Photo: M24.ru/Mikhail Sipko
“Man is mortal, but his main problem is that he is mortal suddenly,” these words, put into Woland’s mouth by Bulgakov, perfectly describe the feelings of most people. There is probably no person who is not afraid of death. But along with the big death, there is a small death - clinical. What is it, why do people who have experienced clinical death often see divine light, and is this not a delayed path to heaven - in the material M24.ru.
Clinical death from a medical point of view
The problems of studying clinical death as a borderline state between life and death remain one of the most important in modern medicine. Unraveling its many mysteries is also difficult because many people who have experienced clinical death do not fully recover, and more than half of patients with a similar condition cannot be resuscitated, and they die for real - biologically.
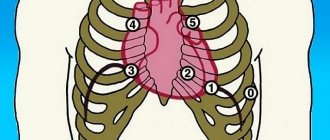
So, clinical death is a condition accompanied by cardiac arrest, or asystole (a condition in which various parts of the heart first stop contracting, and then cardiac arrest occurs), respiratory arrest and deep, or transcendental, cerebral coma. Everything is clear with the first two points, but about whom it is worth explaining in more detail. Typically, doctors in Russia use the so-called Glasgow scale. The eye opening reaction, as well as motor and speech reactions are assessed using a 15-point system. 15 points on this scale correspond to clear consciousness, and the minimum score is 3, when the brain does not respond to any type of external influence, corresponds to an extreme coma.
After stopping breathing and cardiac activity, a person does not die immediately. Consciousness turns off almost instantly, because the brain does not receive oxygen and oxygen starvation occurs. But nevertheless, in a short period of time, from three to six minutes, he can still be saved. Approximately three minutes after breathing stops, cell death in the cerebral cortex begins, the so-called decortication. The cerebral cortex is responsible for higher nervous activity, and after decortication, resuscitation measures may be successful, but the person may be doomed to a vegetative existence.
Photo: TASS/Sergey Bobylev
After a few more minutes, cells in other parts of the brain begin to die - in the thalamus, hippocampus, and cerebral hemispheres. A condition in which all parts of the brain have lost functioning neurons is called decerebration and actually corresponds to the concept of biological death. That is, reviving people after decerebration is, in principle, possible, but the person will be doomed to remain on artificial ventilation and other life-sustaining procedures for the rest of his life.
The fact is that vital (vital - M24.ru) centers are located in the medulla oblongata, which regulates breathing, heartbeat, cardiovascular tone, as well as unconditioned reflexes such as sneezing. During oxygen starvation, the medulla oblongata, which is actually a continuation of the spinal cord, is one of the last parts of the brain to die. However, despite the fact that the vital centers may not be damaged, by that time decortication will have already occurred, making it impossible to return to normal life.
Other human organs, such as the heart, lungs, liver and kidneys, can survive without oxygen for much longer. Therefore, one should not be surprised by the transplantation, for example, of kidneys taken from a patient who is already brain dead. Despite brain death, the kidneys are still in working order for some time. And the muscles and intestinal cells live without oxygen for six hours.
Currently, methods have been developed that can increase the duration of clinical death to two hours. This effect is achieved using hypothermia, that is, artificial cooling of the body.
Photo: TASS/Vladimir Smirnov
As a rule (unless, of course, it happens in a clinic under the supervision of doctors), it is quite difficult to determine exactly when cardiac arrest occurred. According to current regulations, doctors are required to carry out resuscitation measures: cardiac massage, artificial respiration within 30 minutes from the beginning. If during this time it was not possible to resuscitate the patient, then biological death is declared.
However, there are several signs of biological death that appear within 10–15 minutes after brain death. First, Beloglazov's symptom appears (when pressure is applied to the eyeball, the pupil becomes like a cat's), and then the cornea of the eyes dries out. If these symptoms are present, resuscitation is not performed.
Where does the feeling of bliss come from?
Many people who have experienced cardiac arrest have reported an incredible lightness that envelops their entire body, a feeling of euphoria, peace, and happiness that they have never experienced to such an extent before. But in fact, the reason for their appearance is quite understandable - during emergency situations, the body releases a certain amount of endorphins in order to “block” the strongest feeling of stress or pain. Considering that possible death is, in general, the most dangerous of all possible situations for the human body, the happiness hormone is produced in maximum quantities. In Germany, a study led by Alexander Wutzler proved that during clinical death the amount of serotonin increases at least three times.
How many people survive clinical death safely?
It may seem that most people who find themselves in a state of clinical death come out of it safely. However, this is not the case; only three to four percent of patients can be resuscitated, after which they return to normal life and do not suffer from any mental disorders or loss of body functions.
Another six to seven percent of patients, being resuscitated, nevertheless do not fully recover and suffer from various brain lesions. The vast majority of patients die.
These sad statistics are largely due to two reasons. The first of them is that clinical death can occur not under the supervision of doctors, but, for example, at the dacha, from where the nearest hospital is at least half an hour’s drive. In this case, doctors will arrive when it is no longer possible to save the person. Sometimes it is impossible to defibrillate in a timely manner when ventricular fibrillation occurs.
"Special Report": Beyond
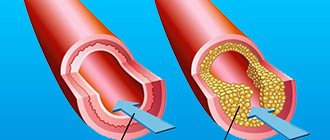
The second reason remains the nature of the damage to the body during clinical death. If we are talking about massive blood loss, resuscitation measures are almost always unsuccessful. The same applies to critical myocardial damage during a heart attack.
For example, if a person has more than 40 percent of the myocardium affected as a result of blockage of one of the coronary arteries, death is inevitable, because the body cannot live without heart muscles, no matter what resuscitation measures are taken.
Thus, it is possible to increase survival rate in case of clinical death mainly by equipping crowded places with defibrillators, as well as by organizing flying ambulance teams in hard-to-reach areas.
Near-death experience: people's memories
The most controversial and frequently discussed topic is the memories of people saved from clinical death. The images that people see in this state are often similar: bright light, tunnels, sensations of flying or falling, leaving the body, talking with deities or deceased relatives. Many believe that since patients' visions are similar, this can serve as evidence of the existence of an afterlife. But science has its own explanation for this phenomenon.
Organizing a funeral yourself - instructions
Eighth heart of David Rockefeller. How did the hundred-and-one-year-old billionaire die?
American billionaire David Rockefeller died today, March 20, at his home in New York. He was 101 years old. The New York Times reported this. According to Rockefeller family spokesman Fraser Seitel, the cause of death was chronic heart failure.
David Rockefeller was not only a legendary businessman (he is the ex-president of Chase Manhattan Bank, as well as the grandson of oil tycoon and the first dollar billionaire in history, John Davison Rockefeller). He also holds the record for the number of organ transplants.
He had a heart transplanted seven times - there was no other person in the world who owned eight hearts. David Rockefeller underwent his first transplant in 1976, when he was 62 years old. The last one will be in August 2021.
In the medical world, David Rockefeller is such a legend that Russian surgeons are quite familiar with the history of his illness.
“The reason for the first heart transplant was cardiomyopathy, a disease that rendered the heart muscle unusable,” cardiac surgeon Vladimir Khoroshev told Life. — Simply put, the heart has ceased to function as a pump, to perform its direct function. With such a diagnosis, an artificial heart has not yet been invented, there is only one way out - a transplant.
After the first transplant, David Rockefeller, as expected, took immunosuppressants - drugs that suppress the immune system so that the body does not reject the donor heart.
“Subsequent transplants to Rockefeller were done because the donor heart stopped functioning: the body still rejected the tissue of the new heart,” said Vladimir Khoroshev. — You need to understand that it is almost impossible for ordinary people to undergo a second transplant. It is very expensive. He had such an opportunity. A heart transplant is a very expensive operation. A minimum of 10–12 specialists take part in it, plus tests, diagnostics, and a search for a donor (usually donor hearts are taken from dead people). Such an operation, especially the last one he underwent at age 99, costs millions of dollars.
According to the doctor, the cause of the banker’s death was not surgery, but “a combination of reasons—primarily age.”
As Alexei Zhao, vice-president of the Interregional Public Organization of the Transplant Community, said, seven heart transplants are a unique case, and if the patient did not have a big name and an impressive budget, none of the specialists would undertake to transplant the organ.
In America, the patient or the insurance company pays for the operation itself, medications, and consumables, but the heart as a donor organ is priceless and cannot be bought. To get it, you have to go through a line. According to the doctor, it is not known for sure whether Rockefeller went through the line, especially all seven times, but it can be assumed that the famous name and money helped him speed up the process.
“So many transplant operations are determined by the fame and financial capabilities of the patient,” he said. “An ordinary patient rarely gets the chance to have a second transplant; a third is almost out of the question. This point is due to a large shortage and a waiting list for donor hearts.
The doctor noted that a fair queue is a very serious issue.
“Every patient has the right to a transplant if there is a vital need,” said the doctor. “But if there is a shortage of organs, the most optimal recipient is chosen, who will live longer. Therefore, when a person is 90 years old and has already had several transplants, doing another one is not advisable from a social point of view and in terms of costs. The heart could go to a young man who would live with him for another 50 years.
It is also known that David Rockefeller survived two kidney transplants.
Risk factors for sudden cardiac death
It is difficult to say for what exact reason a person’s heart suddenly stops beating during sleep. As a rule, autopsies in such situations do not show serious violations of the structure and structure of the heart. However, doctors are prepared to warn with a list of the most common causes of heart failure, which significantly increases the risk that you will experience sudden cardiac death at night.
First of all, this is a violation of blood flow in the heart area, coronary heart disease, disruption of the structure and function of the main heart muscle, blood clots and blockage of arteries, congenital and chronic diseases of the cardiovascular system, excess weight and diabetes. A separate group of risk factors includes previous heart attacks or cardiac arrest, and frequent episodes of loss of consciousness.
Official statistics state that all cases of unexpected death during sleep can be divided into three main causes: primary arrhythmia (47%), ischemic factors (43%) and insufficiency of the pumping function of the heart (8%).
Precursors of sudden cardiac death
Cardiologists and physiologists have compiled a small list of conditions that may precede sudden arrhythmic death and should seriously alert both the person and his loved ones.
- unexpected cases of severe weakness, sweating and dizziness, which quickly end.
- unnatural pallor of a person against the background of surges in blood pressure.
- pallor after physical exertion, during stress and emotional overstimulation.
- low rather than high blood pressure after any physical activity.
If at least one such episode occurs, you should seek help from a cardiologist and carry out the necessary examinations and, if necessary, treatment.
First aid
If you find yourself near a person who suddenly has a life-threatening attack, immediately call emergency services, open the windows in the room (to increase oxygen access), ask the person not to move under any circumstances and try to remain conscious for as long as possible.
If possible, medical assistance for unexpected cardiac death should be provided as early as possible - in the first 5-6 minutes after cardiac arrest and disappearance of signs of life.
Resuscitation measures include indirect cardiac massage (rhythmic pressure on the chest with a certain frequency, which helps push out blood and all cavities of the heart), artificial respiration (mouth to mouth). In a medical facility, it is possible to carry out defibrillation (applying electrical shocks to the chest with a special device), which is a very successful way to restore heart rhythm.
If measures to provide first aid to the patient are successful, he is hospitalized in the cardiology or intensive care unit for examination and identification of the causes of this condition. In the future, such people should regularly attend appointments with a cardiologist and follow all preventive recommendations.
Non-drug prevention of the causes of cardiac death can be considered giving up any bad habits, proper nutrition and exercise, positive emotions, avoiding stress and emotional stress.