Sudden cardiac arrest during sleep in Russia causes from eight to sixteen deaths per every ten thousand population annually. The majority of people who experienced cardiac arrest suffered from mental disorders (45%), asthma (16%), heart disease (11%), and gastritis (8%). In some patients (22%), sudden death was the first manifestation of the disease.
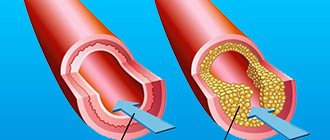
Patients who suffer from cardiac arrest during sleep for a few seconds are also worried about lack of vigor, headache in the morning, decreased performance, snoring, increased irritability, unbalanced behavior, impotence and decreased libido, memory impairment. Such patients are more likely to have metabolic syndrome or atherosclerosis.
Causes of cardiac arrest
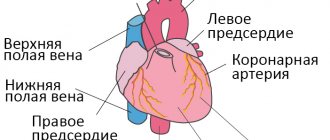
The causes of cardiac arrest at night during sleep are divided into direct cardiac and external. The main cardiac (cardiac) factors are increased blood pressure, atherosclerotic cardiosclerosis, myocardial ischemia and inflammation, acute vascular obstruction due to embolism or thrombosis, rhythm disturbances, and the development of cardiac tamponade.
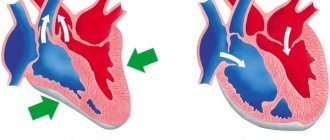
With cardiac tamponade, fluid accumulates between parts of the pericardium. The cavities of the heart are compressed, the muscle cannot contract normally. This condition directly threatens the patient’s life and requires urgent treatment. The pathology is characterized by the presence of complaints that patients usually present with heart failure.
Other causes of cardiac arrest during sleep include:
- loss of a significant volume of fluid due to ongoing diarrhea or vomiting, injury, shock;
- unilateral compression of one lung;
- the appearance of air between the layers of the pleura;
- oxygen deficiency caused by suffocation or anemia;
- severe allergies;
- hypothermia of the body (below 28 degrees);
- metabolic disorders or acute hypercalcemia.
In medical practice, hypercalcemia is a pathological increase in calcium levels in the blood. This occurs due to increased leaching of calcium from bone tissue, decreased absorption of calcium by bones, active absorption of the substance in the intestine, slow excretion from the body, or a combination of several factors. The clinical manifestations of this pathology are varied.
Why do apnea and sleep disorders lead to heart problems?
Your heart is also at risk. If you have sleep apnea, you are at increased risk for developing heart disease, even if you are otherwise healthy. According to statistics, over the past 15 years, cardiovascular diseases have been the leading cause of death worldwide, and sleep-disordered breathing is associated with a number of cardiovascular diseases, including hypertension, myocardial infarction and ischemia, congestive heart failure...
Patients suffering from sleep apnea have an increased risk of developing cardiovascular disease, even if they are young, in excellent shape, eat a healthy diet, exercise regularly...
Scientists aren't entirely sure why we need sleep to keep our heart healthy. However, they were able to establish that when we wake up frequently at night or regularly experience lack of sleep, certain biological functions of our body are disrupted. These disturbances (for example, if you stop breathing during sleep) lead to hormonal and chemical imbalances, which contribute to high blood pressure, low blood oxygen levels, changes in sugar metabolism, obesity... Together, these changes lay the foundation for the development of heart disease.
When you experience repeated pauses in breathing during sleep, the level of oxygen in your blood drops, your body tells your heart to beat faster and harder to supply oxygen to your vital organs, and as a result, your blood pressure rises. This frequent drop in oxygen levels is thought to damage the blood vessels supplying the heart. Also, the stress on the heart due to severe obstructive sleep apnea can cause the heart to become enlarged, leading to oxygen deficiency because the enlarged heart cannot pump blood effectively.
A 2015 study published in the Canadian Journal of Cardiology found that OSA is much more common in patients with heart failure than in the general population. Sleep apnea may contribute to the progression of heart failure.
Untreated OSA can lead to related conditions such as obesity, diabetes, stroke...
What happens during cardiac arrest
After sudden cardiac arrest during sleep, clinical death occurs in the second minute. Afterwards, the pupils dilate and do not react to the light source, and the skin quickly turns pale or acquires a pronounced bluish tint. These are the signs by which you can identify an extremely dangerous condition. In order for a person to survive, it is necessary to “start” the heart (perform an indirect massage) a maximum of five to seven minutes after stopping.
Diagnosis of sudden cardiac arrest
Cardiac arrest during sleep includes the initial symptoms of clinical death. With effective resuscitation, this phase is reversible. Therefore, resuscitation must begin as quickly as possible.
With complete loss of consciousness, the patient does not respond to braking or shouting. After the activity of the heart muscle stops, the brain dies on average within seven minutes, since it is the first to suffer from oxygen deficiency, and the stop of metabolic processes causes cell death.
During diagnosis, it becomes impossible to determine the pulse in the carotid artery, but this sign depends on the experience of others. If there is no pulsation in the carotid artery, then you can try to listen to the heartbeat by placing your ear to the victim’s chest. After making sure that the heart is not beating, you need to immediately begin resuscitation measures.
Other symptoms of cardiac arrest during sleep include dilation of the pupils, lack of reaction of the pupils to light, the appearance of individual seizures, and a change in skin color to pale or bluish. If an ambulance manages to arrive at the scene of the incident, then an electrocardiogram can confirm the simultaneous breathing disorder (in some cases, breathing does not stop completely, but is disrupted, which is accompanied by noisy breaths, the interval between which can be up to two minutes).
The most common diseases of the cardiovascular system:
- Hypertension
(high blood pressure): Places additional stress on the heart and damages blood vessels.
During sleep, your blood pressure usually drops by about 10-20%. When you stop breathing, your oxygen levels drop. The brain's response to lack of oxygen is to release adrenaline as well as constrict blood vessels to increase the flow of oxygen to vital organs such as the heart and brain, leading to increased blood pressure. That is, sleep apnea causes a constant jump in high blood pressure, increasing it by 10-20% above normal. A constant surge of high blood pressure can continue during waking hours, leading to the development of hypertension.
That is, when the force of blood flowing through the vessels is constantly too high, the circulatory system can become damaged, which can lead to a heart attack, stroke….
- Arrhythmia
(heart rhythm disorder) – the heart beats irregularly or differently than normal:
Obstructive sleep apnea can contribute to arrhythmias due to:
- repeated episodes of oxygen starvation (hypoxia);
- increased levels of carbon dioxide in the blood (hypercapnia);
- direct effects on the heart due to changes in chest pressure.
- Stroke
– vascular diseases of the brain:
It is the second leading cause of death worldwide. It is also a leading cause of long-term disability. Insufficient sleep caused by obstructive sleep apnea is significantly associated with stroke risk, even in the absence of other risk factors, including age, gender, race, smoking status, alcohol use, diabetes, or hypertension.
The more severe the symptoms of OSA, the higher the risk of stroke, particularly in middle-aged and older people, and especially in men. Scientists speculate that the difference in risk between men and women may be due to the fact that men are more likely to develop sleep apnea at a younger age and therefore go untreated for OSA for a longer period of time than women.
Signs of imminent cardiac arrest
Cardiac arrest during sleep is a sudden condition, but many patients noted the appearance of signs of the imminent onset of such a dangerous condition. 35% of patients had at least one sign indicating the presence of heart disease, Danish scientists say. In 17% of cases, a few hours before cardiac arrest, the person lost consciousness or felt chest pain (34%) - this is the most common symptom. Some patients experienced shortness of breath (29%).
According to the results of American studies, every second person who suffered sudden cardiac arrest during sleep experienced problems with the functioning of the heart muscle several weeks before the attack. Half of the men and more than half of the women reported chest pain or difficulty breathing four weeks before the attack. Almost all (93%) had the same symptom the day before cardiac arrest.
Treatment
To restart a stopped heart muscle in a medical facility, doctors use:
- Adrenalin;
- Norepinephrine;
- Atropine.
The listed drugs stimulate the activity of the heart. After the injection is administered, an electrocardiogram is taken. If necessary, the heart is started using a defibrillator, a device that creates an electrical shock. The device is already used in the intensive care unit to deliver the victim alive to the clinic .
Medicines for cardiac therapy
Patients are treated using the following medications:
- Heart failure: causes, symptoms, treatment and prevention
- Adrenaline allows you to strengthen and accelerate the contraction of the heart muscle.
- Atropine is administered if asystole develops.
- Lidocaine suppresses arrhythmia.
- Sodium bicarbonate is infused if the heart has stopped for a long time, the activity of the organ has stopped due to acidosis or hyperkalemia.
- Magnesia helps stabilize and activate the heart muscle.
- Calcium eliminates hyperkalemia.
Proper use of medications allows for effective therapy. The chances of survival for a person whose heart has stopped in his sleep increase many times over.
Some patients require surgery. Patients have a pacemaker implanted into their heart muscle.
Rehabilitation period
When returning home, the patient must follow all medical recommendations:
- forget about bad habits;
- take medications prescribed by the doctor;
- undergo regular preventive examinations.
If the patient takes glycosides and leads a healthy lifestyle, relapse does not occur . A person has a chance to become a long-liver.
Consequences of cardiac arrest
The severity of the consequences depends on the speed and correctness of medical care. According to statistics, only one out of twenty people can be saved from death when the heart stops during sleep. Prolonged oxygen deficiency leads to the appearance of irreversible foci of ischemia in the brain, damage to the kidneys and liver. When carrying out resuscitation measures, fractures of the ribs, sternum, and accumulation of air or gases in the pleural cavity are possible.
Consequences from the brain can be partial or complete memory impairment, paroxysmal convulsions in the limbs, involuntary chewing movements, visual or auditory hallucinations, blindness accompanying irreversible changes in the optic nerves (while vision is restored in rare cases).
Stopping the activity of the heart muscle is not only provoked by cardiac diseases, but can also become a significant risk factor for the development of other pathologies.
Non-epileptic paroxysms during sleep
According to the International Classification of Sleep Disorders ICSD, the following groups of disorders are distinguished:
- parasomnias:
- dyssomnia;
- sleep disorders in somatic diseases,
- sleep disorders in psychiatric diseases.
PARASOMNIAS
Parasomnias are phenomena of non-epileptic origin that occur during sleep, but are not per se sleep disorders (Parkes, 1985).
In most cases, parasomnias occur during full or partial awakening, or when changing stages of sleep. Within the heterogeneous group of parasomnias, there are disorders of awakening, disorders of the transition from sleep to wakefulness, disorders combined with the REM sleep phase, etc. Polysomnography plays an important role in the differential diagnosis of parasomnia and epileptic paroxysms.
AWAKENING DISORDERS
Sleepy intoxication (ICSD 307.462)
The term "sleep intoxication" refers to a state of confusion during or after awakening from sleep (usually awakening from deep sleep in the first half of the night) (Roth et al, 1981). Sleepy intoxication is a nonspecific phenomenon observed in many hypersomnias,
Clinical characteristics. Sleepy intoxication can occur spontaneously or be provoked by a sudden awakening. Disorientation and short-term (several minutes) slowness after awakening are characteristic. Episodes of sleepy intoxication in some cases can be longer - up to 1 hour or more.
Episodes of sleepy intoxication are not accompanied by vegetative symptoms (tachycardia, tachypnea), hallucinations, fear, or circling around oneself.
Data from laboratory and functional studies. Polysomnography. Changes occur during deep sleep - non-REM-IV.
Differential diagnosis should be made with complex partial seizures, other parasomnias (for example, nightmares).
Sleepwalking (somnambulism) (ICSD 307.46-0)
The term “somnambulism” means a pathological condition characterized by sleepwalking and changes in behavior during deep sleep.
Clinical characteristics. The disease manifests mainly during puberty (Kavey et al, 1990) and ends in the postpubertal period (Cirignotta et al, 1983). It is also possible for the disease to develop in adults, however, in comparison with children, severe psychopathological disorders are observed in adults. Clinical manifestations of somnambulism have been well known since ancient times. The leading symptom is sleepwalking. Attempts to wake up a patient with somnambulism, as with other parasomnias, are futile and can lead to manifestations of aggressiveness. Sometimes aggression in patients with somnambulism can be observed spontaneously (Gottlieb et al, 1986). People around should be warned about the possible aggressive actions of patients and the undesirability of interrupting an attack by forcibly awakening. Sometimes sleepwalking becomes complex, which is manifested not only by wandering around the room, but also by leaving the house. The duration of episodes of somnambulism ranges from a few seconds to several minutes. Provoking factors are: stress, emotional disorders, taking various medications - neuroleptics, antidepressants, antihistamines, barbiturates (Niarahua, 1979), and sometimes lithium preparations (Charney et al, 1979).
Data from laboratory and functional studies. Attacks of somnambulism are observed during the deep non-REM-IV sleep phase (Blatt et al, 1991). A polysomnographic study reveals prolongation of slow-wave sleep phases, an increased frequency of incomplete awakenings, and hypersynchronous delta activity.
The differential diagnosis of somnambulism should be carried out, first of all, with psychomotor attacks of temporal and frontal localization. Psychomotor attacks are usually shorter, often accompanied by an aura and oroalimentary automatisms. In addition, it is fundamentally important to have a history of daytime paroxysms, which supports the diagnosis of “partial epilepsy.” Significant assistance in differential diagnosis is also provided by neuroradiological research methods - CT, NMR, positron emission tomography, which often detect structural brain damage in partial epilepsies. EEG video monitoring allows us to identify patterns characteristic of partial epilepsies.
Treatment. Regular sleep and strict control by others over the child’s behavior are necessary. Benzodiazepines have a satisfactory effect (Clement, 1970: Reich, Gutnik, 1980), as well as hypnosis (Hurwitz et al, 1991).
Nightmares (ICSD 307.46 1)
Nightmares are a pathological condition characterized by sudden awakening during deep sleep, screaming, autonomic disorders (tachycardia, tachypnea, redness of the skin, mydriasis) and changes in behavior accompanied by a pronounced feeling of fear.
Clinical characteristics. Nightmares occur primarily in childhood and disappear in adolescence. Boys are more often affected (Kramer, 1979). Paroxysm occurs in the first third of the night. The patient suddenly screams loudly, sits up in bed, there is disorientation and an expression of fear on his face. Sometimes the behavior of patients becomes panicky. Autonomic symptoms such as tachycardia and tachypnea are also typical. Clinical manifestations are more pronounced the longer the patient remains in a state of deep sleep. Attempts to calm a child during an attack are of little help. Children with nightmares usually have normal intelligence. There were no behavioral disturbances in the interictal period.
Data from laboratory and functional studies. Nightmares occur during the slow-wave sleep phase - non-REM-III-IV. The EEG shows a normal alpha rhythm.
Differential diagnosis should be made with nocturnal paroxysmal states of epileptic and non-epileptic origin. For the differential diagnosis of nightmares and epileptic paroxysms of frontotemporal localization, it is necessary to conduct an EEG study, which allows us to identify patterns typical of epilepsy. It is extremely difficult to clearly distinguish between nightmares and somnambulism. The transformation of nightmares into somnambulism, and vice versa, is often noted (Kales et al, 1980).
When differentially diagnosing nightmares with alpine slumbers, one should take into account the time of occurrence of paroxysms and some character traits. Alpine naps usually occur in the last third of the night, and the accompanying vegetative symptoms are moderate. During alpine slumbers, in comparison with nightmares, orientation is quickly restored in the post-attack period. It should also be noted that in some cases, patients with alpine drowsiness remember their night attacks.
Differential diagnosis should also be made with hypnoygic hallucinations in narcolepsy. However, unlike nightmares, hypnagogic hallucinations in narcolepsy occur during REM sleep.
Treatment. Benzodiazepines and tricyclic antidepressants have a satisfactory effect. Sometimes an evening dose of anti-depressants and antipsychotics is sufficient (Flemenbaum, 1976). Improved sleep hygiene is also necessary (Hauri, 1982).
Sleep disorders associated with disruption of the transition from sleep to wakefulness
Sleep disorders associated with disruption of the transition from sleep to wakefulness are a group of pathological conditions characterized by sleep disturbances as a result of rhythmic movements, startling when falling asleep, somnilokia, and calf muscle cramps.
Rhythmic movement sleep disorders (Nighttime rhythmic head shaking ICSD 3073)
Clinical characteristics. The main symptoms occur in the first 2 years of life. Stereotyped movements of the head and neck are typical, occurring immediately before falling asleep and persisting during light sleep
(Thorpy, Glovinsky, 1989). Various types of stereotypical movements are noted - head impacts, rotation, swinging to the sides, rolling the body. In adolescence, these disorders are sometimes observed in autism, minimal brain dysfunction, and “borderline” mental disorders (Snyder, 1987).
Data from laboratory and functional studies. A polysomnographic study records normal bioelectrical activity. There are no epileptic patterns.
Treatment. Effective therapy to correct these disorders has not been developed (Watanabe et al., 1980).
Jerks on falling asleep (ICSD 30747.2)
Clinical characteristics. Sudden short-term contractions of the muscles of the arms, legs, and sometimes the head that occur when falling asleep are typical. In this case, patients often experience sensations of falling, hypnagogic drowsiness, and illusions. These changes are not pathological and are observed in 60-70% of healthy people. In some cases, startles lead to partial awakening, which may interfere with falling asleep.
Data from laboratory and functional studies. A polysomnographic study reveals short, high-amplitude muscle twitches (myoclonus) at the moment of falling asleep, and partial awakenings (Broughton, 1988).
Differential diagnosis should be made with myoclonic epileptic syndromes and restless legs syndrome. It is also necessary to exclude organic and psychiatric diseases accompanied by similar symptoms.
Treatment. Benzodiazepines and L-DOPA preparations have a satisfactory effect. However, this therapy is indicated only for sleep disorders (Lund, Clarenbach, 1992).
Somnilokia (ICSD 307-47.3)
Clinical characteristics. The main clinical signs are sleep-speaking and screaming in sleep, which can be repeated several times during the night. Patients do not remember any episodes of sleep talk. Provoking factors are fever and stress. At the same time, other sleep disorders may occur, for example, somnambulism, nightmares, sleep apnea syndrome.
Data from laboratory and functional studies. Somnilokia can occur at any stage of sleep, but most often during REM sleep.
Differential diagnosis must be made with nocturnal paroxysms of both epileptic and non-epileptic origin, accompanied by verbalization. Treatment. No special therapy is required.
Nocturnal calf cramps (ICSD 729.82)
Clinical characteristics. Night cramps of the calf muscles are observed in children and adults. Familial cases have been described (Jacobsen et al, 1986). Typical are paroxysms of sudden awakening, accompanied by intense pain in the calf muscles. The attack continues for 30 minutes, then suddenly passes. Often, such paroxysms can be secondary and occur in a wide range of diseases: Parkinson’s disease, rheumatism, endocrine, neuromuscular and metabolic diseases.
Data from laboratory and functional studies. A polysomnographic EMG study reveals increased activity of the affected muscles.
Treatment. During an attack, calf massage, movement, warming are recommended (Saskin el A1, 1988), and sometimes taking magnesium and iron supplements (Lund, Claren-bach, 1992).
Parasomnias that occur during RKM sleep
Parasomnias that occur during the REM sleep phase include the following pathological conditions - alpine naps, sleep paralysis, REM sleep-dependent asystoles, behavior disorders in REM sleep.
Alpine Slumbers (ICSD 307.470)
Clinical characteristics. Alpine naps occur at the age of 3-5 years in ordinary children. Girls are more often affected (Kramer, 1979). Typical are sudden awakening, accompanied by severe fright, fear, and a feeling of threatening danger. Episodes are observed, as a rule, in the last third of the night. The content of the dream is remembered and can be clearly described. There are a number of factors that provoke the development of alpine naps. In children, alpine naps are most often provoked by psychogenic stress, sleep deprivation, and taking medications that suppress REM-COH (tricyclic antidepressants, MAO inhibitors).
The pathogenesis of alpine naps is not clear enough. In 60% of cases, alpine slumbers are associated with traumatic events in the anamnesis (Kals et al, 1980). Facio et al (1975) described alpine naps in 69% of Vietnam War veterans.
Data from laboratory and functional studies. A polysomnographic study reveals awakening in the REM sleep phase, tachycardia, and tachypnea.
Differential diagnosis should be made primarily with nightmares. Compared to alpine naps, nightmares occur upon awakening during the slow-wave sleep phase. The content of sleep during nightmares is usually fragmentary and not remembered.
Along with nightmares, alpine naps should be differentiated from behavioral disorders during REM sleep, which are characterized by motor phenomena and preservation of muscle tone during the REM sleep phase.
Treatment. In children, alpine naps pass spontaneously. For frequent, at least weekly episodes, psychotherapy is recommended. Among medications, L-DOPA and β-blockers have a positive effect.
Sleep paralysis (ICSD 780.56-2)
Clinical characteristics. Typical episodes of “sleep paralysis” are hypnagogic hallucinations, oneiric states. Both familial (Rushton, 1944) and sporadic cases (Hishikawa, 1976; Meier-Ewert, 1989) have been described.
Data from laboratory and functional studies. A polysomnographic study reveals depression of muscle tone, the beginning of the sleep cycle with the REM sleep phase (sleep onset REM) or fragmented REM sleep.
Differential diagnosis. The range of diseases with which a differential diagnosis should be made is quite wide and includes hysterical states, paroxysmal myoplegia, drop attacks of various etiologies. Treatment. Pathogenetic therapy has not been developed.
Painful erections during sleep (ICSD 780.563)
Clinical characteristics. Paroxysmal pain in the penile area during erection, observed during the REM sleep phase, is characteristic.
REM sleep - dependent asystole (ICSD 780.56-4)
Clinical characteristics. Cardiac arrest during REM sleep. During the day, patients may experience a feeling of heaviness in the chest.
Data from laboratory and functional studies. In a polysomnographic study during the REM sleep phase, asystoles lasting up to 2.5 seconds are noted (Guilleminault et al, 1984).
REM sleep behavior disorders (ICSD 780.59-0)
Clinical characteristics. The age of onset of the disease is variable, although there is a tendency for the disease to predominately occur in adults and even the elderly. The most typical symptoms of the disease are paroxysmal episodes of sudden awakening during the REM sleep phase, accompanied by screaming or crying, searching movements, and a feeling of stiffness. Sometimes attacks become more complex: patients jump out of bed, rush around the room, and in some cases leave the house. Often the behavior is aggressive. During the day, no naroxysmal disorders were observed. Both symptomatic and idiopathic forms have been described (Uchiyama et al, 1995). A symptom complex of behavioral disorders during REM sleep is often observed in some neurological diseases - Shy-Drager syndrome, Parkinson's disease, narcolepsy, encephalomyelitis, cerebral astrocytoma. It is also possible that this symptom complex may develop when taking alcohol or a number of medications (imipramine, amphetamine).
The pathogenesis is not clear enough. The relationship between the genesis of the disease and biochemical disorders in the metabolism of adrenaline and norepinephrine is discussed.
Data from laboratory and functional studies. A polysomnographic study 60-90 minutes after falling asleep during the REM sleep phase reveals increased motor activity. In this case, muscle tone, as a rule, does not change. There is also an increase in deep sleep and an increase in REM sleep phases. There are no associated autonomic reactions. After an attack, the patient can be quite easily awakened (Shondienst, 1995).
Differential diagnosis should be made with nightmares, somnambulism, epileptic paroxysms of frontal and temporal localization. Compared to behavior disorders during REM sleep, nightmares and somnambulism are observed mainly in children during the slow-wave sleep phase. Behavioral disorder during REM sleep differs from epileptic paroxysms in the “coupling” with REM-CHOM, the absence of an aura, impaired consciousness, and motor stereotypies.
Treatment. Clonazepam has a satisfactory effect.
Other parasomnias
According to the International Classification of Sleep Disorders, this group includes the following diseases and pathological conditions - bruxism, nocturnal enuresis, abnormal swallowing syndrome associated with sleep, nocturnal paroxysmal dystonia, sudden nocturnal death syndrome, including in children, lethal familial insomnia, primary snoring , sleep apnea in children, congenital central hypoventilation syndrome, benign myoclonus of newborns during sleep.
Bruxism (ICSD 306.8)
Clinical characteristics. The main symptoms are stereotypical teeth grinding and biting teeth during sleep. In the morning, the patient often complains of pain in the facial muscles, jaw joints, and pain in the neck (Lavigne et al, 1991). An objective examination often reveals abnormal teeth, malocclusion, and inflammation of the gums. According to the literature, about 90% of the population have had an episode of bruxism at least once in their lives, but only 5% have symptoms so severe that they require therapy. Provoking or trigger factors are often dental prosthetics and stress (Pingitore et al, 1991). Familial cases of bruxism have been described.
Data from laboratory and functional studies. A polysomnographic EMG study reveals increased activity of the jaw muscles, which is combined with the appearance of K-complexes and partial awakening. Bruxism occurs both during non-REM and REM sleep (Ware and Rugh, 1988).
Differential diagnosis. Diagnosis and differential diagnosis of bruxism usually does not present any difficulties (Glares, Rao, 1977). In some cases, the diagnosis of bruxism is mistakenly made in patients with epileptic paroxysms, who experience tongue bite during night attacks. The diagnosis of bruxism is supported by the lack of tongue bite and severe wear and tear of the teeth.
Treatment. The use of biofeedback methods is being discussed (Glares, Rao, 1977; Punch, Gale, 1980).
Nocturnal enuresis (ICSD 780.56-0)
Clinical characteristics. Nocturnal enuresis is repeated involuntary urination during sleep. There are primary and secondary nocturnal enuresis. With primary enuresis, urinary control is not acquired. With secondary enuresis, acquired control over urination is lost. Approximately 15% of boys and 10% of girls suffer from primary enuresis. Primary enuresis usually goes away on its own at puberty. Sometimes primary enuresis is combined with somnambulism and nightmares.
Data from laboratory and functional studies. A polysomnographic study reveals an increase in the duration of deep sleep. During non-REM sleep III-IV, non-specific body movements are noted; when sleep phases change, urination occurs, followed by a decrease in muscle tone (Mikkelsen et al, 1980).
Differential diagnosis. In differential diagnosis, it is necessary to exclude diseases such as diabetes mellitus and urinary tract infections (Mikkelsen, Rappaport, 1980; Schmitt, 1982).
Treatment. It is recommended to limit fluid intake in the evening. Among drugs, antidepressants, in particular imipramine, have a satisfactory effect (Mikkelsen et al, 1980). For enuresis caused by a urinary tract infection, the underlying disease should be treated. Automotive training and wearing special trousers with a built-in sound device during the day are also recommended. When urinating, the sound device is activated (De Leon and Sacks, 1972).
Abnormal Swallowing Syndrome Associated with Sleep (ICSD 780.566)
Clinical characteristics. The main manifestations are excessive, frequent swallowing movements, which contribute to coughing and a feeling of suffocation. Often the attack ends with awakening. Fear of another attack can cause another attack.
Data from laboratory and functional studies. Polysomnographic studies show an increased incidence of incomplete awakenings (Guilleminault et al, 1976).
Differential diagnosis. The most difficult differential diagnosis is bronchial asthma. Anamnestic information about the presence of allergic disorders is informative.
Hypnogenic paroxysmal dystonia (ICSD 780.59-1)
Clinical characteristics. Hypnogenic paroxysmal dystonia is a rare variant of paroxysmal dystonia (Lugaresi, Cirignotta, 1981). It occurs exclusively during the non-REM sleep stage and is triggered by awakening. Characteristic attacks are accompanied by choreoathetoid, ballistic movements and/or dyskinesias. The duration of attacks varies from several seconds to several minutes. Consciousness is always preserved. Familial cases have been described (Lee et al, 1985). Epilepsy is common in the pedigree (Sellal and Hirsch, 1991).
Data from laboratory and functional studies. A polysomnographic study reveals a disturbance in the sleep profile; multiple motor artifacts are recorded at the time of the attack. A number of researchers have discovered typical epileptic patterns when using depth electrodes in the frontotemporal areas (Mierkord et al, 1992). The question of the epileptic genesis of hypnogenic paroxysmal dystonia is debatable. Differential diagnosis should be made with pseudoepileptic (psychogenic) paroxysms, as well as with epileptic seizures of frontal and temporal localization. Pseudoepileptic paroxysms, in comparison with hypnogenic paroxysmal dystonia, are characterized by a longer duration of attacks, the presence of psychopathological character traits, and the absence of stereotypies.
In epileptic seizures of frontal and temporal localization, in contrast to hypnogenic paroxysmal dystonia, a disturbance of consciousness is often observed, and epileptic EEG patterns are also recorded.
Treatment. Clonazepam and carbamazepine have a satisfactory effect (Blank et al, 1993).
Sudden nocturnal death syndrome (ICSD 780.59-3)
Clinical characteristics. The syndrome is observed predominantly in young people, mainly of South Asian origin. Often these patients have a history of nightmares. The episode can occur at any stage of sleep and manifests itself with an attack of sudden suffocation, dyspnea. Attempts to wake the patient are unsuccessful. After resuscitation, ventricular flutter is determined. In the deceased patients, no changes were found in the heart that could explain sudden death.
Data from laboratory and functional studies. In a polysomographic study, pathology is not determined (Cobb et al, 1984; Lown, 1987).
Pediatric sleep apnea (ICSD 770.80)
Clinical characteristics. The term “childhood sleep apnea” refers to central or obstructive sleep apnea observed in children. There are 4 variants of this syndrome: apnea in prematurity, apparent life-threatening event, apnea in early childhood, obstructive sleep apnea syndrome.
Premature infants, especially those born before 37 weeks of gestation, have severe immaturity of the respiratory system. In this regard, this group of children often experience episodes of apnea during sleep. The occurrence of apnea in newborns is also due to decreased sensitivity to carbon dioxide. A risk factor for apnea in prematurity is gestational age. 50-80% of preterm infants born at 31 weeks of gestation have episodes of sleep apnea (Henderson Smart, 1985). In the development of an “obvious life-threatening episode” and apnea in young children, a decisive role is played by insufficient maturity of the central regulation of breathing (Brazy et al, 1987). Episodes of apnea in young children can be provoked by factors such as sudden tilting of the head, feeding, vomiting, and painful external stimuli.
Apnea in children manifests itself during sleep and is characterized by signs of hypoventilation (pallor of the skin or cyanosis, muscle hypotension). With frequently recurring episodes of apnea in children, hypertension of the pulmonary arterioles, right ventricular hypertrophy, and, in some cases, increased erythropoiesis in the liver may develop (Naeye, 1980).
Diagnosing sleep apnea in children is difficult. Compared to adults with sleep apnea, children do not have symptoms such as snoring or daytime fatigue.
Data from laboratory and functional studies. During a polysomnographic study, episodes of apnea are recorded, including a central phase lasting up to 20 seconds and an obstructive phase lasting about 10 seconds. Bradycardia and decreased oxygen saturation are also noted.
Treatment. Pathogenetic therapy has not been developed.
Congenital central hypoventilation syndrome (ICSD 770.81)
Clinical characteristics. From birth, shallow breathing is detected during sleep, sometimes with episodes of apnea (Fleming, 1980). Subsequently, due to dysmetabolic disorders caused by impaired respiratory function (hypoxia, hypercapnia), pulmonary hypertension, cor pulmonale, and brain hypoxia develop (Paton el al, 1989). As the disease progresses, cyanosis, generalized hypotension, and hyporeflexia occur. The prognosis is unfavorable.
Data from laboratory and functional studies. A polysomnographic study reveals decreased respiratory function against the background of hypercapnia and hypoxia. Sometimes episodes of apnea are recorded.
Treatment. Oxygen administration is recommended (Schlake el A1, 1991).
Sudden infant death syndrome (ICSD 798.0)
Frequency. 1 4:1000 births die as a result of sudden death (Byard, 1991). Sudden infant death syndrome most often occurs in children in the first year of life; 40% of all deaths in the first year of life are due to sudden infant death syndrome. After 3 months of life, the risk of developing sudden death syndrome decreases (Harrison, 1991).
The pathogenesis of sudden death syndrome is unclear. The role of dysfunction of brain stem structures is discussed (Stumer et al, 1990; Takahashima, Becker, 1991; Kinney et al, 1991). A number of researchers point to the significance of changes in cardiac function - prolongation of the QT interval, asymmetry in the maturation of sympathetic innervation of the right and left parts of the heart (Schwartz et al, 1982), reduced heart response to changes in heart rate in the QT phase (Sadeh et al, 1987). In the genesis of sudden death syndrome, according to James et al (1990), gastroesophageal reflux, intoxication, infections, incompetence of the immune system, hyperthermia due to high temperature in the room or excessively warm clothing may also play a role. The following risk factors for the development of sudden death syndrome in children have been identified (Hoppenbrouwers, Hodgman, 1982):
- prematurity (especially <1500 g);
- twins or triplets;
- the presence of sudden death syndrome in childhood among relatives;
- short intervals between births;
- smoking or maternal drug use (opiates, cocaine).
Socioeconomic factors also play a certain role, which undoubtedly positively correlate with the risk of sudden infant death syndrome. Lying on the baby's stomach also appears to be a risk factor. It has been noted that in southern Australia and the Netherlands, where children lie on their stomachs less, the risk of developing sudden death syndrome is lower.
Treatment. It is necessary to target and monitor children at risk. For respiratory motility disorders, breathing exercises are recommended. Avoid lying on the baby's stomach for long periods of time. For respiratory disorders, it is advisable to prescribe theophylline, and for hyperexcitability, phenobarbital.
Benign sleep myoclonus in newborns (ICSD 780.59-5)
Clinical characteristics. Debut - in early childhood. Asynchronous twitching of the limbs and trunk is typical during quiet sleep (Coulter, Alien, 1989).
Data from laboratory and functional studies. In a polysomnographic study, short (40-300 ms) asynchronous myoclonus is recorded (Resnick et al, 1986).
Lethal familial insomnia (ICSD 337.9)
Clinical characteristics. The age of onset is variable. Progressive insomnia is typical, starting with difficulty falling asleep, which after a few months leads to complete loss of sleep. Objectively, autonomic disorders are significantly pronounced - hypersalivation, anhidrosis, cardiopulmonary dysfunction. The disease progresses rapidly, after 2 years a coma develops, and patients die.
Data from laboratory and functional studies. A polysomnographic study reveals the absence of deep sleep and/or dissociated REM sleep, myoclonus.
Treatment is symptomatic.
<< Return to top
Prevention of the syndrome
You can prevent cardiac arrest during sleep by avoiding negative provoking factors that affect blood circulation. For people with heart disease, no less important than regularly taking cardiac pills are regular walks in the fresh air, drinking enough clean water, giving up alcohol and smoking, and a balanced diet.
The use of drugs to normalize heart rhythm is possible only under pulse control. We must also remember about a possible overdose. The patient should learn to independently determine and count the pulse; it is important to follow the doctor’s recommendations regarding the dosage and duration of taking medications.
Unfortunately, the decisive factor in sudden cardiac arrest during sleep is the speed of first aid. But it has not yet been possible to achieve complete and effective resuscitation measures at home.