronounced in severe cases of the disease.
The diagnosis of HSP is not difficult in cases where the disease begins with a typical skin syndrome. Difficulties arise when the disease debuts with articular, abdominal or renal syndromes.
At the onset of the disease, no matter how it begins - with a monosyndrome or polysyndrome, it is difficult to decide what course it will take. The course of the disease can be acute, protracted or chronic recurrent. In the acute course, a reverse development of all symptoms is observed within 2 months. In case of protracted symptoms, individual symptoms persist for up to 6 months, taking an undulating course. In a chronic relapsing course, the disease continues indefinitely, sometimes for years, relapsing with one, more often skin syndrome or several. A situation is possible when only Schönlein-Henoch jade is preserved.
A feature of the modern course of HSP is the more frequent involvement of the kidneys in the pathological process. Nevertheless, with the use of pathogenetic therapy in recent decades, undoubted success in treatment has been achieved: the overall duration of the disease has decreased, the percentage of extremely severe fulminant forms, the number of complications and deaths have decreased.
Goals of therapy for HSP: 1) elimination of clinical manifestations; 2) prevention of life-threatening conditions (intussusception, mesenteric thrombosis, intestinal necrosis, renal failure); 3) normalization of laboratory parameters; 4) restoration of age-appropriate quality of life.
The nature of therapy for HSP varies depending on the phase of the disease - debut, relapse, period of remission; clinical form - simple (skin), mixed, with kidney damage; degree of severity of clinical manifestations - mild (satisfactory state of health, mild rashes, arthralgia is possible), moderate (multiple rashes, arthralgia or arthritis, periodic abdominal pain, microhematuria, trace proteinuria), severe (confluent rashes, elements of necrosis, recurrent angioedema, persistent abdominal pain, gastrointestinal bleeding, gross hematuria, nephrotic syndrome, acute renal failure); nature of the course of the disease - acute (up to 2 months), prolonged (up to 6 months), chronic (recurrent or development of Schönlein-Henoch nephritis).
Treatment of the onset or recurrence of HSP can be divided into pathogenetic, with the use of intensive therapy in severe cases, and symptomatic. Particular attention is paid to the sanitation of concomitant infections, which can be a resolving or supporting factor for a recurrent course.
PATHOGENETIC THERAPY, in principle, involves influencing the basic mechanisms of pathogenesis by: 1) eliminating circulating immune complexes (plasmapheresis, infusion therapy) 2) suppressing immune complex inflammation (glucocorticosteroids, non-steroidal anti-inflammatory drugs, cytostatics); 3) correction of hemostasis (direct and indirect anticoagulants, antiplatelet agents, fibrinolysis activators). However, in practice, treatment is aimed primarily at eliminating those clinical manifestations that occur in a particular patient. The nature of therapy is individual, but the common thing is the use of anticoagulants and/or antiplatelet agents that affect the final stage of pathogenesis.
Antiplatelet agents are used for all forms of the disease. Curantil (dipyridamole, persantine) 5-8 mg/kg per day in 4 divided doses; trental (pentoxifylline, agapurine) 5-10 mg/kg per day in 3 doses; ticlopidine (ticlid) 250 mg 2 times a day. In severe cases, two drugs are prescribed simultaneously to enhance the antiaggregation effect. The duration of treatment depends on the clinical form and severity: 2-3 months - for mild cases; 4-6 months - for moderate cases; up to 12 months - with severe recurrent course and Schönlein-Henoch nephritis; in case of chronic course, treatment is carried out with repeated courses for 3-6 months.
Anticoagulants are indicated for moderate and severe cases at the onset or in the active period with subsequent exacerbations; in mild cases, monotherapy with antiplatelet agents is usually sufficient. Heparin or its low molecular weight analogue fraxiparin is used. The dose of anticoagulants is selected individually, focusing on the positive clinical dynamics of symptoms (stabilization of skin rashes, relief of abdominal pain, reduction in the degree of hematuria), as well as laboratory parameters (extension of blood clotting time or activated recalcification time by 2-3 times compared with the initial one, conversion of positive paracoagulation tests to negative). In the absence of proper clinical and laboratory effect, the dose is increased by 50-100 units/kg/day. Our experience shows that in moderate cases there is no need to increase the dose above 300-400 IU/kg/day, and in severe cases in 40% of cases the effect is achieved at 500-800 IU/kg/day. In the latter group of patients, the weak anticoagulant effect of the drug is due to the high content of acute phase proteins that bind heparin and depletion of the level of antithrombin III, and therefore additional administration of fresh frozen plasma is indicated at a dose of 10-20 ml/kg per day as a donor of antithrombin III. Use subcutaneous injection of heparin into the abdominal tissue 3-4 times a day (fraxiparine - 2 times) or intravenously. For moderate HSP, the course of treatment usually lasts up to 25-30 days; in case of severe to persistent relief of clinical syndromes, 45-60 days of heparin therapy are necessary; with developed Schönlein-Henoch nephritis, it lengthens. The withdrawal of drugs is carried out gradually at 100 units/kg/day every 1-3 days.
Fibrinolysis activators - nicotinic acid and its derivatives (xanthinol nicotinate, theonicol, complamin) - are vasoactive drugs that promote the release of vascular plasminogen activators into the bloodstream and are used to inhibit fibrinolysis. The dose is selected taking into account individual sensitivity, usually it is 0.3-0.6 g per day.
Glucocorticosteroids are effective in severe cases of the disease with wave-like recurrence of skin purpura with a pronounced exudative component, necrosis, and persistent articular syndrome; long-term intractable abdominal syndrome; renal changes with gross hematuria or high degree of erythrocyturia; nephrotic syndrome, which is always accompanied by high inflammatory activity in laboratory tests. Treatment with glucocorticosteroids must be carried out against the background of anticoagulant-antiplatelet therapy. For moderate and mild cases, their use is not justified. In simple and mixed forms without kidney damage, the oral dose of prednisolone is 0.7-1.5 mg/kg per day and is used in a short course of 7-20 days. With the development of Schönlein-Henoch nephritis, 2 mg/kg per day is prescribed for 1-2 months, followed by a decrease of 2.5-5.0 mg once every 5-7 days until complete withdrawal.
Cytostatics are appropriate for severe forms of Schönlein-Henoch nephritis (nephrotic syndrome with hematuria, mixed form, rapidly progressive nephritis) or hematuric form of nephritis with relapses of gross hematuria in the absence of positive dynamics of treatment with glucocorticosteroids, as well as in the presence of severe skin syndrome with necrosis against the background of high immunological activity. For oral administration, use azathioprine 2 mg/kg/day, cyclophosphamide 2 mg/kg/day for up to 4-6 months. Treatment is carried out under the control of the composition of peripheral blood: if leukopenia develops, cytostatics are canceled; against the background of intercurrent illnesses, the dose is reduced by 2 times until recovery.
4-aminoquinoline derivatives: prescribed when the activity of severe forms of the disease subsides against the background of reducing the dose of prednisolone or after its discontinuation, as well as for recurrent skin purpura. Drugs in this group (plaquenil, delagil) have a weak immunosuppressive, anti-inflammatory, and antiplatelet effect. The daily dose is 4-6 mg/kg, duration of use is 6 months. Treatment is also carried out under the supervision of a general blood test (possibility of leukopenia) and observation by an ophthalmologist (possibility of decreased visual acuity, pigment deposition in the cornea).
INTENSIVE THERAPY. By the nature of the means and methods of treatment used, it is an integral part of pathogenetic therapy and is used in patients with the most severe course of the disease: with fulminant development of symptoms, with the development of critical conditions (gastrointestinal bleeding, prolonged gross hematuria, acute renal failure).
Intravenous permanent heparinization: the use of constant round-the-clock intravenous administration of heparin in an individually selected dose (400-800 IU/kg/day) for 7-15 days in patients with severe mixed forms contributes to a more rapid relief of the main clinical manifestations compared to subcutaneous administration of the drug 4 once a day. After the end of permanent heparinization, they switch to subcutaneous administration of heparin.
Transfusion therapy: is carried out in children with severe HSP for 5-15 days during the acute period of the disease, when clinical manifestations, hypercoagulation, hemodynamic disorders are most pronounced, simultaneously with other pathogenetic therapy. Transfusion therapy is aimed at improving peripheral microcirculation, rheological properties of blood, and relieving intoxication. Transfusion therapy includes: low-molecular plasma replacement solutions (reopolyglucin, reogluman, reomacrodex) at a rate of 10-20 ml/kg/day; glucose-novocaine mixture (5% glucose solution and 0.25% novocaine solution in a ratio of 2:1 or 3:1) in the amount of 10 ml per 1 kg of body weight, but not more than 100 ml; antispasmodics - aminophylline (5 mg/kg/day), no-spa (2 ml of 2% solution) in 150-250 ml of isotonic sodium chloride solution; inhibitors of proteolytic enzymes (contrical 20,000 - 40,000 IU/kg/day, trasylol 50,000 - 100,000 IU/day). The drugs are administered dropwise at a rate of 10-15 drops per minute.
Plasmapheresis is aimed at removing toxins, bacteria, inflammatory substances, antibodies, immune complexes, cryoglobulins from the circulation and is indicated for severe HSP, continuous or wave-like recurrence of symptoms. Plasmapheresis helps normalize the rheological properties of blood, relieves vascular spasm, improves microcirculation, increases the functional activity of immunocompetent cells, and increases the sensitivity of patients to drugs. The volume of exfused plasma is 10-30 ml per 1 kg of the child’s body weight (for a course of treatment consisting of 3-8 sessions of plasmapheresis, 2 to 5 volumes of circulating plasma are removed). The first 3-4 sessions are carried out daily, and the subsequent ones - once every 3 days. Exfusion rate is 50 ml per minute. To prevent thrombosis, heparin is used at a rate of 100-300 IU/kg. Low molecular weight dextrans, solutions of albumin, glucose, and saline are used as replacement solutions.
The use of “pure” plasmapheresis is ineffective in children with chronic recurrent HSP, since relapses recurred in 100% of cases after 1-3 months. Plasmapheresis also does not affect the prevention and course of the renal process. Significantly better results, especially in patients with Henoch-Schönlein nephritis, were obtained when plasmapheresis was performed synchronously with pulse therapy with immunosuppressants.
Synchronous therapy: justified in patients with severe Schönlein-Henoch nephritis or in the case of long-term and persistent recurrent course of other symptoms of HSP in the presence of immunological activity. Plasmapheresis is carried out in combination with intravenous administration of metipred at a rate of 15-20 mg/kg and/or cyclophosphamide at a rate of 5-12 mg/kg daily for 3 days, then 2 times a week for 2-4 weeks.
Symptomatic therapy. In the acute period, to improve blood circulation and microcirculation, bed rest is necessary until the hemorrhagic rash and pain symptoms disappear, followed by its gradual expansion. Violation of bed rest often leads to increased or repeated rashes.
A hypoallergenic diet with the exclusion of obligate allergens is indicated for all patients during the acute period. For severe abdominal pain, dyspeptic disorders, and intestinal bleeding, table No. 1 (anti-ulcer) is prescribed. For the nephrotic variant of glomerulonephritis, a salt-free diet with protein restriction is used.
Antihistamines are effective in children with a history of food, drug or household allergies, manifestations of exudative-catarrhal diathesis, allergic diseases (polynosis, Quincke's edema, obstructive bronchitis, bronchial asthma). Use tavegil, suprastin, diazolin, fenkarol and other drugs in age-specific dosages for 7-10 days.
Enterosorbents are necessary for patients with a burdened allergic history, in the presence of abdominal syndrome with dyspeptic manifestations, in cases where food agents were a provoking factor of the disease. Enterosorbents bind toxins and biologically active substances in the intestinal lumen, thereby preventing their penetration into the systemic bloodstream. For this purpose, polyphepan, smecta, enterosorb, and activated carbon are prescribed 3-4 times a day for 5-10 days.
Indications for the use of non-steroidal anti-inflammatory drugs may be high laboratory inflammatory activity (leukocytosis, ESR, fibrinogen, seromucoid), recurrent skin purpura, persistent articular syndrome in the absence of the need to prescribe glucocorticosteroids. The duration of treatment is 4-8 weeks. Ortofen (Voltaren) is used in a daily dose of 1-2 mg/kg, indomethacin 3-4 mg/kg, ibuprofen (Brufen) 15-20 mg/kg in 3 doses after meals. Careful use of these drugs is necessary in case of kidney damage due to the likelihood of increased hematuria.
Membrane stabilizers are prescribed in repeated courses for Schönlein-Henoch nephritis or recurrent skin syndrome. Drugs in this group help reduce the permeability of the vascular wall, improve trophic processes, and have an immunomodulatory effect. The most widely used are retinol, tocopherol (vitamin E), rutin, dimephosphone for 1 month.
TREATMENT OF RELATED INFECTIONS. Acute and chronic bacterial and viral infections, according to most clinicians, occupy a leading place among the factors immediately preceding the development of HSP and provoking subsequent relapses. Treatment of intercurrent infections is carried out simultaneously with pathogenetic and symptomatic therapy. Often, timely treatment of concomitant infectious manifestations determines the outcome of HSP.
Antibiotics are indicated only in the presence of acute or exacerbation of chronic foci of infection. Most often, HSP is accompanied by bacterial infections of the upper respiratory tract, which, taking into account the sensitivity of the microflora, determines the use of penicillin antibiotics (ampicillin, ampiox, phenoxymethylpenicillin) and macrolides (erythromycin, sumamed, rulid). In most cases, one course of antibiotic therapy is sufficient; if necessary, treatment can be continued for up to 3-4 weeks with sequential changes in drugs.
Since in almost all patients intercurrent infections provoke exacerbations of HSP or Henoch-Schönlein nephritis, the use of immunomodulators in a group of frequently ill children helps to reduce morbidity and, as a result, reduce exacerbations of the underlying disease. Along with traditionally used drugs - dibazole (1-2 mg/kg in 2 doses, for 4-5 weeks), levamisole (2 mg/kg per day for 3 days with breaks between courses of 5 days; 3-4 courses in total ), currently using immunal (10-20 drops 3 times a day - 8 weeks), tonsilgon (15 drops 3 times a day - 6 weeks).
In recent years, in a small group of children, simultaneously with pathogenetic therapy, we have used intravenous immunoglobulin in a course dose of 200-400 mg/kg IgG; in 4 children - repeated courses. These were patients with continuous recurrence of HSP and with Schönlein-Henoch nephritis, occurring with frequent relapses of gross hematuria or nephrotic syndrome against the background of exacerbation of chronic persistent viral infections (herpetic, cytomegalovirus) or acute viral diseases. The introduction of immunoglobulin made it possible to achieve complete clinical and laboratory remission or a significant reduction in the number of skin rashes, to prevent the relapse of gross hematuria or nephrotic syndrome against the background of ARVI, as was constantly observed in patients before the use of intravenous immunoglobulin. Therefore, we believe that this type of treatment, successfully used in patients with other systemic diseases, can be recommended for use in HSP if there are appropriate indications.
With timely complex therapy, most patients recover. Difficulties arise in the treatment of persistently recurrent forms. In these cases, it is important to search for and influence possible factors that support the pathological process. These are tonsillectomy, adenotomy, conservative treatment of chronic diseases of the nasopharynx, treatment of chronic periodontitis, recurrent pyoderma, recurrent herpetic infection, intestinal dysbiosis, viral hepatitis, nonspecific anti-tuberculosis chemoprophylaxis, deworming, immunomodulatory therapy, etc.
During the period of clinical and laboratory remission, all children are subject to regular dispensary observation by a pediatrician once a quarter for at least 5 years from the moment of its onset; with the development of Schönlein-Henoch nephritis by a nephrologist. For any clinical form of the disease, it is necessary to monitor urine tests once a month and against the background of intercurrent diseases lasting up to 5 years; for Henoch-Schönlein nephritis, blood pressure control is carried out once a month. Every six months, an examination should be carried out by a dentist, otolaryngologist and other specialists according to indications in order to identify and timely sanitize foci of infection. It is recommended to avoid preventive vaccinations for 3-5 years (except for the Mantoux reaction). A home regimen is indicated for 6-12 months. Sports activities are contraindicated; Physical education classes are given in a special group for acute cases up to 2 years, for chronic cases - constantly. A diet is prescribed excluding obligate allergens for a year.
The outcome of HSP in children is generally favorable. Recovery after the onset is observed in more than half of the patients. A long-term recurrent course of the disease is possible, with the frequency of relapses ranging from once over several years to monthly. However, over time, as a rule, the disease acquires a monosyndromic character: only cutaneous purpura (less often with articular syndrome) or chronic Schönlein-Henoch nephritis develops, most often of the hematuric form. At the same time, kidney function remains intact for a long time. The outcome of chronic renal failure is observed extremely rarely, with a mixed form of glomerulonephritis or a rapidly progressing variant.
Professor Galina LYSKINA. Galina ZINOVIEVA, associate professor. Elena KIKINSKAYA, Candidate of Medical Sciences. Moscow Medical Academy named after. I.M. Sechenov.
Symptoms of vasculitis
Manifestations of vasculitis depend on the characteristics of the course of the disease.
With periarteritis nodosa, muscle pain, sharp abdominal pain, vomiting, high fever, and weight loss may occur. Wegener's granulomatosis causes purulent and bloody nasal discharge, the nasal mucosa becomes covered with ulcers, and coughing up blood may occur. Giant cell arteritis is accompanied by weakness, fever, headaches, and weight loss. Ulcers on the genitals, stomatitis, and inflammation of the eyes (Behcet's syndrome) may occur.
With vasculitis affecting the skin, a rash occurs on the legs and other parts of the body. When the nervous system is damaged, sensitivity is impaired.
Treatment of the disease is complicated by diabetes mellitus, hypertension and venous insufficiency.
1.General information
Reiter's vasculitis (in other spellings "Ruiter's vasculitis") refers to a special group of allergic disorders in which the immune-inflammatory process primarily affects venules, arterioles and capillaries, that is, medium and small blood vessels. Reiter's vasculitis differs from similar vascular inflammations in a longer prodromal period with nonspecific symptoms, the true cause of which is identified, as a rule, retrospectively.
Allergic arteriolitis is rare (there are no exact epidemiological statistics), mainly in young women, although this trend is not absolute (for example, according to some data, about 10% of cases are children). Regarding the etiopathogenesis of vascular allergens, including Reiter's allergic vasculitis, various hypotheses are still being expressed, scientific discussions are ongoing and multidisciplinary research is being carried out.
A must read! Help with treatment and hospitalization!
Vasculitis - treatment
Treatment of systemic vasculitis (SPb) is primarily accompanied by immunosuppressive (suppressive) therapy, and medications are also used to improve blood flow in the vessels. In cases of severe disease, plasmapheresis is used (a method of purifying the blood of large particles such as immune complexes). Often, treatment of vasculitis requires consultation with a nephrologist, ophthalmologist, laryngologist, neurologist, dermatologist and surgeon.
In our clinic, you can be examined by a rheumatologist, receive qualified advice from doctors in other fields, and diagnose diseases using modern equipment.
How to treat?
In cases of a mild form of the disease, treatment of hemorrhagic vasculitis can be done without compulsory hospitalization of the patient, but in any case it will require bed rest. During the acute period, a hospital stay under the constant supervision of doctors is necessary. An acute disease is usually cured within about 2 months; if the disease is protracted, the duration of treatment can increase to six months.
Therapy includes medication as indicated. In severe cases of the disease, glucocorticosteroids may be prescribed, as well as plasmapheresis or transfusion therapy for children. In the presence of allergic manifestations, antihistamines are prescribed. The diet for hemorrhagic vasculitis is aimed at excluding potentially allergenic foods that can worsen the patient’s condition - citrus fruits, strawberries, chocolate, coffee, eggs, etc. For severe renal and abdominal syndrome, special diets are prescribed.
Cost of treatment for vasculitis:
| Services list | Price in rubles | |
| Saint Petersburg | Vsevolozhsk | |
| Initial appointment with a 1st stage rheumatologist | 1850 | — |
| Repeated appointment with a 1st stage rheumatologist | 1650 | — |
| Initial appointment with a rheumatologist, leading specialist | 2500 | 2000 |
| Repeated appointment with a rheumatologist, leading specialist | 2300 | 1800 |
| MANIPULATION | ||
| Capillaroscopy | 1500 | — |
Prevention
Unfortunately, it is impossible to protect yourself one hundred percent from the appearance of vasculitis. Preventive measures include maintaining immunity, a healthy lifestyle, and paying attention to health.
If a person has already been diagnosed with vasculitis, we must not forget that the disease can return, so you need to carefully monitor your well-being.
Medical specialists in St. Petersburg remind: the sooner treatment is started, the less negative impact the disease will have on the body. If symptoms appear, consult a doctor immediately. Registration by phone is carried out around the clock.
Diagnostics
Since the disease can occur individually in each patient, the variety of clinical symptoms requires the collection of a detailed history, laboratory tests, and sometimes histological analyzes of the elements of the rash and skin are necessary. It is important to notice in time an increase in immunoglobulin E (IgE) due to the formation of immune complexes on the vascular wall.
After scratching the allergic rash and bursting the blisters, accompanying pathogenic bacteria may join. To determine their type, the method of inoculation on a Petri dish is used, and the level of sensitivity to various antibiotics is also established.
What it is?
Allergic vasculitis is a disease that affects the walls of blood vessels due to an allergic reaction. Allergic vasculitis (hereinafter referred to as AL) combines several independent diseases, which, in fact, are its forms.
The disease can affect people of any age and gender, however, the signs of allergic vasculitis in children and adults may differ.
- Thus, in childhood, the spots are hemorrhagic in nature and have blurry boundaries and a bright red tint. In some places the spots may merge.
- In adults, the spots, on the contrary, are clear.
Statistics show that different forms of the disease are more pronounced in certain groups. Thus, hemorrhagic vasculitis often affects children under 14 years of age.
Classification
Today there is no unified classification of skin vasculitis. These include several dozen dermatoses that have clinical similarities. The simplest division is related to the source of the disease.
- Primary vasculitis is an independent disease caused by the direct action of an allergen: medicine, intoxication, food, hypothermia or, conversely, prolonged exposure to the sun. For example, toxic-allergic vasculitis, which manifests itself as a reaction to the action of a substance. Treatment in such cases comes down to stopping contact with the allergen.
- Secondary - occurs as a result of some diseases, for example, rheumatic.
The following type of classification is based on the degree and depth of vascular damage in tissues and organs:
| Dermal form, or vasculitis of the skin | Affects mainly small vessels located in the upper layers of the dermis. The mildest form, which causes virtually no complications with timely treatment. |
| Dermo-hypodermal form | Damage to the vessels of the dermis, reaching the deep layers. Sometimes small vessels of soft tissues are affected. |
| Hypodermal form | It is characterized by damage to large vessels - veins and arteries. One of the most dangerous variants of the disease, requiring hospital treatment. |
When it comes to skin lesions, the following types are distinguished:
- rheumatic (systemic) – directly related to lupus and arthritis;
- hemorrhagic (synonyms used in the medical field - anaphylactic purpura, Henoch-Schönlein disease, sometimes called capillary toxicosis);
- polymorphic vasculitis (doctors call it Ruiter's allergic arteriolitis);
- leukocytoclastic - breakdown of leukocyte nuclei, detected by histological examination;
- urticarial vasculitis (in medical circles known as necrotizing urticarial vasculitis);
- papulo-necrotic vasculitis (a disease similar to Werther-Dümling syndrome);
- giant cell – leads to severe damage to large arteries;
- granulomatous - granules form inside the vessels, slowing down or stopping the flow of blood;
- vasculitis nodosum (erythema nodosum, rarely caused by medications);
- nodular-ulcerative vasculitis (three times the name is chronic erythema nodosum).
Diagnosis of vasculitis is based not so much on recording symptoms, but on assessing the rate of change. A histological examination of the affected area and consultation with the necessary specialists are mandatory.