Heart failure is a disease that is accompanied by insufficient contractility of the heart, which does not meet the metabolic needs of the body
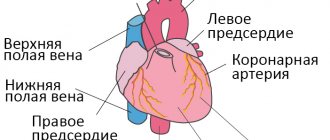
A healthy heart easily pumps blood from the left ventricle through the body to the organs. This allows you to provide them with oxygen and essential nutrients. After fulfilling its saturation function, the blood returns to the heart, but to the right side. From there, the blood is sent to the lungs, where it is saturated with oxygen and again begins its path through the left ventricle.
In other words, the disease is a weakening of the very pumping function of the heart. The lesion occurs either on the right side of the heart or on the left (right and left ventricular heart failure, respectively). Progressive disease may involve damage to both sides of the heart. In addition, deficiency can be chronic or acute.
Causes
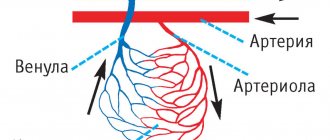
One of the main causes of chronic disease is coronary artery disease - coronary heart disease, angina pectoris.
Coronary heart disease is often caused by narrowing of the coronary vessels. They are vessels that supply the heart with oxygen and nutrients. Arterial stenosis interferes with the functioning of the heart. As a result, the most dangerous complication may occur - myocardial infarction, as a result of which heart failure often develops.
Hypertension causes heart failure in about 20 percent of patients. In fact, it is the second most common cause of the disease. High blood pressure puts increased stress on the heart, which leads to a gradual change in its shape, left ventricular hypertrophy.
Also, the disease can be caused by unstable functioning of the heart valves - stenosis or insufficiency.
In addition, there are hereditary heart diseases, alcoholism, drug addiction, overactive thyroid gland, etc. All this can cause the development of the disease.
Clinical forms
- Congestive left ventricular failure is characteristic of mitral disease and severe forms of coronary artery disease - especially in patients with arterial hypertension. Increased pressure in the pulmonary veins helps fill the left ventricle and maintain sufficient cardiac output. At the same time, congestive changes in the lungs disrupt the function of external respiration and are the main factor aggravating the patient’s condition with this form of heart failure. Manifestations: shortness of breath, orthopnea, auscultatory signs of pulmonary congestion (dry rales below the level of the shoulder blades, migrating moist rales) and radiological, cardiac asthma and pulmonary edema, secondary pulmonary hypertension, tachycardia.
- Left ventricular failure is characteristic of aortic disease (see), coronary artery disease, and arterial hypertension. Manifestations: cerebrovascular insufficiency (dizziness, darkening of the eyes, fainting), coronary insufficiency, sphygmographic and echocardiographic signs of low output. In severe cases, Cheyne-Stokes breathing, alternating pulse (rarely), presystolic gallop rhythm (pathological IV tone), and clinical manifestations of congestive left ventricular failure are possible. In the terminal stage, right ventricular failure may occur.
- Congestive right ventricular failure is characteristic of mitral and tricuspid disease, constrictive pericarditis. Usually associated with congestive left ventricular failure. Manifestations: swelling of the neck veins, high venous pressure, acrocyanosis, enlarged liver, subicterus, edema - cavitary and peripheral.
- Right ventricular ejection failure is characteristic of pulmonary artery stenosis and pulmonary hypertension. It is diagnosed mainly radiographically (depleted peripheral pulmonary vascular pattern). Other signs of this form may be detected: shortness of breath at a strictly defined threshold level of physical activity, right ventricular hypertrophy - palpation, then ECG signs of the “pressure load” type (high I wave and decreased T wave in the right precordial leads). In especially severe cases, gray coloration of the skin.
- Dystrophic form. As a rule, end-stage right ventricular failure. Options: a) cachectic; b) edematous-dystrophic with dystrophic changes in the skin (thinning, shine, smoothness of the pattern, flabbiness), edema - widespread or limited mobile, hypoalbuminemia, in the most severe cases - anasarca; c) uncorrectable salt depletion.
In some cases, changes in the heart itself (cardiomegaly, atriomegaly, atrial fibrillation) come to the fore, which allows us to speak of a “central” form of heart failure. As special forms with specific mechanisms of circulatory disorders and manifestations, HF is considered in “blue” congenital defects with insufficient blood flow in the pulmonary circle and unreduced or excessive in the large circle, with cor pulmonale, thyrotoxicosis, anemia, arteriovenous anastomosis, cirrhosis of the liver, as well as arrhythmogenic SN.
Patients may develop “passive adaptation” from childhood (low body weight and height, poor physical development, sharply reduced physical activity, infantilism). The listed forms of CH occur in various combinations; often it is possible to isolate only the leading form.
Types and symptoms
Each individual type of heart failure has its own symptoms, which, in turn, may vary in intensity. However, the main symptom is still difficulty breathing during exercise or at rest. Also, warning signals include increased sweating, tightness in the chest, swelling of the lower extremities, and an increase in the size of the liver.
Left ventricular heart failure
The left side of the heart (left ventricle) is responsible for pumping oxygenated and nutrient-rich blood to the organs. With this type of disease, the pumping function is reduced, which leads to insufficient oxygen saturation of the organs. Instead of stable functioning of the body, blood stagnation occurs, which leads to shortness of breath and pulmonary edema, difficulty breathing, weakness and dizziness.
Left ventricular heart failure can manifest itself either acutely or develop over years and become chronic.
Right ventricular heart failure
The right side of the heart is responsible for returning already low-oxygen blood back to the lungs to saturate them. Right ventricular heart failure means unstable functioning of the right ventricle. This leads to swelling of the lower extremities, an increase in the size of the liver and frequent urination.
The cause of right ventricular heart failure can be an acute or chronic increase in circulatory resistance. It, in turn, is caused by pulmonary embolism, asthma, lung disease, tobacco use, etc.
Systolic and diastolic heart failure
Systolic heart failure develops against the background of unstable functioning of the heart cells or disturbances in its pumping function. At the same time, the organs are not adequately saturated with oxygen and nutrients.
Diastolic heart failure is accompanied by a decrease in the elasticity of the ventricles of the heart. This leads to the fact that it does not relax and cannot be filled in the necessary way. One of the common causes of this type of disease is often high blood pressure.
Chronic and acute heart failure
Chronic deficiency is characterized by long-term development. The body compensates for the symptoms of the disease over time.
Acute failure occurs suddenly, within minutes or hours after a heart attack. Symptoms include severe difficulty breathing, chest pain, unstable heart rate, cold sweat and paleness.
Acute heart failure
DEFINITION.
Acute heart failure, which occurs as a consequence of impaired myocardial contractility, a decrease in systolic and cardiac output, is manifested by several extremely severe clinical syndromes: cardiogenic shock, pulmonary edema, acute decompensated cor pulmonale, etc.
ETIOLOGY AND PATHOGENESIS.
The contractility of the myocardium decreases either as a result of its overload with an increase in the hemodynamic load on the left or right heart, or due to a decrease in the functioning mass of the myocardium or a decrease in the compliance of the chamber walls. Acute heart failure develops when:
- impairment of diastolic and/or systolic myocardial function due to the development of infarction (the most common cause), inflammatory or dystrophic diseases of the myocardium, as well as tachycardia, tachy- and bradyarrhythmias;
- sudden occurrence of myocardial overload in the corresponding part of the heart due to a rapid significant increase in resistance on the outflow tract (in the aorta - hypertensive crisis; in the pulmonary artery - massive thromboembolism of the branches of the pulmonary artery, a prolonged attack of bronchial asthma with the development of acute pulmonary emphysema, etc.) or volume load (increased mass of circulating blood, for example, with massive fluid infusions - a variant of the hyperkinetic type of hemodynamics);
- acute disturbances of intracardiac hemodynamics due to rupture of the interventricular septum or the development of aortic, mitral or tricuspid insufficiency (septal infarction, infarction or avulsion of the papillary muscle, bacterial endocarditis with perforation of the valve leaflets, rupture of the chordae, trauma);
- increased load (physical or psycho-emotional stress, increased inflow in a horizontal position, etc.) on the decompensated myocardium in patients with more or less severe chronic congestive heart failure due to congenital or acquired heart defects, post-infarction cardiosclerosis, hypertrophic or dilated cardiomyopathy.
A decrease in myocardial contractile function leads to a number of compensatory changes in hemodynamics:
- to maintain cardiac output with a decrease in stroke volume, heart rate increases, which is accompanied by a shortening of diastole, a decrease in diastolic filling and leads to an even greater drop in stroke volume;
With a decrease in ventricular contractility, the pressure in the atria and veins increases, resulting in the formation of stagnation in that part of the bloodstream that precedes the chamber of the decompensated myocardium. Increased venous pressure contributes to an increase in diastolic filling of the corresponding chamber and, according to the Frank-Starling law, shock ejection, but an increase in preload leads to an increase in myocardial energy consumption and the progression of decompensation. Acute congestive left ventricular failure is manifested by an increase in pressure in the pulmonary artery system (which is aggravated by the Kitaev reflex - narrowing of the pulmonary arterioles in response to increased pressure in the left atrium), deterioration of external respiration and blood oxygenation, and, when the hydrostatic pressure in the pulmonary capillaries exceeds the oncotic and osmotic pressure , leads first to interstitial and then to alveolar pulmonary edema;
When cardiac output decreases, maintaining a sufficient level of blood pressure is achieved by increasing peripheral resistance. However, this leads to an increase in afterload and a deterioration in tissue perfusion (including the perfusion of vital organs - heart, kidneys, brain), which is especially pronounced when compensatory mechanisms are insufficient and blood pressure decreases.
An increase in peripheral resistance, shunting and sequestration of blood and a slowdown in tissue blood flow, which are primarily characteristic of shock, contribute to the exudation of the liquid part of the blood into the tissue, and therefore hypovolemia, hemoconcentration develop, deterioration of the rheological properties of the blood and conditions are created for the development of thrombotic complications.
With various clinical variants, certain variants of hemodynamic disturbances may come to the fore.
CLINICAL PICTURE AND CLASSIFICATION.
Depending on the type of hemodynamics, the affected chamber of the heart and some features of pathogenesis, the following clinical variants of acute heart failure are distinguished:
| A) with a stagnant type of hemodynamics: - right ventricular (venous congestion in the systemic circulation), - left ventricular (cardiac asthma, pulmonary edema); | B) with hypokinetic 1 type of hemodynamics (small output syndrome - cardiogenic shock): - arrhythmic shock, - reflex shock, - true shock. 1The clinical picture of cardiogenic shock can develop with hypovolemia preceding a heart attack (against the background of active diuretic therapy, profuse diarrhea, etc.) |
Since myocardial infarction is one of the most common causes of acute heart failure, its classification in this disease is of interest (Table 8).
Table 8 Classification of acute heart failure during myocardial infarction (based on Killip T. & Kimball J., 1967)
| Class | Clinical signs of deficiency | Frequency % | Mortality % | Principles of pharmacological treatment |
| I | There are no wheezing or third sounds in the lungs | 33 | 8 | Not required |
| II | Wheezing in the lungs no more than 50% of the surface or the third tone | 38 | 30 | Reduce preload using primarily diuretics |
| III | Crackles in the lungs over more than 50% of the surface (often a picture of pulmonary edema) | 10 | 44 | Reducing preload with diuretics and nitrates, and if ineffective, increasing cardiac output with non-glycoside inotropic agents |
| IV | Cardiogenic shock | 19 | 80-100 | Depending on the clinical variant, severity and type of hemodynamics, different combinations of infusion and inotropic therapy |
Acute congestive right ventricular failure
manifested by venous stagnation in the systemic circulation with increased systemic venous pressure, swelling of the veins (best noticeable in the neck) and liver, and tachycardia; swelling may appear in the lower parts of the body (in a horizontal position - on the back or side). Clinically, it differs from chronic right ventricular failure by intense pain in the liver area, aggravated by palpation. Signs of dilatation and overload of the right heart are determined (expansion of the borders of the heart to the right, systolic murmur over the xiphoid process and protodiastolic gallop rhythm, emphasis of the second tone on the pulmonary artery and corresponding ECG changes). A decrease in left ventricular filling pressure due to right ventricular failure can lead to a drop in the minute volume of the left ventricle and the development of arterial hypotension up to the picture of cardiogenic shock (see).
With pericardial tamponade, constrictive pericarditis, the pattern of congestion in a large circle is not associated with contractile insufficiency of myocardial contractile function, and treatment is aimed at restoring diastolic filling of the heart.
Biventricular failure, when congestive right ventricular failure accompanies left ventricular failure, is not discussed in this section, since its treatment differs little from the treatment of severe acute left ventricular failure.
Acute congestive left ventricular failure
clinically manifests: paroxysmal shortness of breath, painful suffocation and orthopnea, occurring more often at night, sometimes - Cheyne-Stokes breathing, cough (first dry, and then with sputum, which does not bring relief), later - foamy sputum, often colored pink, pallor, acrocyanosis, hyperhidrosis and is accompanied by agitation and fear of death. In case of acute congestion, moist rales may not be heard at first, or a meager amount of fine bubbling rales is detected over the lower parts of the lungs; swelling of the mucous membrane of small bronchi can manifest itself as a moderate picture of bronchial obstruction with prolongation of exhalation, dry wheezing and signs of pulmonary emphysema. For differential diagnostics with bronchial asthma, dissociation between the severity of the condition and (in the absence of a pronounced expiratory nature of shortness of breath and “silent zones”) the paucity of the auscultatory picture can serve. Loud, varied moist rales over all the lungs, which can be heard at a distance - bubbling breathing, are characteristic of a detailed picture of alveolar edema. Possible acute expansion of the heart to the left, the appearance of a systolic murmur at the apex of the heart, a proto-diastolic gallop rhythm, as well as an emphasis on the second tone on the pulmonary artery and other signs of load on the right heart up to the picture of right ventricular failure; Tachycardia up to 120-150 per minute is possible. Blood pressure, depending on the initial level, can be normal, high or low.
The picture of acute congestion in the pulmonary circulation, which develops with stenosis of the left atrioventricular orifice, is essentially left atrial failure, but is traditionally considered together with left ventricular failure.
Cardiogenic shock
– clinical syndrome characterized by arterial hypotension (SBP less than 90-80 mm Hg, or 30 mm Hg below the “working” level in people with arterial hypertension, decreased pulse pressure and signs of a sharp deterioration in microcirculation and tissue perfusion, including blood supply to the brain and kidneys (lethargy or agitation, a drop in diuresis of less than 20 ml per hour, cold skin covered with sticky sweat, pallor, gray cyanosis, marbled skin pattern); sinus tachycardia, which has a compensatory nature.
A decrease in cardiac output with a clinical picture of cardiogenic shock can be observed in a number of pathological conditions not associated with insufficiency of myocardial contractile function - with acute obstruction of the atrioventricular orifice by an atrial myxoma or thrombus of a prosthetic valve, with pericardial tamponade, with massive pulmonary embolism. These conditions are often combined with the clinical picture of acute right ventricular failure. Pericardial tamponade and atrioventricular orifice obstruction require immediate surgical intervention; drug therapy in these cases can only worsen the situation. In addition, the picture of shock during myocardial infarction is sometimes imitated by dissecting aortic aneurysm (see), which requires differential diagnosis, since it requires a fundamentally different therapeutic approach.
There are three main clinical variants of cardiogenic shock:
- arrhythmic shock develops as a result of a drop in cardiac output due to tachycardia/tachyarrhythmia or bradycardia/bradyarrhythmia; after stopping the rhythm disturbance, adequate hemodynamics are quickly restored;
- reflex shock (pain collapse) develops as a reaction to pain and is characterized by a rapid response to pain therapy; absence of signs of congestive heart failure, deterioration of tissue perfusion (in particular, gray cyanosis); pulse pressure usually exceeds a critical level;
- true cardiogenic shock develops when the volume of damage exceeds 40-50% of the mass of the left ventricular myocardium (more often with anterolateral and repeated infarctions, in people over 60 years of age, against the background of arterial hypertension and diabetes mellitus), characterized by a detailed picture of shock that is resistant to therapy , often combined with congestive left ventricular failure; Depending on the chosen diagnostic criteria for this condition, the reported mortality rates (in the absence of surgical treatment) range from 80-100%.
In some cases, especially with the development of myocardial infarction in patients receiving diuretics, the developing shock is hypovolemic in nature, and adequate hemodynamics are relatively simply restored by replenishing the circulating volume.
DIAGNOSTIC CRITERIA.
One of the most consistent signs of acute heart failure is sinus tachycardia (in the absence of sick sinus syndrome, complete AV block or reflex sinus bradycardia); characterized by expansion of the borders of the heart to the left or right and the appearance of the third tone at the apex or above the xiphoid process.
In acute congestive right ventricular failure, the following have diagnostic value:
- swelling of the neck veins and liver,
- Kussmaul's sign (swelling of the jugular veins on inspiration),
- intense pain in the right hypochondrium,
- ECG signs of acute overload of the right ventricle (type S1-Q3, increasing R wave in leads VI,II and formation of a deep S wave in leads V4-6, depression STI,II,aVL and elevation STIII,aVF, as well as in leads V1,2 ; possible formation of blockade of the right bundle branch, negative T waves in leads III, aVF, V1-4) and the right atrium (high pointed waves PII, III).
In acute congestive left ventricular failure, the following are of diagnostic importance:
- shortness of breath of varying severity up to suffocation,
- paroxysmal cough, dry or with foamy sputum, foaming from the mouth and nose,
- orthopnea position,
the presence of moist rales heard over the area from the posterior-lower sections to the entire surface of the chest; local small-bubble rales are characteristic of cardiac asthma; with advanced pulmonary edema, large-bubble rales are heard over the entire surface of the lungs and at a distance (bubbling breathing)
Cardiogenic shock at the prehospital stage is diagnosed based on:
- SBP drops less than 90-80 mmHg. (or 30 mm Hg below the “working” level in people with arterial hypertension),
- decrease in pulse pressure - less than 25-20 mm Hg,
- signs of impaired microcirculation and tissue perfusion - a drop in diuresis of less than 20 ml per hour, cold skin covered with sticky sweat, pallor, gray cyanosis, marbled skin pattern, in some cases - collapsed peripheral veins.
ALGORITHM FOR TREATMENT OF ACUTE HEART FAILURE AT THE PREHOSPITAL STAGE.
For any clinical variant of acute heart failure, prompt correction of the condition that led to the development of such a formidable complication is indicated:
If the cause is cardiac arrhythmia, the basis for normalizing hemodynamics and stabilizing the patient’s condition is restoring normal heart rate.
a) For paroxysms of tachycardia and tachyarrhythmia, electrical pulse therapy is indicated, and if it is impossible to carry out it in the shortest possible time, specific antiarrhythmic therapy is indicated, depending on the nature of the rhythm disturbance (see chapter “ ARRHYTHMIAS ”)
b) In case of tachysystolic form of constant form of atrial fibrillation, atrial fibrillation of unknown duration or paroxysm of atrial fibrillation more than a day old, it is necessary to carry out rapid digitalization by administering digoxin intravenously in an initial dose of 1 ml of 0.025% solution,
c) with sinus bradycardia and sinoatrial block, it is sufficient to increase heart rate by intravenous administration of 0.3-1 ml of 0.1% atropine solution. If it is ineffective and with other bradyarrhythmias - slow rhythm from the AV connection (replacement), AV block of the II-III degree, electrical pacing is indicated. The impossibility of its implementation serves as an indication for drug treatment (for more details, see the chapter “ ARRHYTHMIAS ”);
If the cause is myocardial infarction, then one of the most effective methods of combating decompensation is the rapid restoration of coronary blood flow through the affected artery, which in prehospital care can be achieved using systemic thrombolysis (see chapter “MYOCARDIAL INFARCTION ” );
If acute heart failure is the result of acutely developed disturbances of intracardiac hemodynamics due to trauma, myocardial rupture, or damage to the valve apparatus, emergency hospitalization by a special team to a specialized surgical hospital to provide surgical care is indicated.
However, in practice, it is more often necessary to limit oneself (at least at the first stage of care) to pathogenetic and symptomatic therapy. The main task is to maintain adequate pumping function of the heart, for which different approaches are used depending on the clinical variant of acute heart failure. In any case, oxygen therapy plays a certain role in the fight against hypoxemia - inhalation of humidified oxygen through a nasal catheter at a rate of 6-8 l/min.
Treatment of acute congestive right ventricular failure consists of correcting the conditions that are its cause - pulmonary embolism (see), status asthmaticus (see), etc. This condition does not require independent therapy.
The combination of acute congestive right ventricular failure with congestive left ventricular failure is an indication for therapy according to the principles of treatment of the latter.
The combination of acute congestive right ventricular failure with small output syndrome (cardiogenic shock), caused by a decrease in blood flow into the pulmonary circulation and left ventricle, may require fluid infusion, sometimes coupled with inotropic therapy.
In the treatment of acute congestive left ventricular failure, the following areas are distinguished:
- Reducing preload on the myocardium and pressure in the pulmonary artery, for which they use appropriate body position and medications that have a venous vasodilating effect - Lasix, morphine, nitrates.
- Dehydration.
- Suppression of the respiratory center, reducing the work of the respiratory muscles and thereby providing physical rest to the patient. Suppression of the respiratory center helps to relieve the so-called “respiratory panic” (inappropriately deep and frequent breathing), leading to a further increase in shifts in the acid-base balance.
- Anti-foaming.
- Inotropic therapy (according to strict indications).
- Combating increased membrane permeability (if standard therapy is ineffective).
- Correction of microcirculatory disorders (as an auxiliary measure).
- Treatment of acute congestive heart failure begins with the administration of sublingual nitroglycerin in a dose of 0.5-1 mg (1-2 tablets) and giving the patient an elevated position (in case of an unexpressed picture of congestion - an elevated head end, in case of advanced pulmonary edema - a sitting position with legs down) ; these measures are not performed in cases of severe arterial hypotension.
- A universal pharmacological agent for acute congestive heart failure is furosemide (Lasix, Urix), which reduces the hemodynamic load on the myocardium due to venous vasodilation within 5-15 minutes after IV administration. Thanks to the diuretic effect that develops later, the preload decreases even more. Furosemide is administered intravenously as a bolus without dilution in a dose of 20 mg for minimal signs of congestion to 200 mg for extremely severe pulmonary edema.
- The more pronounced the tachypnea and psychomotor agitation, the more indicated is the addition of a narcotic analgesic to therapy - morphine, which, in addition to venous vasodilation and reducing preload on the myocardium, already 5-10 minutes after administration reduces the work of the respiratory muscles, suppresses the respiratory center, which provides an additional reduction in load on the heart. Its ability to reduce psychomotor agitation and sympathoadrenal activity also plays a certain role; the drug is administered intravenously in fractional doses of 2-5 mg (for which 1 ml of a 1% solution is adjusted to 10 ml with isotonic sodium chloride solution and 2-5 ml are administered) with repeated administration if necessary after 15 minutes. Contraindications are respiratory rhythm disturbances (Cheyne-Stokes breathing), severe depression of the respiratory center, acute obstruction of the respiratory tract, chronic decompensated cor pulmonale, and cerebral edema.
- Severe congestion in the pulmonary circulation in the absence of arterial hypotension, resistant to therapy, or any degree of acute congestive left ventricular failure during myocardial infarction, as well as pulmonary edema against the background of a hypertensive crisis without cerebral symptoms, are indications for intravenous drip administration of nitroglycerin or isosorbide dinitrate. The infusion is carried out under constant monitoring of blood pressure and heart rate at an initial dose of 10-15 mcg/min, followed by an increase every 3-5 minutes by 10 mcg/min until the desired effect is achieved or side effects appear, in particular, a decrease in blood pressure to 90 mmHg . Art. (every 10 mg of the drug is diluted in 100 ml of 0.9% sodium chloride solution; 1 drop of the resulting solution contains 5 mcg of the drug). Contraindications to the use of nitrates are uncompensated arterial hypotension, hypovolemia, pericardial constriction and cardiac tamponade, pulmonary artery obstruction, and inadequate cerebral perfusion.
- With the development of acute left ventricular failure against the background of a hypertensive crisis with cerebral symptoms, intravenous drip administration of a mixed vasodilator of myotropic action sodium nitroprusside (50 mg in 250 ml of 5% glucose solution) is indicated under the control of blood pressure and heart rate at an initial dose of 0.5 mcg/kg min, or 20 mcg/min with its increase every 5 minutes by 5 mcg/min until the expected effect is achieved (average dose - 1-3 mcg/kg min), the maximum rate of administration (5 mcg/kg min) or the development of side effects. Unlike nitrates, sodium nitroprusside not only reduces preload, but, by increasing arterial flow to tissues, in particular, increasing cerebral and renal blood flow, it also reduces afterload, which leads to a reflex increase in cardiac output. Sodium nitroprusside is more likely than nitrates to cause steal syndrome; Contraindications to its use are coarctation of the aorta and arteriovenous shunts; it requires special caution in old age.
- Modern vasodilating therapy, including powerful diuretics, has reduced to a minimum the importance of bloodletting and the application of venous tourniquets to the extremities, however, if it is impossible to carry out adequate therapy due to the lack of drugs, these methods not only can, but should be used, especially with rapidly progressing pulmonary edema ( bloodletting in a volume of 300-500 ml).
- In case of acute congestive left ventricular failure, combined with cardiogenic shock or with a decrease in blood pressure during therapy that has not given a positive effect, the addition of non-glycoside inotropic agents to treatment is indicated - intravenous administration of dobutamine at a dose of 2.5-10 mcg/kg min, dopamine 5 -20 mcg/kg/min. Persistent hypotension with SBP below 60 mm Hg. requires the addition of norepinephrine infusion (see “Treatment of cardiogenic shock” ).
- The means of directly combating foaming during pulmonary edema are “defoamers” - substances that ensure the destruction of foam, reducing surface tension. The simplest of these means is alcohol vapor. Alcohol is poured into a humidifier, passing oxygen through it, supplied to the patient through a nasal catheter or breathing mask at an initial rate of 2-3 liters, and after a few minutes - at a rate of 6-8 liters of oxygen per minute (less effective is the use of cotton wool moistened with alcohol, inserted into a mask); the disappearance of bubbling breathing is observed within a period of 10-15 minutes to 2-3 hours; the simplest method - spraying alcohol in front of the patient's mouth using any pocket inhaler or a regular spray bottle - is the least effective; in extreme cases, intravenous administration of 5 ml of 96% ethyl alcohol in the form of a 33% solution is possible.
- Persistent signs of pulmonary edema during stabilization of hemodynamics may indicate an increase in membrane permeability, which requires the administration of glucocorticoids for membrane stabilizing purposes (4-12 mg of dexamethasone).
- In the absence of contraindications, in order to correct microcirculatory disorders, especially with long-term intractable pulmonary edema, heparin is indicated - 5000 IU intravenously as a bolus, then drip at a rate of 1 thousand IU/hour with continued therapy in the hospital (see chapter “ MYOCARDIAL INFARCTION ” ).
Treatment of cardiogenic shock involves increasing cardiac output and improving peripheral blood flow in the following ways.
- Relief of adverse reflex effects on hemodynamics.
- Combating heart rhythm disturbances.
- Ensuring adequate venous return and diastolic filling of the left ventricle, combating hypovolemia and disturbances in the rheological properties of blood.
- Restoration of adequate tissue perfusion of vital organs.
- Stimulation of myocardial contractility with non-glycoside inotropic agents.
In the absence of signs of congestive heart failure (shortness of breath, moist rales in the posterior lower parts of the lungs), the patient must be given a horizontal position or even a Trendelenburg position (with the head end lowered), which contributes to an increase in venous return, an increase in cardiac output, and also an improvement in cerebral blood flow during centralized circulation .
Regardless of the characteristics of the clinical picture, it is necessary to provide complete analgesia (see chapter “ MYOCARDIAL INFARCTION ”).
Stopping rhythm disturbances (see above) is the most important measure to normalize cardiac output, even if, after restoration of normosystole, there is no restoration of adequate hemodynamics. Bradycardia may indicate increased vagal tone and requires immediate intravenous administration of 0.5-1 ml of 0.1% atropine solution.
To combat hypovolemia that occurs with right ventricular infarction or with previous dehydration (long-term use of diuretics, profuse sweating, diarrhea), intravenous isotonic sodium chloride solution is used in an amount of up to 200 ml over 10-20 minutes with repeated administration of a similar dose if there is no effect or complications.
The lack of effect from the entire complex of therapeutic measures, including the active fight against hypovolemia, or the combination of cardiogenic shock with congestive heart failure is an indication for the use of inotropic agents from the group of pressor amines.
a) dopamine (dopmin) at a dose of 1-5 mcg/kg min has a vasodilating effect, at a dose of 5-15 mcg/kg min - vasodilating and positive inotropic (and chronotropic) effects, and at a dose of 15-25 mcg/kg min - positive inotropic (and chronotropic) and peripheral vasoconstrictive effects. 200 mg of the drug is dissolved in 400 ml of 5% glucose solution (1 ml of the mixture contains 0.5 mg, and 1 drop - 25 mcg of dopamine); the initial dose is 3-5 mcg/kg min with a gradual increase in the rate of administration until the effect is achieved, the maximum dose (25 mcg/kg min) or the development of complications (most often sinus tachycardia exceeding 140 per minute, or ventricular arrhythmias). Contraindications to its use are thyrotoxicosis, pheochromocytoma, cardiac arrhythmias, hypersensitivity to disulfide, previous use of MAO inhibitors; If you have previously taken tricyclic antidepressants, the dose should be reduced.
b) dobutamine (Dobutrex), unlike dopamine, does not affect dopaminergic receptors, has a more powerful positive inotropic effect and a less pronounced ability to increase heart rate and cause arrhythmias. 250 mg of the drug is diluted in 500 ml of 5% glucose solution (1 ml of the mixture contains 0.5 mg, and 1 drop - 25 mcg of dobutamine); in monotherapy it is prescribed at a dose of 2.5 mcg/kg/min. with an increase every 15-30 minutes. by 2.5 mcg/kg/min. until an effect, side effect is obtained or a dose of 15 mcg/kg/min is achieved, and when dobutamine is combined with dopamine - in the maximum tolerated doses. Contraindications to its use are idiopathic hypertrophic subaortic stenosis, stenosis of the aortic mouth;
c) if it is not possible to use other pressor amines or if dopamine and dobutamine are ineffective, norepinephrine can be used in an increasing dose not exceeding 16 mcg/min (if combined with an infusion of dobutamine or dopamine, the dose should be halved). Contraindications to its use are thyrotoxicosis, pheochromocytoma, previous use of MAO inhibitors; if you have previously taken tricyclic antidepressants, the dose should be reduced;
If there are signs of congestive heart failure and in the case of using inotropic drugs from the group of pressor amines, the administration of peripheral vasodilators - nitrates (nitroglycerin or isosorbide dinitrate at a rate of 5-200 mcg/min) or sodium nitroprusside (at a dose of 0.5-5 mcg/kg) is indicated /min).
In the absence of contraindications, in order to correct microcirculatory disorders, especially with long-term intractable shock, heparin is indicated - 5000 IU intravenously as a bolus, then drip at a rate of 1 thousand IU/hour with continued therapy in the hospital (see chapter “ MYOCARDIAL INFARCTION ”).
COMMON THERAPY ERRORS.
Acute heart failure is a life-threatening condition, and therefore incorrect therapy can be fatal. All identified treatment errors are due to outdated recommendations , which are partially preserved in some modern standards of medical care at the prehospital stage.
The most common mistake in all clinical types of acute heart failure is the prescription of cardiac glycosides. In conditions of hypoxemia, metabolic acidosis and electrolyte disorders, which are invariably present in acute heart failure and cause increased sensitivity of the myocardium to digitalis, glycosides increase the risk of developing serious rhythm disturbances. The inotropic effect is achieved late and affects both the left and right ventricles, which can lead to an increase in pulmonary hypertension.
In acute heart failure , attempts to stop paroxysmal arrhythmias with drugs rather than by electrical cardioversion are dangerous, since most of the antiarrhythmic drugs used have a pronounced negative inotropic effect (exceptions include lidocaine for ventricular paroxysmal tachycardia and magnesium sulfate for ventricular paroxysmal tachycardia of the “pirouette” type). Equally dangerous are drug attempts to combat bradyarrhythmias, taken instead of cardiac pacing, which is not always effective and can be fraught with the development of fatal arrhythmias or an increase in myocardial oxygen demand.
In acute left ventricular failure ( both in small output syndrome and in congestive hemodynamics), glucocorticoid hormones are still widely used.
In case of cardiogenic shock, they are inferior to modern drugs in their effect on hemodynamics, but their use in large doses worsens potassium deficiency and increases the risk of arrhythmias, even fatal ones, and in case of myocardial infarction, myocardial ruptures become more frequent and scarring processes worsen (their use may be justified only in acute myocarditis).
In case of congestive left ventricular failure, aminophylline is traditionally used, to reduce pressure in the pulmonary artery system, stimulate diuresis and unloading is not justified, since modern drugs with vasodilating and diuretic activity (see above) are much more effective in this regard and, unlike aminophylline, are not increase myocardial oxygen demand and do not have an arrhythmogenic effect. Recommendations for the use of aminophylline to combat broncho-obstruction accompanying edema also seem unconvincing, since the obstruction is caused not so much by bronchospasm as by edema of the mucous membrane. In addition, obstruction, by increasing expiratory resistance, increases pressure in the alveoli, which partially prevents further exudation of fluid.
In case of cardiogenic shock , mesaton is relatively often used, which has very narrow indications only for the reflex nature of arterial hypotension caused by peripheral vasodilation. Mezaton does not increase cardiac output, but causes only peripheral vasoconstriction, which in most cases leads to worsening disturbances in the blood supply to vital organs, increasing the load on the myocardium and worsening the prognosis.
Relatively often one has to deal with the administration of pressor amines during cardiogenic shock without a preliminary attempt to compensate for hypovolemia, which, with inadequate blood volume, is fraught with the development of a critical state of microcirculation with a fatal deterioration in prognosis. However, excessive use of plasma expanders can provoke the development of congestive heart failure.
Unlike chronic, acute right ventricular failure should not resort to bloodletting.
INDICATIONS FOR HOSPITALIZATION.
Acute circulatory failure is a direct indication for hospitalization in the intensive care unit (unit) or cardiac intensive care unit.
If possible, patients with cardiogenic shock should be hospitalized in a hospital with a cardiac surgery department, because modern ideas about the treatment of this condition are clearly associated with aortic balloon counterpulsation and early surgical intervention.
Transportation is carried out on a stretcher in a horizontal position (for cardiogenic shock and right ventricular failure) and in a sitting position for congestive left ventricular failure.
previous article
Point of view about Beta blockers
next article
The Ministry of Health of the Republic of Belarus is 100 years old!
Top
Diagnostics
The process of diagnosing a disease begins with a general assessment of the patient's condition and medical history. Particular attention is paid to symptoms: onset, duration, how it manifested itself. Not only the heart, but also the lungs are examined. If a heart attack is suspected, a 12-lead ECG is performed. A general blood test and echocardiography are also performed.
Treatment
Medicines are used for treatment. The most commonly prescribed medications are ACE inhibitors, beta blockers, digoxin and diuretics (diuretics). Drug treatment helps prevent complications and improve quality of life.
Rhythm therapy and pacemaker implantation are also used for treatment. The second method allows you to activate the atria and ventricles. Often, a defibrillator is implanted as part of the pacemaker. It counteracts serious heart rhythm disturbances.
Unfortunately, heart failure cannot be completely cured. However, timely treatment can increase the patient's life expectancy. The prognosis depends not only on the type of disease, but also on age, lifestyle and bad habits.