Myocardial infarction is a focus of ischemic necrosis (death) of the heart muscle, resulting from an acute circulatory disorder in the coronary artery. Myocardial infarction is one of the most common forms of coronary heart disease (CHD). The condition poses a threat to human health and life and is the leading cause of death among adults in developed countries. Most often, symptoms of myocardial infarction are recorded in men (about 5 times more often than in women), and 70% of all sick people are aged 55–65 years. A heart attack manifests itself with extremely unpleasant symptoms: sharp pain in the chest, shortness of breath, cold sweat, and a feeling of fear. However, with timely identification of risk factors, diagnosis of a heart attack and provision of timely assistance during an attack of myocardial infarction in the clinic, it is possible to avoid tragic consequences.
Causes of heart attack
The direct cause of a heart attack is the sudden occurrence of an obstruction to blood flow in the branches of the coronary artery. In 95–97% of cases, such an obstacle is a blood clot formed as a result of atherosclerotic lesions of the arteries. In other cases, a heart attack occurs without any manifestations of atherosclerosis, and the main cause is a pronounced prolonged spasm of the coronary artery.
In extremely rare cases, myocardial infarction develops as a complication of other diseases (arteritis, developmental anomalies and injuries of the coronary artery, infective endocarditis, etc.). The likelihood of symptoms of an acute heart attack increases several times if the following risk factors are present:
- hyperlipoproteinemia (abnormal increase in the level of lipids and/or lipoproteins in the blood);
- old age (55 years and older);
- male gender;
- physical inactivity (lack of physical activity);
- obesity;
- smoking;
- diabetes;
- hypertonic disease;
- hereditary predisposition (presence of IHD in blood relatives).
The first symptoms in men
Male gender is one of the risk factors for the development of cardiovascular pathologies. Men are more likely to drink alcohol, smoke and experience stress. With age, the likelihood of the disease gradually increases.
Statistics show that in men, acute heart attack can be the initial manifestation of coronary artery disease. Many of them, even with pronounced signs of illness, do not always go to the doctor and undergo examination. Therefore, the disease is constantly progressing. Symptoms of a heart attack in men appear suddenly. They may be preceded by physical exertion, emotional distress, sudden hypothermia or overwork. Initial signs may be the following:
- Sharp dagger pain behind the sternum;
- Dyspnea;
- Smokers have an increased cough;
- Sticky sweat.
A person experiences a feeling of fear, which is clearly visible on his face. Painful sensations do not allow you to fully inhale or exhale.
They manifest signs of ischemia against the background of alcoholism and prolonged heavy drinking, atrial fibrillation, and atherosclerosis of the lower extremities. The pathology is combined with chronic obstructive pulmonary disease, which occurs due to smoking. Coronary syndrome can masquerade as acute pancreatitis, which occurs in patients with alcoholism. The following symptoms are of concern:
- Nausea, vomiting;
- Abdominal pain and bloating;
- Hiccups.
In older people, a heart attack can occur against the background of an existing arrhythmia. These can be various types of extrasystole or atrial fibrillation. The first and only sign is sudden cardiac arrest, which is manifested by loss of consciousness.
Symptoms of a heart attack
In most cases, the first symptoms of myocardial infarction are increasing manifestations of a person’s existing angina:
- pain in the sternum (longer and more intense);
- an increase in the area of pain and the appearance of irradiation (spread of pain to other areas: left arm, shoulder blade, collarbone, jaw);
- a sharp drop in exercise tolerance;
- a significant decrease in the effect of taking nitroglycerin;
- development of shortness of breath at rest, dizziness, general weakness.
Symptoms of a heart attack rarely appear against the background of new-onset angina or after a period of long remission. Often, the occurrence of an acute heart attack is provoked by one of the following factors:
- severe stress;
- significant physical stress;
- severe overheating or hypothermia;
- surgery;
- sexual intercourse;
- binge eating.
The typical course of the disease is characterized by the fact that the main complaints are associated with such symptoms of a heart attack as severe pain, which is localized behind the sternum. The pain can be burning, squeezing, cutting. Often symptoms of myocardial infarction include pain spreading to the left arm, shoulder blade and shoulder. However, antianginal drugs such as nitroglycerin do not have an analgesic effect. Compared to an attack of angina, the duration of pain is increased: from 30 minutes to several days. Even slight physical activity or stress increases pain.
Most people note that the painful symptoms of a heart attack have a pronounced emotional overtones: there is a feeling of fear of death, hopelessness, doom, and intense melancholy. The person becomes easily excitable, may scream, and strive to constantly change body positions. In addition, symptoms of myocardial infarction are severe weakness, shortness of breath, excessive sweating, nausea, vomiting, and dry cough.
The examination reveals in patients such objective symptoms of a heart attack as pale skin with blue discoloration of the nasolabial triangle and nails, the skin is moist to the touch. The pulse rate rises to 90–100 beats per minute, while blood pressure rises slightly. Often in the first days, an increase in body temperature to 37–38 °C is detected.
Symptoms and signs of myocardial infarction in women
Female heart attacks have a number of atypical features and are less studied compared to male ones. The thing is that women are less likely to suffer from coronary heart disease. They are helped in this by estrogen, a hormone that is produced by the female body almost throughout life. It prevents the development of atherosclerosis. After menopause, the amount of estrogen in the body decreases and the chances of developing coronary heart disease in women increase.
Precursors of myocardial infarction in women are often swelling of the extremities that appear at the end of the day, chronic fatigue, shortness of breath, and digestive problems.
Often, a heart attack in women occurs without severe chest pain and may be accompanied by nausea, high fever and high blood pressure. Sometimes a false toothache develops. There are also cases of asymptomatic heart attacks.
This course of the disease is much more dangerous, since the patient can endure the first signs of the disease without attaching much importance to them. Some patients who have experienced a heart attack find out about it only after a while, undergoing diagnostics.
Consequences of a heart attack
Myocardial infarction rarely goes away without leaving a trace. Its consequences in the form of complications can significantly reduce life expectancy. The most common complications of a heart attack are:
- early post-infarction angina;
- heart rhythm disturbances;
- cardiogenic shock (sharp decrease in myocardial contractility);
- acute cardiovascular failure;
- cardiac aneurysm (protrusion of the thinned wall of the heart);
- heart rupture (violation of its integrity).
After a heart attack, it is possible to return to a full life; the likelihood of this depends on many factors, including the timeliness and adequacy of treatment of the heart attack, the prevalence of tissue necrosis, and the presence of complications. Unfortunately, the mortality rate from a heart attack is high and amounts to about 35%. A third of those who have had the disease develop circulatory failure, in which people may lose their ability to work and become disabled.
Terms of rehabilitation for elderly people after a heart attack
Each case of heart attack is individual in its manifestations. But there are several general patterns. The official classification divides the severity of the disease into 4 degrees. The first degree is quite mild and is characterized by small focal lesions without complications. The fourth, the most severe, is dangerous due to large areas of damage, aneurysm and other serious consequences.
The duration of the recovery period directly depends on the assigned severity level. For example, if necrosis after a heart attack occupies a small area, then the patient undergoes rehabilitation for six months. Whereas an extensive myocardial infarction leads to complications that are eliminated only after a year, or even more. All subsequent stages of rehabilitation proceed much more slowly. Severe patients begin to walk and exercise much later.
Recommended articles on this topic:
- How to support your heart in old age
- What vitamins and minerals are needed by the heart of an elderly person?
- Health in old age: how to care for an elderly relative
If we talk about older people, then due to age and, as a consequence, deterioration of the body as a whole, complications after such a blow occur in them much more often. It is this fact that is associated with a significant increase in the rehabilitation time for older people after a heart attack (up to two years, subject to good care and strict adherence to medical recommendations).
Diagnosis of myocardial infarction
In a typical course, the diagnosis of acute myocardial infarction is performed based on an analysis of the clinical picture of the disease. To confirm the diagnosis, electrocardiography and laboratory diagnostics are used. The presence of an atypical form can usually be determined only with the help of additional methods for diagnosing a heart attack. The main diagnostic signs of myocardial infarction are the following:
- prolonged pain (more than 30 minutes), which is not eliminated with nitroglycerin;
- characteristic pattern on the electrocardiogram;
- an increase in erythrocyte sedimentation rate (ESR), leukocytosis, detected by a general blood test;
- deviation of biochemical parameters from the norm (detection of C-reactive protein, increase in the level of fibrinogen, sialic acids);
- the presence in the blood of markers of myocardial cell death.
It is not difficult to distinguish between the symptoms of myocardial infarction and signs of other diseases with severe pain in the heart area (angina pectoris, pleurisy, pulmonary embolism, spontaneous pneumothorax, intercostal neuralgia, etc.) when diagnosing a heart attack. With an atypical course, it is more difficult: the abdominal form can be mistaken for food poisoning, peptic ulcer, pancreatitis, acute cholecystitis; cerebral form - for a stroke.
Heart attack and other age groups
In recent years, the number of young people suffering from heart attacks has tripled in Russia. In children 10-16 years old, doctors diagnose fibrous cholesterol plaques - indirect signs of a heart attack. The disease is becoming a threat not only to older people.
The modern rhythm of life in big cities is invariably associated with unhealthy eating on the go, a sedentary lifestyle, stress at work, and prolonged depression. People do not pay enough attention to their health, rarely spend time in the fresh air, and do not get enough sleep. All this negatively affects the condition of blood vessels and the functioning of the heart.
It is necessary to check your health regularly. Diseases may remain dormant for a long time and not cause trouble, but this does not mean that they do not exist. The employer obliges its employees to undergo a medical examination annually and this should not be taken lightly. Often with such examinations it is possible to identify and eliminate pathology in time.
To avoid problems, you should use the universal recipe for health - engage in accessible sports, review your diet, give up tobacco and alcohol, and learn to control your emotions!
Treatment of heart attack
If qualified treatment of myocardial infarction is started in a timely manner, this largely determines the prognosis of the disease and the severity of the consequences. In the most acute and acute periods of the disease, hospital therapy is necessary. Treatment for a heart attack includes:
- relief of pain with analgesics, anesthesia with nitrous oxide for persistent pain;
- oxygen therapy – oxygen inhalations are performed using nasal catheters, flow rate 3–4 l/min;
- restoration of coronary blood flow using thrombolytic therapy;
- improving blood supply to the damaged area of the myocardium with the help of nitrates, β-blockers and calcium antagonists;
- prevention of heart rhythm disturbances using magnesium solution;
- stabilization of the emotional state with the help of sedatives, tranquilizers and psychotherapy;
- compliance with the daily regimen: first bed rest, after 2 weeks - ward rest, minimum physical activity (only dosed walking). The average duration of inpatient treatment for heart attack is 3 weeks.
- Compliance with the diet: diet during the acute period with the exclusion of “heavy” foods from the diet, increasing the frequency of meals and reducing the amount of food consumed at a time.
Diagnostics
Carried out in a hospital. Immediately after moving the patient within the walls of the institution, a minimum of studies are prescribed. Measurement of blood pressure, heart rate, and auscultation.
Then the stabilization of the victim’s condition begins with the use of drugs based on organic nitrates and other means.
An extensive, large-focal infarction has an unfavorable prognosis in 70% of cases, therefore the chances of recovery and even bringing the person’s position to an acceptable state are low.
If successful, the patient is transferred to intensive care, and as he stabilizes, he is transferred to a regular ward. Then a thorough diagnosis is prescribed.
Activity:
- Oral interview and history taking to identify key points.
- Measurement of blood pressure, heart rate. After the fact, to establish the status and success of primary actions.
- Electrocardiography. To identify consequences and causes.
- Echocardiography. Makes it possible to see all complications and organic defects. It is considered the main diagnostic method.
- Daily Holter monitoring if indicated.
- MRI of the chest.
The differential technique requires special tests. Shchetkin-Blumberg and others (to identify damage to the digestive tract). The task of urgent differentiation lies with doctors.
Prevention of heart attack
The goal of primary prevention of myocardial infarction is to combat coronary heart disease and eliminate risk factors. Quitting smoking, maintaining an active lifestyle, systematic moderate physical activity, maintaining normal body weight, and a balanced diet will help prevent the development of a heart attack.
Secondary prevention aims to combat the development of recurrent infarctions: preventive measures include the prescription of anticoagulants, β-blockers, and calcium antagonists. An important point is to ensure patency of the coronary artery. This can be accomplished by cardiac bypass surgery or stenting of cardiac vessels.
If you need an examination to identify risk factors or treat a heart attack, the ABC-Medicine clinic offers you its assistance. To ask any question you are interested in about diagnosing a heart attack or any other aspects of the problem, as well as to make an appointment with a specialist, call +7.
Heart attacks
CARDIAC ISCHEMIA
Coronary artery disease (CHD) is defined as acute or chronic damage to the heart caused by a decrease or cessation of blood supply to the myocardium (heart muscle) as a result of pathological changes in the coronary artery system. The basis of this disease is the discrepancy between the ability to supply the myocardium with oxygen and the need for it.
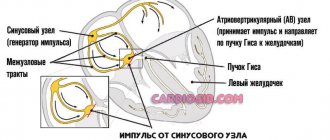
The human heart works constantly throughout his life and needs a constant supply of oxygen and nutrients. To achieve this, the heart has its own branched system of blood vessels, which in appearance resembles a crown or crown. Therefore, the vessels of the heart are called coronary or coronary. The work of the heart is continuous, and the movement of blood through the vessels of the heart must also be continuous.
Clinical manifestations of coronary artery disease include angina pectoris, myocardial infarction, cardiac rhythm and conduction disturbances, and heart failure.
Despite significant advances made over the past three decades in the prevention, diagnosis and treatment of coronary artery disease, this disease is currently the main cause of premature mortality and disability in most industrialized countries.
Myocardial ischemia is associated with a decrease in vessel diameter caused by both the development of atherosclerotic plaque and changes in vascular tone as a result of dysregulation. The consequence of ischemia is a violation of metabolism, electrical functions and myocardial contractility.
Risk factors for atherosclerosis and coronary artery disease
Unchangeable
- Age factor (aging of the body);
- The influence of gender (the predominance of IHD in young and middle age in men); for women, the dangerous age occurs after 50 years;
- Hereditary predisposition (coronary heart disease, heart attack, cerebral stroke, in at least one of the direct relatives: parents, grandparents, especially if the disease began before the age of 55);
Correctable
- Arterial hypertension (more than 140/90 mm Hg at any age);
- Smoking (one of the most significant risk factors!);
- Unbalanced diet (consumption of high-calorie foods rich in saturated fats and cholesterol);
- elevated blood cholesterol (more than 5 mmol/l or more than 200 mg/dl);
- Excess body weight and sedentary lifestyle;
- Insufficient physical activity;
- Psycho-emotional stress.
MYOCARDIAL INFARCTION is one of the clinical forms of coronary heart disease, accompanied by the development of ischemic myocardial necrosis (tissue death) caused by an acute violation of coronary circulation as a result of a discrepancy between the need of the heart muscle for oxygen and its delivery to the heart. Over the past 20 years, mortality from myocardial infarction in men has increased by 60%. The heart attack made me look much younger. Nowadays it is no longer uncommon to see this diagnosis in thirty-year-olds. So far it spares women up to 50 years of age, but then the incidence of heart attacks in women is compared with the incidence in men.
Myocardial infarction occurs when blood flow to the heart muscle is significantly reduced or stopped as a result of prolonged spasm or blockage of the arteries supplying the heart muscle. Contributing factors may include mental stress, nervous shock, smoking, and excessive physical activity.
The onset of myocardial infarction is considered to be the appearance of an attack of intense, painful, often accompanied by a feeling of fear of approaching death, sometimes extremely acute (“dagger-like”) and prolonged (more than 30 minutes, often many hours) chest pain, which does not go away after taking nitroglycerin. The pain can radiate to the left arm, lower jaw, ear, stomach area, or spine. Sometimes, especially in old age, the onset of a heart attack may differ from the picture described above: pain behind the sternum may be slight or completely absent, or may first appear in the area of the left shoulder, larynx, lower jaw, or left shoulder blade. Also, the onset of a heart attack can manifest itself in the form of lack of air, cough with foamy sputum, dizziness, nausea, vomiting, confusion. Such forms are called atypical.
The first signs of myocardial infarction are:
- severe, prolonged chest pain (more than 30 minutes)
- no improvement after taking nitroglycerin
- feeling of "fear of death"
- pale face, cold forehead
- acute feeling of pressure in the chest (a feeling of a “clenched fist”)
- sometimes (especially in women) vomiting
- lack of air, shallow breathing
What to do?:
- call an ambulance
- provide psycho-emotional peace
- ensure a comfortable, least painful position (sitting with your legs slightly raised up and your knees bent)
- unbutton your clothes, free your neck
- provide access to fresh air (open a window)
- take a nitroglycerin tablet under the tongue, repeat after 3 minutes (but not more than 3 tablets). Attention: nitroglycerin lowers blood pressure, so the position must be sitting or lying down, and the number of tablets should not exceed 3.
- Chew ½ aspirin tablet
The measures taken can significantly reduce the development of complications of myocardial infarction (cardiogenic shock, pulmonary edema, etc.) and prevent death.
PREVENTION:
NUTRITION Numerous clinical studies and observations have confirmed the effectiveness of a low-calorie diet rich in vegetables, fruits, fish, grains and nuts, and garlic in the prevention of cardiovascular diseases. On the contrary, with excessive consumption of foods rich in fats and lipids, the risk increases by 2.5-5 times. The amount of salt received daily in all forms should not exceed 6 grams, and in the case of arterial hypertension (AH) - 5 grams.
It has been noted that among people who eat fish at least once a week, the risk of death from a heart attack or stroke is on average 52% (!) lower than among those who eat fish less often. Three or more servings of vegetables and fruits per day reduce cardiovascular risk by 27%, and the risk continues to decrease as their consumption increases.
Nutrition is an important factor in controlling blood glucose levels in patients with diabetes, since the risk of cardiovascular disease in people with this disease is high.
CONTROL OF BLOOD PRESSURE Various studies prove that arterial hypertension increases the risk of developing coronary artery disease and, in particular, myocardial infarction. With systolic blood pressure 180 mmHg. and higher, IHD develops 8 times more often than with normal blood pressure. Therefore, the need to prevent hypertension is beyond doubt, and implies monitoring blood pressure, promptly identifying and preventing increases in blood pressure, strictly following his instructions when a doctor prescribes drug therapy, and also combating smoking, overeating, excessive consumption of table salt and excess body weight.
BODY WEIGHT AND PHYSICAL ACTIVITY The risk of death from coronary heart disease in physically inactive people is 3 times higher than in physically active people. Regular exercise normalizes cholesterol levels in the blood, blood pressure, blood sugar levels and, of course, helps get rid of excess weight. There is also an opinion that properly selected physical exercises not only strengthen the cardiovascular system, but also have a positive effect on mood and are successfully used in the treatment of depression. Young healthy people can regularly run in the morning, do morning exercises, and play various sports. For older people, as well as those suffering from coronary heart disease, and even more so for those who have suffered a myocardial infarction, a set of physical exercises (physical exercises) should be prescribed by a general practitioner or cardiologist.
Excess body weight (obesity) significantly increases the risk of developing coronary heart disease; proper nutrition and regular exercise help normalize weight.
SMOKING Smoking increases the risk of myocardial infarction, sudden death and the development of atherosclerosis, leads to an increase in total cholesterol in the blood, causes damage to the walls of blood vessels, and reduces its elasticity. In addition, cigarette smoke contributes to the development of conditions that lead to blood clots. The volume of hemoglobin that delivers oxygen is reduced. Quitting smoking reduces the risk of cardiovascular accidents by 60%.
The effectiveness of the most active strategies using psychotherapy, nicotine replacement patches and tablets reaches 40%.
ALCOHOL Alcohol abuse significantly increases the risk of coronary heart disease through other risk factors, increasing blood pressure, body weight, and blood cholesterol levels. In addition to influencing the development of coronary artery disease, alcohol contributes to damage to the heart, liver, pancreas, central nervous system, and significantly increases the risk of strokes, especially hemorrhagic and subarachnoid hemorrhages, hypertension, arrhythmias, sudden death, alcoholic cardiomyopathy, and breast cancer in women.
PSYCHOLOGICAL FACTORS The important role of factors such as depression, loss of social support, stress, and emotional personality in the development of MI and strokes is generally recognized. Stress and mental overstrain contribute to an increase in blood cholesterol levels, heart rate, and cause vasospasm. In addition, social and professional stress can contribute to the emergence of other risk factors for the development of coronary artery disease: increased blood pressure, increased smoking intensity, overeating, or even lead to coronary artery thrombosis.
What is a heart attack and what do you need to know about it?
To pump blood, the heart constantly needs oxygen and nutrients. The two large coronary arteries supply oxygenated blood to the heart muscle. If one of these arteries or their branches suddenly becomes blocked, a certain part of the heart becomes starved of oxygen. This phenomenon is called cardiac ischemia.
In the case of prolonged cardiac ischemia, tissue that does not receive oxygen dies, which is actually called a heart attack, myocardial infarction, or, literally speaking, the death of the heart muscle.
Most heart attacks last for several hours, so don't wait to seek help if you suspect a heart attack. In some cases, heart attack symptoms may not appear at all, but most heart attacks cause chest pain. Other signs of a heart attack include:
- difficulty breathing;
- dizziness;
- fainting;
- nausea.
The pain that occurs during a heart attack can be compared to a feeling of compression of the heart. The pain may be constant or intermittent. It is also worth noting that the signs of a heart attack in women and men may be different.
Who is at risk of a heart attack
We can distinguish groups of patients whose risk of death from myocardial infarction is very high:
- resuscitated after cardiac arrest, clinical death;
- people with acute heart failure (the contraction function of the heart muscle is not fully restored);
- persons with a history of myocardial ischemia (reduced blood flow to certain areas of the heart);
- patients with pronounced hypertrophy (thickening) of the left ventricle, which is visible during examination;
- patients with congenital or fatal diseases or those with irreversible anatomical changes in the heart (valve prolapse, athlete's heart, congenital anomalies in the coronary vessels, sarcoidosis);
- patients with any neoplasms of the myocardium;
- suffering from apnea (stopping breathing) during sleep.
When you don't die from a heart attack
A favorable prognosis is given to patients with minor, localized myocardial damage, when only part of the organ is susceptible to necrosis. In this case, the cells that remain unharmed take over the functions of the entire organ, and the person, having undergone the necessary therapy and rehabilitation measures, continues to live. However, it is extremely important to follow all the recommendations of your doctor.
Medicine does not stand still: scientists are working to create drugs and techniques that will reduce mortality from heart attacks. Until this happens, a person must take care of his health to avoid a heart attack.