Heart failure is associated with decreased heart function. The heart muscle cannot produce the energy needed to pump the required amount of blood throughout the body.
In Russia alone, about 7 million people suffer from heart failure. In people over 70, one in four people are affected, with men typically affected at a much younger age than women. The risk for men is approximately one and a half times higher than for women. In Russia, diseases of the circulatory system are the most common cause of death.
- What is heart failure?
- What causes heart failure?
- What are the types of heart failure and what are their symptoms? Left-sided heart failure
- Right-sided heart failure
- Global heart failure
- Systolic heart failure
- Diastolic heart failure
- Chronic heart failure
- Acute heart failure
What is heart failure?
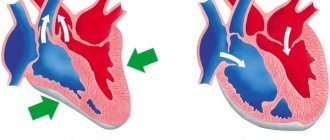
With a healthy heart, oxygen-rich blood from the left ventricle is pumped through the body to the organs, providing them with oxygen and nutrients. After supplying the organs, low-oxygen blood returns from the body to the right side of the heart, from where it is transported to the lungs. In the lungs, the blood is enriched with oxygen so that it can again be pumped throughout the body through the left ventricle.
Heart failure is a weakening of the pumping function of the heart. Typically, either the right side of the heart is affected (right-sided heart failure) or the left side of the heart (left-sided heart failure). With advanced heart failure, both sides of the heart can be affected (global heart failure). Heart failure can also be chronic or acute in nature. Chronic heart failure is more common than acute heart failure, which occurs suddenly and unexpectedly. Acute heart failure can occur suddenly against the background of an acute cardiovascular accident and/or decompensated heart failure.
Treatment
First medical aid for AHF directly depends on the type of pathology.
Fainting
First aid for fainting
As a rule, treatment of fainting occurs without the use of medications.
Emergency care for fainting type of fainting consists of the following actions:
- place the patient in a horizontal position with the leg end raised;
- unbutton the buttons of your shirt and free yourself from clothing that is constricting your chest;
- provide access to fresh cool air;
- Spray your face with water or wipe your forehead and cheeks with a wet cloth;
- give warm sweet tea or weak coffee to drink if the patient is conscious;
- in the absence of consciousness, pat your cheeks and apply cold to your temples.
Cup of hot sweet coffee
If the above actions are ineffective, you can inject vasoconstrictor drugs, for example, Cordiamin.
Collapse
The woman in the photo suddenly felt ill
First aid for collapse is aimed at eliminating the causes that provoked the development of this condition. First aid for collapse consists of immediately placing the patient in a horizontal position, raising the leg end and warming the patient.
If the person is conscious, then you can give him hot sweet tea. Before transport to the hospital, the patient is given an injection of a vasoconstrictor drug.
Syringe for intravenous injection
In a hospital setting, the patient is administered medications that eliminate both the symptoms of vascular insufficiency and the causes of this pathological condition:
- drugs that stimulate the respiratory and cardiovascular centers - these drugs increase the tone of the arteries and increase the stroke volume of the heart;
- vasoconstrictors - adrenaline, Dopamine, Norepinephrine and other drugs that quickly increase blood pressure and stimulate the heart are administered intravenously;
- infusion of blood and red blood cells - required in case of blood loss to prevent shock;
- carrying out detoxification therapy - droppers and solutions are prescribed that quickly remove toxic substances from the blood and replenish the volume of circulating fluid;
- Oxygen therapy – prescribed to improve metabolic processes in the body and saturate the blood with oxygen.
Possible nursing problems with AHF of the collapse type are the difficulty of giving the patient something to drink if his consciousness is impaired, and of administering the drug intravenously at low pressure - it is not always possible to immediately find a vein and get into the vessel.
Important! Saline solutions are not effective if the collapse is caused by the deposition of blood into the intercellular space and internal organs. In such a situation, to improve the patient's condition, it is necessary to inject colloidal solutions into the plasma.
Shock
Treatment of shock consists of taking measures aimed at improving the systemic functions of the body and eliminating the causes of this condition.
The patient is prescribed:
- painkillers – in case of injuries and burns, before carrying out any actions, it is necessary to administer painkillers to the patient, which will help prevent the development of shock or stop it in the erectile stage;
- oxygen therapy – the patient is given humidified oxygen through a mask to saturate the blood with oxygen and normalize the functioning of vital organs; if consciousness is depressed, the patient is given artificial ventilation;
- normalization of hemodynamics - medications are administered that improve blood circulation, for example, red blood cells, colloidal solutions, saline solutions, glucose and others;
- administration of hormonal drugs - these drugs help to quickly restore blood pressure, improve hemodynamics, and relieve acute allergic reactions;
- diuretics - prescribed for the prevention and elimination of edema.
Important! With the development of AHF, all medications should be administered intravenously, since due to impaired microcirculation of tissues and internal organs, the absorption of medications into the systemic bloodstream changes.
What are the types of heart failure and what are their symptoms?
Each type of heart failure has different symptoms, and the symptoms can vary in intensity. However, the main symptom of heart failure is difficulty breathing during exercise or at rest. Warning signs may include sweating with mild exercise, an inability to lie flat, tightness in the chest, or swelling in the legs.
Left-sided heart failure
The left side of the heart is responsible for pumping oxygen-rich blood throughout the body to the organs. In left-sided heart failure, the pumping function of the left ventricle is limited, resulting in insufficient oxygenated blood to be pumped throughout the body. Instead, the blood remains in the pulmonary circulation, which can lead to fluid in the lungs (pulmonary edema), difficulty breathing, throat irritation, a rattling sound when breathing, weakness, or dizziness.
It is most often caused by coronary artery disease (CHD), high blood pressure or a heart attack, and less commonly by problems with the heart muscle or heart valves.
Left-sided heart failure may present acutely or develop over time. It is usually first noticed by shortness of breath from physical activity. When severe, it can even lead to hypotension (low blood pressure) at rest.
Right-sided heart failure
The right side of the heart is responsible for returning low-oxygen blood back to the lungs. In right-sided heart failure, the right ventricle does not work properly. This causes increased pressure in the veins, forcing fluid into the surrounding tissue. This leads to swelling, especially in the feet, toes, ankles and legs. This can also lead to an urgent need to urinate at night when the kidneys receive better blood circulation.
The cause is most often an acute or chronic increase in pulmonary circulatory resistance. Caused by pulmonary diseases such as pulmonary embolism, asthma, severe emphysema, chronic obstructive pulmonary disease (COPD, most commonly due to tobacco use), or left-sided heart failure. Rare causes include heart valve problems or heart muscle disease.
Global heart failure
When both the left and right sides of the heart are affected, it is called global heart failure. There are symptoms of left and right heart failure.
Systolic and diastolic heart failure
Systolic heart failure is associated with loss of normal functioning of heart muscle cells or external impairment of pumping function. Blood enters the lungs, and the organs do not receive enough oxygen.
In diastolic heart failure, the elasticity of the ventricle is lost, causing it to not relax and fill appropriately. One of the most common causes of diastolic dysfunction is high blood pressure. Due to increased resistance in the arteries, the heart must work harder. The elasticity of the heart muscle decreases, and less blood can be pumped from the ventricles to the body between contractions. This results in the body not receiving enough blood and nutrients.
Heart valve disease can also cause the heart muscle to thicken. The heart muscles become stiffer and less elastic due to the accumulation of proteins. Symptoms range from cough to shortness of breath.
Chronic and acute heart failure
Chronic heart failure is a progressive disease that takes months or years to develop and is more common than acute heart failure. In chronic heart failure, symptoms are often not taken seriously because the body is able to compensate over a long period of time or symptoms are associated with increasing age. Symptoms reflect either left- or right-sided heart failure.
Acute heart failure occurs suddenly, minutes or hours after a heart attack, when the body can no longer compensate. Some symptoms include:
- severe difficulty breathing and/or coughing;
- Gurgling sound when breathing;
- Heart rhythm disturbances;
- Pallor;
- Cold sweat.
Clinical manifestations
The syndrome usually develops suddenly
The clinical picture of AHF is always accompanied by a decrease in blood pressure and directly depends on the severity of the condition; this is presented in more detail in the table.
Table 1. Clinical forms of pathology
| Name | How does it manifest clinically? |
| Fainting woman fainting | The patient suddenly feels weak, dizzy, and has “floaters” flashing before his eyes. Consciousness may be preserved or absent. If after 5 minutes the patient does not come to his senses, then fainting is accompanied by convulsions; as a rule, this rarely happens and with properly organized help the person’s condition quickly normalizes |
| Collapse Retardation during collapse | This condition is much more severe than fainting. The patient's consciousness can be preserved, but there is severe inhibition and disorientation in space. Blood pressure is sharply reduced, the pulse is weak and thready, breathing is shallow and rapid. The skin is pale, acrocyanosis and sticky cold sweat are observed. |
Shock State of shock | Clinically, shock is not much different from collapse, but in this condition a sharp depression of the heart and other vital organs develops. Due to severe hypoxia, the brain suffers, against the background of which degenerative changes can develop in its structure |
What classes is heart failure divided into?
There are several classifications of heart failure:
- Classification according to V. Kh. Vasilenko, N. D. Strazhesko, G. F. Lang;
- Classification of acute heart failure according to the Killip scale;
- And the most common is the New York Heart Association classification.
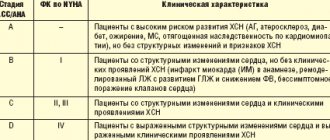
According to the New York Heart Association (NYHA) functional classification, heart failure is classified into classes I-IV depending on the severity of symptoms and limitation of physical activity.
Heart failure is divided into four classes depending on the severity of symptoms:
- NYHA I: heart disease without any restrictions on physical activity. Normal activity does not cause increased fatigue, palpitations, or difficulty breathing.
- NYHA II: Heart disease causing moderate limitation in daily activities. No symptoms at rest.
- NYHA III: Heart disease causing marked limitation in daily activities. Simple activities such as brushing your teeth, eating, or talking cause fatigue, palpitations, or difficulty breathing. There are no symptoms at rest.
- NYHA IV: Heart disease that causes symptoms at rest (and with any degree of light physical activity).
Heart failure significantly reduces quality of life. Patients often experience great frustration with physical limitations and tend to withdraw from social life. For this reason, psychological disorders such as depression are often present in addition to the expected physical symptoms.
Diagnostics
To make a diagnosis, the doctor must perform the following actions and analyze the results of the following studies:
- Collecting anamnesis - what complaints are bothering you, when they appeared, how they change under the influence of stress or medications; presence of concomitant diseases
- Examination – presence of edema, dilated veins on the anterior abdominal wall and neck
- Physical examination - auscultation and percussion of the lungs determines the level of fluid in the pleural cavity without the use of x-rays. Tapping the cardiac borders allows you to assess the size of the heart, especially the right half. Listening to murmurs is necessary to diagnose valve defects and changes in the density and structure of lung tissue.
- General clinical tests - blood for cellular composition, lipids, protein, glucose, bilirubin, coagulogram and others.
- Assessment of blood gas composition - percentage of oxygen and carbon dioxide.
- Study of external respiration function (spirography)
- X-ray of the chest - provides information about the condition of the chest organs
- Electrocardiogram
- ECHO-KG
- Catheterization of the right ventricle to measure pressure in the branches of the pulmonary artery
- Lung biopsy
- CT, MRI of the chest - visualize the size, structure of the heart and its relationship with neighboring organs, as well as the structure of the lungs and the condition of the pleural cavity.
- Angiography of the pulmonary vessels - allows you to evaluate the patency of the arteries by introducing an iodine-containing substance through a catheter under the control of an X-ray machine.
How is heart failure diagnosed?
Diagnosis begins with a comprehensive assessment of a person's medical history, paying particular attention to symptoms (onset, duration, manifestation). This helps classify the severity of the symptom. The heart and lungs are examined. If a heart attack or rhythm disorder is suspected, a 12-lead resting ECG is performed. In addition, echocardiography and complete blood count. The need for catheterization is determined individually.
Prevention measures
At a consultation with a cardiologist
In order to prevent the development of acute vascular insufficiency, it is important to follow the doctor’s recommendations:
- promptly identify and treat diseases of the cardiovascular system;
- do not take any medications without a doctor’s prescription, especially for the treatment of arterial hypertension;
- do not stay in direct sunlight for a long time, in a bathhouse, sauna, especially if there are any disturbances in the functioning of the heart and blood vessels;
- Before a blood transfusion, be sure to take tests to make sure that the donor’s blood matches the group and Rh factor.
Maintaining an active lifestyle, giving up bad habits, and a nutritious and balanced diet will help prevent disorders of the cardiovascular system and blood pressure.
How is heart failure treated?
For chronic heart failure, medications (such as ACE inhibitors, beta blockers and diuretics) are used. Medicines are used to prevent complications and improve quality of life. ACE inhibitors and beta blockers can prolong life, but they must be taken regularly to achieve a beneficial effect.
In addition, rhythm therapy (to treat cardiac arrhythmias) and implantation of a three-chamber pacemaker are used. The latter ensures timely activation of the atria and both ventricles. A defibrillator is also often implanted as part of a pacemaker to counteract dangerous heart rhythm disturbances in the setting of severe heart failure. This treatment is also known as resynchronization therapy. An important part of successful treatment is physical therapy.
conclusions
Not all diseases that lead to the development of cardiopulmonary failure are reversible, but the right treatment can reduce symptoms to a minimum. Lifestyle changes such as regular physical activity, healthy eating, reducing dietary salt, reducing stress and excess weight improve prognosis and quality of life.
The only way to prevent the development of SLN is to control the underlying disease and follow the instructions of the attending physician.