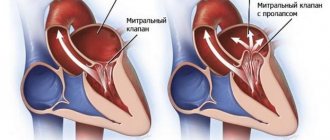
Heart failure (HF) is a pathological condition caused by the failure of the heart as a pump that provides adequate blood circulation. Manifestation and consequence of pathological conditions affecting the myocardium or complicating the work of the heart: coronary heart disease, heart defects, arterial hypertension, diffuse lung diseases, myocarditis, myocardial dystrophy (including thyrotoxic, sports, etc.), myocardiopathy (including alcoholic) and etc.
Acute heart failure can be either acute itself, or it can be an acute manifestation of chronic heart failure.
What it is
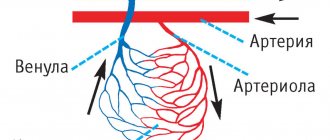
Coronary insufficiency (CI) is a condition in which blood flow through the coronary (coronary) arteries does not meet the energy needs of the heart. In this case, myocardial ischemia occurs - damage to heart cells due to lack of oxygen and nutrients. Ischemia is a local process that occurs in the place of the myocardium (heart muscle) where its nutrition has been disrupted. The process of deterioration of blood flow itself is most often explained by a narrowing of the lumen of the blood-bearing vessel. Globally this can happen for 2 reasons:
- obstruction (blockage) of the artery lumen;
- spasm due to contraction of the vessel walls.
A combination of these reasons is also possible.
In this case, a person cannot notice any changes in his condition until the level of stenosis (narrowing of the lumen of the artery) reaches critical values. Or until the need of the heart for nutrition makes the stenosis significant. When these conditions are met, ischemia develops in the area of the heart muscle—an attack of angina, myocardial infarction, or even sudden cardiac death occurs. Thus, we can say that clinically coronary insufficiency manifests itself in various forms of coronary heart disease (CHD).
According to research, the number of patients with coronary artery disease in Russia exceeds 7.5 million people - this is a very high figure. Moreover, the prevalence among people of retirement age is 16% higher than among people of working age. That is, the incidence of the disease progresses with age. Men get sick earlier and more often than women.
Sudden cardiac death and its prevention
Coronary death
Coronary death refers to death that occurs as a result of the cessation of effective heart function. As a rule, in this case, either ventricular fibrillation or primary cardiac arrest develops. In almost 90% of cases, acute coronary death is caused by coronary heart disease. It also happens that before this, IHD did not manifest itself in any way, that is, it was asymptomatic. In some cases, the patient was bothered by angina attacks and arrhythmia. After a heart attack, the risk of sudden death increases several times.
Manifestations and course of coronary death
Autopsies of patients who died suddenly usually reveal damage to the coronary arteries by atherosclerotic plaques. In this case, the lumen of the vessel narrows by 70% or more. Very often, on the damaged surface of the vessel there is a thrombus that has completely stopped blood flow in a fairly large area of the heart muscle. Usually, signs of myocardial infarction cannot be identified, since too little time has passed since the onset of the disease. Histological examination can reveal signs of incipient necrosis and cell restructuring.
Due to electrical instability of the myocardium, life-threatening arrhythmia occurs (asystole or ventricular fibrillation). Blood flow stops, including through the cerebral arteries. In this regard, the person quickly loses consciousness and falls. Noisy wheezing breathing and foam at the mouth may appear. After a few minutes, the muscles will begin to twitch involuntarily. The skin becomes pale, cyanosis of the lips and limbs is observed. The pulse and breathing stop completely, the pupils dilate and stop responding to light.
Help with cardiac death
Sudden coronary death leads to irreversible changes in the cerebral cortex within 5-6 minutes. Therefore, emergency measures to restore blood flow must begin immediately and continue until the arrival of the medical team.
Every person needs to know the basics of cardiopulmonary resuscitation. Her tasks include checking and, if necessary, restoring the patency of the airways, starting artificial ventilation (mouth-to-mouth, mouth-to-nose), and chest compressions. According to the latest recommendations, a person without experience can skip the first two points and immediately begin cardiac massage. Several studies have shown that this approach is more effective and leads to improved survival.
Indirect cardiac massage should be performed as follows:
- Place the person on their back on a hard surface;
- Place your palms on the middle third of the sternum perpendicular to it;
- Start squeezing your chest without bending your elbows;
- In this case, the sternum should bend by 5 cm, and the frequency of movements should be about 100 per minute.
The effectiveness of resuscitation measures can be judged by the color of the skin.
Prevention of sudden coronary death
To prevent cardiac death, it is necessary to influence the main provoking factors, among which the most important are:
- Myocardial ischemia;
- Decrease in left ventricular ejection fraction;
- Various arrhythmias.
To eliminate oxygen starvation of the heart, adequate drug therapy is necessary, including the main classes of drugs to improve coronary blood flow (nitroglycerin, beta blockers, aspirin, statins).
If necessary, endovascular restoration of artery patency should be performed. A special balloon is inserted into the affected area through a puncture in the femoral artery, inflated, and then a spring (stent) is installed, which prevents further narrowing of the vessel.
If such an operation cannot be performed for any reason, coronary artery bypass grafting is performed with opening of the chest and connection to a heart-lung machine. In this case, additional vessels (the person’s own arteries and veins, taken from an arm or leg) are sewn from the aorta to the coronary arteries. Recovery after this operation is longer, but the prognosis is favorable.
If myocardial contractility decreases, special devices can be installed to increase it. Special medications, such as digoxin, are also prescribed.
To prevent arrhythmia, in particular ventricular fibrillation, a cardioverter-defibrillator is installed. It is a miniature device that is placed under the skin in the chest area. Using special wires, it is connected to the myocardium and, if an arrhythmia occurs, it restarts the heart using a discharge. It should be remembered that with asystole this device will be ineffective.
Unfortunately, coronary death is a rather insidious disease, and it is not always possible to identify potential patients. That is why the most important thing in the fight against this condition is the timely implementation of emergency measures. Nowadays, many public places have defibrillators that can be used for life-threatening arrhythmias. They also often conduct special courses on teaching resuscitation measures to ordinary citizens.
RISK FACTORS FOR SUDDEN DEATH
Sudden cessation of blood circulation (“cardiac arrest”, clinical death) occurs most often as a result of diseases of the cardiovascular system. The cessation of blood circulation leads to the death of cells in the cerebral cortex, which cannot exist without a constant supply of oxygen for more than 5 minutes. The time frame originally used to describe sudden death was 24 hours. Now they have been reduced to 1 hour.
The risk factors for sudden death are essentially the same as for coronary heart disease.
1. Arterial hypertension and left ventricular hypertrophy
First of all, left ventricular hypertrophy. The risk of sudden death increases with increasing myocardial mass.
2. Lipids
The connection between high cholesterol levels and the risk of sudden death is well established and proven, although there is no reliable data on reducing this risk when lipid levels are normalized.
3. Nutritional features
Most epidemiological studies have not found a clear association between the risk of sudden death and any dietary characteristics.
4. Physical activity
The risk of sudden death is higher both in people who do not regularly engage in strenuous exercise and in people with a lack of physical activity.
5. Alcohol addiction
Severe alcohol dependence and especially binge drinking increase the risk of sudden death. However, moderate alcohol consumption reduces the risk of sudden death (30 g of ethanol per day).
6. Heart rate and heart rate variability
An increase in heart rate is an independent risk factor for sudden death. This may be due to a decrease in parasympathetic activity. Heart rate variability is an indicator associated not only with cardiac, but also with non-cardiac causes of death, so its relationship with the risk of sudden death cannot currently be assessed.
7. Smoking
Smoking is an independent risk factor for sudden clinical death and for the development of myocardial infarction. For persons with a history of circulatory arrest, continued smoking after discharge from hospital is also an independent risk factor for repeated sudden circulatory arrest.
8. Diabetes mellitus
To date, there is no convincing evidence that diabetes mellitus is an independent risk factor for sudden death.
9. Changes on the ECG
A large number of studies have noted a clear connection between ECG changes such as ST segment depression and T wave changes with cardiac death in general and sudden death in particular. Prolongation of the QT interval in individuals without heart disease is also an unfavorable prognostic factor for the development of cardiac death. Similar facts have not been proven regarding QT interval dispersion.
10. Genetic basis
Long QT syndrome, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, polymorphic ventricular tachycardia, dilated cardiomyopathy are inherited in a monogenic manner and have a clear predisposition to sudden death.
The cause of sudden death is often ventricular fibrillation (VF) 75-80% and ventricular tachycardia (VT), less often electromechanical dissociation (EMD) and asystole. Circulatory arrest usually occurs at home (2/3 of cases), in men over 50 years of age (3/4 of cases) during the day (8-18 hours).
All risk factors for coronary heart disease
Since in most cases sudden cardiac death is caused by ischemic disease, it is clear that almost all risk factors for coronary heart disease are also risk factors for sudden death. The greatest importance belongs to such factors as old age, arterial hypertension, left ventricular hypertrophy, tobacco smoking, high blood cholesterol, excess body weight, nonspecific electrocardiographic changes. The risk of sudden cardiac death increases especially significantly when several risk factors are combined.
Previous myocardial infarction
Myocardial infarction is an important risk factor for sudden cardiac death. The potential risk of sudden cardiac death in the first 72 hours from the onset of a heart attack ranges from 15 to 20% of cases. The highest risk of sudden cardiac death is observed in patients with myocardial infarction between 3 days and 8 weeks if the course of the disease was complicated by ventricular tachycardia or atrial fibrillation, or if paired, salvo, early ventricular extrasystoles, or repeated episodes of salvo ventricular extrasystoles were recorded. When heart rate is normalized and left ventricular dysfunction is eliminated, the risk of sudden death is sharply reduced.
An unfavorable prognostic factor in the post-infarction period is depression of the ST interval (painless or accompanied by pain) during exercise testing. The combination of subtotal stenosis of one or more coronary arteries, areas of left ventricular dyskinesia (detected by echocardiography) and frequent polytopic ventricular extrasystoles has a poor prognostic value. The risk of sudden death is significantly increased by the presence of a left ventricular aneurysm, its pronounced hypertrophy, as well as ventricular fibrillation that occurred in the acute period of myocardial infarction and was successfully stopped.
Left ventricular myocardial dysfunction
A decrease in the contractile function of the left ventricular myocardium is one of the main risk factors for sudden cardiac death in cardiac patients. A reduction in ejection fraction of less than 40% is considered critical. After the onset of congestive heart failure of various origins, the risk of sudden cardiac death is very high, it can be 35-40% within 5 years.
Left ventricular myocardial hypertrophy
Left ventricular myocardial hypertrophy of any origin significantly predisposes to sudden cardiac death, with fatal arrhythmia being the most common mechanism of death. This is explained by the fact that with myocardial hypertrophy, the kinetics of ions in it is disrupted, there is a pronounced heterogeneity in the medium of propagation of depolarization and repolarization waves in the myocardium, which contributes to the development of ventricular fibrillation and flutter.
“Unreasonable” decrease in exercise tolerance
Usually, the basis for an unreasonable decrease in exercise tolerance is myocardial ischemia, which is also often combined with cardiac arrhythmias. These factors significantly increase the risk of sudden cardiac death.
Previous sudden cardiac death and previous resuscitation
In patients who have survived sudden cardiac death, the risk of recurrence of ventricular fibrillation is very high: up to 25% during the first year and approximately 5% during the second year (N. M. Shevchenko, 1992).
Violation of autonomic regulation of the heart
In case of coronary artery disease, inflammatory myocardial diseases, diabetes mellitus and other diseases, damage to the autonomic nervous system is observed, which causes its dysfunction and leads, in particular, to a decrease in the effects on the heart and an increase in sympathetic activity. Signs of a violation of the autonomic regulation of the heart are an increase in heart rate and a decrease in heart rate variability.
An increase in sympathetic activity significantly increases the risk of sudden cardiac death, especially in the morning, after the patient awakens. Sympathetic stimulation is also promoted by various toxic effects on the myocardium (smoking, alcohol).
REMINDER FOR THE POPULATION
Prevention of Sudden Cardiac Death
The problem of sudden cardiac death (SCD) has remained one of the pressing health problems for many years due to its medical and social significance, as well as its drama. Sudden cardiac death is understood as circulatory arrest that develops suddenly, within an hour from the onset of clinical symptoms. This outcome is unexpected both for doctors and relatives, since the patient is in a stable condition on the eve of the attack. In some people, sudden cardiac death is the first and last manifestation of the disease. What is the reason for such transience of events? Sudden cardiac death in most cases is an arrhythmic death, in which medical care should be provided within the first 5-6 minutes, and in 90% of cases, circulatory arrest during sudden cardiac death occurs outside of a hospital setting.
According to WHO, the incidence of sudden cardiac death is 30 cases per week per 1 million population. To make it easier to imagine the scale of the problem, here are the following figures: in Europe and the USA, about 350,000 people die suddenly every year (this is an entire city of regional significance!), and every 5 minutes in the world one person dies suddenly! Unfortunately, there are no accurate statistics on sudden cardiac death in our country, since such a diagnosis is not included in post-mortem reports. However, given the high morbidity and mortality from cardiovascular diseases in our country, one of the highest in Europe, there is no doubt that we are “leaders” in this matter.
Since, as indicated, resuscitation measures in case of circulatory arrest must be carried out immediately, and in real life are not always feasible, the main approach to solving the problem of sudden cardiac death is its prevention. It should primarily be carried out in individuals at high risk of sudden cardiac death. Among heart diseases, the main cause of sudden cardiac death is coronary heart disease, which accounts for up to 80% of all cases of sudden cardiac death, and especially in patients who have had a myocardial infarction.
The examination program for patients with coronary artery disease should include:
- Consultation with a cardiologist;
- ECG;
- Test with physical activity - treadmill test;
- Echocardiography;
- Daily ECG monitoring with additional options (assessment of heart rate variability, sinus rhythm turbulence, T wave alternans);
- High-resolution ECG with registration of late ventricular potentials.
Recently, the issue of the risk of sudden death in athletes has become relevant. In an analysis of 185 cases of death of athletes in the United States (1985-1995), the main cause was identified as cardiovascular pathology, with hypertrophic cardiomyopathy leading in it (36%). When analyzing medical documentation, more than a third of athletes noted fainting or pre-fainting conditions, or cardiac complaints several months before death.
It is customary to distinguish three main categories of sudden death in athletes:
- 1st: “commotio cordis” syndrome - develops in the event of a strong blow to the heart, followed by a life-threatening arrhythmia;
- 2nd: sudden death in athletes under 30 years of age is usually associated with congenital cardiac pathology (hypertrophic cardiomyopathies, WPW syndrome, Brugada syndrome, etc.);
- 3rd: sudden death in athletes after 30 years of age, when the death is caused by an already acquired pathology, for example, ischemic heart disease.
The examination program for athletes should include:
- Consultation with a cardiologist;
- ECG;
- Echocardiography;
- Test with physical activity - treadmill test;
- Daily ECG monitoring.
In recent years, the development of sudden cardiac death has been identified as a cause such as respiratory arrest during sleep (obstructive apnea syndrome). This syndrome is manifested by snoring, pauses in breathing during sleep, and daytime sleepiness. In contrast to the generally accepted fact that the peak of cardiovascular mortality in the general population occurs in the early morning hours (from 6.00 to 12.00), in patients with obstructive apnea syndrome, the highest incidence of sudden cardiovascular mortality occurs during the night period (from 00.00 to 6.00). Sleep apnea leads to the development of sinus node arrest, AV blockade of various degrees, up to complete transverse block, and also contributes to the development of arterial hypertension, diabetes mellitus, and maintains obesity (obesity is typical for persons with obstructive apnea).
The examination program for patients with obstructive apnea syndrome should include:
- Consultation with a cardiologist;
- Consultation with an otolaryngologist;
- Polysomnography;
- Consultation with an endocrinologist.
To combat this disease, special breathing devices are selected that eliminate sleep apnea and normalize sleep.
I would like to emphasize that persons with so-called risk factors for cardiovascular diseases are also at risk of premature death. These include: smoking, hypertension, high cholesterol, family history of cardiovascular pathology, obesity, diabetes, physical inactivity. These individuals are recommended to undergo examination using scales developed by European cardiologists (see figure), as well as additional tests (homocysteine, myeloperoxidase, C-reactive protein, comprehensive lipid profile, etc.) and calculate the risk of fatal complications in the next 10 years.
About holding Health Day on the topic
“Let’s prevent the risks of sudden death!”
On October 8, 2021, the State Budgetary Institution “Center for Medical Prevention” of the Ministry of Health of the Krasnodar Territory will organize the next Health Day, which is held as part of the Day for the Prevention of Sudden Death and Life-Threatening Aries. Health Day is held with the aim of preventing cardiovascular diseases and promoting the principles of a healthy lifestyle. An indicative Health Day with the participation of regional specialists will be held in the city of Krasnodar. During the Health Day, organized jointly with the city administration and with the participation of the press, diagnostic tests, consultations, lectures, propaganda and festive events will be carried out.
Cardiovascular diseases, mainly sudden cardiac death (SCD), are the leading cause of death in most countries of the world. SCD is the most pressing problem of our time. The mechanisms underlying the development of sudden cardiac death in the vast majority of cases are ventricular tachycardia (VT) and ventricular fibrillation (VF) - 95%, and the remaining 5% are due to bradyarrhythmias and asystole. The main cause of SCD is coronary heart disease.
Sudden cardiac death is one of the pressing problems of our time. Currently, many different studies are being conducted to study this problem. When treating patients with cardiovascular diseases, the main efforts of doctors should be aimed at actively preventing sudden cardiac death with the help of drugs that have maximum effectiveness and safety.
The issue of preventing sudden cardiac arrest is very important, since the correct attitude to one’s own feelings and the complaints of a loved one will in many cases prevent a fatal outcome. As a number of research works show, many people ignore the warning signals sent by their own body. Thus, very often, patients resuscitated after a sudden stop of blood circulation report previous chest pain, attacks of severe weakness, shortness of breath, palpitations and some other symptoms that appeared hours, days or even weeks before the development of the episode. Many patients with diagnosed heart disease report deterioration of their condition prior to cardiac arrest, but the appearance of these symptoms for some reason does not prompt many of them to seek medical help. And this is due, first of all, to the lack of awareness of patients about the symptoms of heart disease and its potential complications and outcomes.
Sudden cardiac death is a rather insidious disease, and it is not always possible to identify potential patients. That is why the most important thing in the fight against this condition is the timely implementation of emergency measures. Nowadays, many public places have defibrillators that can be used for life-threatening arrhythmias. They also often conduct special courses on teaching resuscitation measures to ordinary citizens.
GBUZ "Center for Medical Prevention" of the Ministry of Health of the Krasnodar Territory.
Causes
Coronary insufficiency most often occurs due to obstruction or spasm of the coronary vessels of the heart or their branches. Let's take a closer look at each of these cases, as well as several more rare situations.
The image is a coronary angiography of the heart vessels. Source: Image by Mario Ohibsky from Pixabay
Artery obstruction
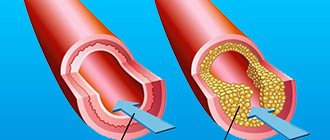
The most important and common cause of coronary insufficiency is atherosclerosis of the coronary arteries. Atherosclerotic plaques protrude into the lumen of the vessel and obstruct blood flow. In this case, chronic coronary insufficiency develops, which most often makes itself felt by attacks of angina pectoris.
Atherosclerotic plaques can also break off or contribute to damage to the inner surface of the vessel and thus provoke thrombosis, which will cause acute coronary insufficiency. Its most common manifestation is myocardial infarction. More information about atherosclerosis can be found here.
Artery spasm
Coronary insufficiency also occurs due to a sharp and prolonged spasm of the coronary arteries. Severe stress, mental and physical overload can lead to this. Often the listed factors complement the existing atherosclerotic lesion of the vessel, which results in angina pectoris or myocardial infarction. However, purely spastic coronary insufficiency is also possible.
Other reasons
There are other, more rare, causes of impaired blood supply to the myocardium:
- Congenital anomalies of the coronary vessels;
- Hypertrophic cardiomyopathy is a condition in which the existing vessels are not enough to meet the needs of the enlarged myocardium (a consequence of hypertension);
- Neoplasms in the chest, compressing blood vessels from the outside (tumor).
Risk factors
Some factors increase the risk of coronary artery disease:
- Male gender and age over 45 years are factors that cannot be adjusted in any way.
- Smoking affects both the development of atherosclerosis and the processes of thrombus formation. Cigarette smoke contains nicotine and carbon monoxide, which have a negative effect on the functioning of the cardiovascular system.
- Low physical activity, a sedentary lifestyle, excess weight and obesity contribute to thrombosis, atherosclerosis, and hypertension, which can lead to coronary insufficiency.
- Eating large amounts of food high in fat and cholesterol contributes to atherosclerosis.
- Chronic stress provokes prolonged spasm of the coronary arteries.
- Heredity - the risk of developing pathology is higher if relatives have it.
Diagnosis of coronary heart failure
In most cases, even after a visual examination of the patient, the doctor may suspect the development of acute coronary insufficiency. But to confirm the diagnosis, it is necessary not only to take into account the totality of clinical signs caused by coronary insufficiency, but also to conduct a diagnostic examination, which includes:
- Complete blood count (the main indicator is an increased number of red blood cells, indicating the presence of an inflammatory process in the body).
- Biochemical blood test (allows us to understand the cause of the disease).
- Blood test for clotting (the consistency of the blood flow and the tendency to thrombosis are studied).
- Coronary angiography (the main diagnostic method aimed at assessing the condition of the coronary arteries).
- X-ray, ultrasound of the chest (allows you to determine whether the patient has other possible diseases of the cardiovascular system and determine the cause of coronary insufficiency).
- Electrocardiography (makes it possible to judge the health of the contractile function of the myocardium and the work of the heart).
- Computed tomography (aimed at identifying stenosis of the coronary arteries, atherosclerotic plaques of different sizes).
- Magnetic resonance imaging of the heart (allows you to take pictures in different planes, measure arterial blood flow, study the filling of the ventricles and atria).
Symptoms
Symptoms of coronary artery disease may vary from case to case. It is also not uncommon for patients to feel nothing strange about their condition until one day, for example, a myocardial infarction occurs.
Among the most characteristic symptoms of coronary insufficiency are:
Angina pain is a pressing, squeezing, burning pain behind the sternum lasting up to 10 minutes. Often appear during physical activity. May begin behind the sternum and then spread to the neck, back, shoulders, arms, jaws;
- Dizziness;
- Cold sweat;
- Pain in the stomach;
- Shortness of breath, especially with exertion;
- Sleep disorders;
- Weakness.
Important! If you notice such symptoms, especially against the background of unusual physical activity, you should immediately call an ambulance. This should also be done if angina has already been diagnosed, but the symptoms are not relieved by nitroglycerin and last longer than 15 minutes.
Source: Pavel Danilyuk: Pexels
The listed symptoms are characteristic of a chronic (reversible) version of coronary insufficiency, which manifests itself as angina pectoris. In the acute (irreversible) version, the described symptoms are more pronounced and last much longer - up to several days (with myocardial infarction). The pain is not relieved by nitroglycerin and can be so severe that it is necessary to resort to narcotic drugs.
Despite the fact that the main symptom of a heart attack is most often severe chest pain (80% of cases), there are other manifestations of the disease:
- Cough and shortness of breath;
- Sharp pain in the upper abdomen;
- Symptoms of brain damage.
An asymptomatic form of myocardial infarction is rare. The area of damage in the heart is not so extensive, and changes are recorded instrumentally after the fact.
Symptoms of chronic and acute coronary heart failure
Among the main signs of coronary insufficiency syndrome:
- cardiopalmus;
- pallor of the skin, the appearance of drops of sweat on the forehead;
- severe pain in the chest, paroxysmal in nature;
- shortness of breath that occurs for unknown reasons;
- chest pain;
- attacks of angina/tachycardia;
- dry cough.
Symptoms worsen after doing physical work, overeating, climbing stairs, emotional experiences (panic, fear). It can also worsen during the resting stage.
Some patients with coronary insufficiency experience:
- nausea;
- vomit;
- frequent urge to urinate;
- flatulence.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Chronic form
A typical manifestation of chronic coronary insufficiency is angina. Most often it is caused by atherosclerotic damage to the coronary arteries of the heart, which causes a narrowing of their lumen. During physical activity, the myocardium requires more blood, while the permeability of the artery is reduced - ischemia occurs with characteristic symptoms.
When attacks are predictable and repeated in response to a load of the same severity, they speak of a stable version of angina. Its course is relatively favorable and can be easily controlled. There are other options:
- Unstable angina is a form of angina in which a plaque in a coronary vessel undergoes ulceration, a thrombus gradually grows in the lumen, causing attacks to constantly progress and ultimately lead to myocardial infarction.
- Prinzmetal's angina (vasospastic angina) - occurs as a result of a sudden spasm of the coronary arteries.
We wrote about angina in more detail here.
Until this point, we were talking mostly about absolute coronary insufficiency, when the direct cause of the pathological condition was pathological processes in the coronary vessels. But there is also a relative form that occurs against the background of hypertrophic cardiomyopathy, which was discussed in the causes of coronary insufficiency. During this process, the myocardium increases in size due to the increased load, while new vessels do not appear. In this case, ischemia of poorly supplied areas also develops.
Coronary insufficiency - what is it?
- Acute coronary heart failure. It is characterized by a discrepancy between the blood flow and the metabolic needs of the myocardium (in parallel, altered coronary arteries of the heart can be diagnosed, angina attacks, severe heart rhythm disturbances, and ECG changes can be observed). The disease, which occurs in an acute manner, often provokes the development of myocardial infarction.
- Chronic coronary insufficiency. It is characterized by prolonged (constant) insufficient blood supply to the myocardium. A prerequisite for the occurrence of pathology is a change in the coronary bed.
Also, coronary heart failure can occur in:
- absolute form (blood flow through the coronary vessels is sharply limited);
- relative form (myocardial oxygen demand increases significantly, but there are no restrictions on coronary blood flow).
Sudden coronary death
Sudden coronary death (SCD) is said to occur when a person dies within no more than 6 hours against the background of apparent well-being due to a cardinal malfunction of the heart. At the same time, the patient loses consciousness and falls.
As a rule, the immediate cause of VCS is ventricular tachycardia and ventricular fibrillation. These are severe rhythm disturbances in which the efficiency of myocardial contraction decreases so much that blood does not flow to vital organs in sufficient volume.
WHO recommends at least 150 minutes of physical activity per week to help reduce the risk of VCS. Source: Mario Ohibsky from Pixabay
However, these arrhythmias are most often preceded by a severe attack of acute coronary insufficiency. Extensive myocardial damage as a result of this attack not only in itself reduces the contractility of the ventricles of the heart, but also contributes to the occurrence of arrhythmias.
Sometimes death can be prevented with timely assistance, but this is more typical for sudden cardiac death of an arrhythmogenic nature. In this case, the developing arrhythmia is of paramount importance, and coronary causes are secondary. Patients with diabetes are at increased risk of VCS.
Important! If you see a person suddenly lose consciousness, you should call an ambulance and, if you have the appropriate skills, perform primary resuscitation measures. Cardiopulmonary resuscitation should be resorted to if you do not detect a pulse and/or breathing in the victim.
Despite this threat in patients with coronary insufficiency, with well-chosen treatment and strict adherence to doctor’s orders, the likelihood of VCS becomes significantly lower. It is also important to seek medical help in a timely manner. It is known that several weeks before an attack, patients sometimes complain of pain in the chest, worsening mood, and fatigue. This means that some treatment measures can be taken before an attack occurs.
Danger of coronary insufficiency
Coronary insufficiency can lead to two life-threatening conditions:
- unstable angina;
- myocardial infarction.
Based on the symptoms of the disease, doctors can determine how high the risk of sudden coronary death (occurs within six hours of the onset of a heart attack) is.
High risk of death if any of the following are present:
- An attack of angina lasts more than 20 minutes.
- Pulmonary edema has developed (the patient constantly stands, breathes heavily, and produces foamy pink sputum).
- The ECG shows reduced or increased ST segment elevation of more than 1 mm above the isoline.
- Angina pectoris, low blood pressure in the arteries.
- According to laboratory tests, there is a change in the level of markers of myocardial necrosis (death).
The average risk of sudden death due to coronary insufficiency is placed if any of the symptoms are observed:
- The attack lasts less than 20 minutes.
- Angina at rest - less than 20, stopped after resorption of Nitroglycerin.
- At night, attacks of chest pain constantly occur.
- The patient's age is over 65 years.
- Severe angina, the first symptoms of which appeared within the last two weeks.
- On the ECG, Q waves are more than 3 mm, dynamic changes in the T wave to normal levels, a decrease in the ST segment at rest.
A low risk of sudden death can be assumed if the following symptoms occur:
- Attacks occur even after simple physical work.
- Recently, the attacks have become more frequent and severe.
- Angina first appeared two weeks to two months ago.
- There are no new changes on the ECG (compared to the results that were obtained previously) or a normal curve for the patient’s age is observed.
Diagnostics
Signs of coronary insufficiency can be suspected independently by detecting symptoms of angina pectoris, although an asymptomatic course up to myocardial infarction is not uncommon.
The following diagnostic methods are used in clinical practice:
- Coronary angiography is the gold standard in diagnosing cardiac vascular pathology; it allows one to visualize narrowing of the lumen in the coronary arteries and their obstruction. The technique is invasive - a catheter for administering a contrast agent is placed through the radial or femoral artery, so the study is performed in the operating room under local anesthesia.
- Optical coherence tomography of the coronary arteries is one of the new and accurate methods for visualizing problem areas in the coronary vessels of the heart. The method is also invasive and is performed in a similar manner to coronary angiography.
- Various types of echocardiography (Echo-CG) allow visualization of areas of the myocardium with impaired contractility, as well as many associated disorders.
- Myocardial scintigraphy - allows you to identify areas of the myocardium with impaired blood circulation, for which special radionuclides are used.
- Stress tests (treadmill test, bicycle ergometry) - procedures allow you to evaluate ECG changes indicating myocardial ischemia during physical activity.
Blood samples are also examined, paying attention to:
- Lipidogram - determination of cholesterol and the ratio of lipids in the blood to identify predisposition to coronary artery disease.
- Blood glucose - to exclude diabetes mellitus.
- Determination of the level of red blood cells and hemoglobin - to exclude iron deficiency anemia.
- Biochemical markers - study the levels of various enzymes that may indicate a heart attack.
Important: elevated blood cholesterol levels can significantly increase the risk of atherosclerotic plaques. They can become one of the causes of coronary insufficiency. Cholesterol may be too high due to a high intake of low-density lipoprotein (LDL) and low intake of high-density lipoprotein (HDL). A nutritionist will help you adjust your diet so that there are more “good”, low-density foods than “bad” foods.
Risk group for the development of cardiac coronary insufficiency
Most often, coronary heart failure is diagnosed in people:
- with a hereditary predisposition;
- with obesity;
- who smoke a lot;
- who have elevated blood cholesterol levels;
- people with diabetes;
- those engaged in sedentary work and leading a sedentary lifestyle;
- suffering from arterial hypertension.
When several risk factors are combined, the likelihood of developing blood clots increases significantly. This means that it is impossible to 100% exclude the occurrence of sudden coronary death in the patient in the future.
Treatment
When prescribing treatment, a cholesterol-lowering diet, moderate regular physical activity and weight loss are first recommended. If you have bad habits, you need to get rid of them. This is called lifestyle modification. Do not underestimate the benefits of such recommendations; in this case, they largely determine the success of treatment and the prevention of future complications.
Source: Michal Jarmoluk from Pixabay
List of sources
- Ageev F.T. , Skvortsov A.A. , Mareev V.Yu., Belenkov Yu.N. “Heart failure against the background of coronary heart disease: some issues of epidemiology, pathogenesis and treatment,” Regular issues of “RMZh” No. 15 dated May 26, 2000
- Lupanov V.P. “Algorithm for diagnosis and treatment of patients with chest pain and normal coronary angiogram (cardiac syndrome X)”, article in the journal “Breast Cancer”
- Akchurin R.S., Shiryaev A.A., Galyautdinov D.M. “Indications for coronary bypass surgery in patients with various forms of coronary artery disease,” Regular issues of “Breast Cancer” No. 19 dated 10/03/2002
Drug treatment
Drug treatment includes several groups of drugs:
- Beta blockers and calcium antagonists - these two groups reduce myocardial oxygen consumption and promote dilation of coronary vessels. These drugs are also effective for common concomitant conditions (hypertension and arrhythmias).
- Statins are drugs that help normalize the lipid profile of the blood. Prevents the growth of atherosclerotic plaques.
- Antiplatelet drugs - reduce the risk of coronary artery thrombosis by preventing blood clotting.
- Nitrates - this group of drugs eliminates the symptoms of angina attacks.
Stages of the disease
Stages of development and severity of congestive heart failure. Of the numerous signs of heart failure listed when describing a particular stage, it is necessary to highlight a few, each of which is sufficient to determine a specific stage. Stage I: Subjective symptoms of heart failure during moderate or greater exercise.
Stage IIA:
- pronounced subjective symptoms of heart failure with light loads;
- orthopnea;
- attacks of suffocation;
- radiographic, and in some cases, electrocardiographic signs of secondary pulmonary hypertension;
- reappearance of edema;
- re-enlargement of the liver;
- cardiomegaly without other signs of this stage;
- atrial fibrillation without other signs of this stage.
Stage IIB:
- repeated attacks of cardiac asthma;
- persistent peripheral edema;
- significant abdominal edema - permanent or reoccurring;
- persistent enlargement of the liver, which may shrink during treatment, but remains enlarged;
- atriomegaly;
- cardiomegaly in combination with at least one of the signs of the previous stage;
- atrial fibrillation in combination with at least one of the signs of the previous stage.
Stage III, terminal:
- severe subjective disorders with minimal exertion or at rest;
- repeated episodes of cardiac asthma during the week;
- dystrophic changes in organs and tissues.
If there is at least one sufficient sign of a more severe stage, then this stage should be established. Priority is given to clinical criteria. Negative results of instrumental studies often turn out to be inconclusive. The most obvious final manifestations of heart failure, such as a decrease in cardiac output, insufficient blood supply to organs and tissues and insufficient supply of oxygen to them, may be absent not only at rest, but also with the load available to the patient. Like blood pressure, the corresponding indicators may not go beyond the wide range of normal variants even in severe heart failure - until the last days and hours of the patient’s life (compensation at the pathological level).
Surgery
Surgical treatment is resorted to when the level of blood flow disturbance in the coronary arteries becomes critical and cannot be compensated for with medication. In this case, we are talking about two operations: coronary artery bypass grafting (CABG) and coronary artery stenting.
Coronary artery bypass grafting is an open operation in which access to the heart is achieved through opening the chest. The idea is to restore blood flow in the coronary artery after the site of narrowing. This is accomplished by connecting the affected artery and a healthy large vessel through another vessel, forming a kind of “bypass bridge” for the flow of blood. The necessary connecting vessel (shunt) can be taken from the lower leg, forearm and other places.
It is important to know that the rehabilitation period is long due to the long fusion of the sternum. Although the operation is complex, it has been practiced in Russia for a long time and, as a rule, goes well.
Coronary artery stenting is a minimally invasive operation in which a narrowed section of a coronary artery is expanded from the inside using a special metal mesh. The heart is most often accessed through the femoral artery of the leg. This surgical intervention is easy and has virtually no recovery period.
Pathogenesis
The mechanism of formation of coronary vascular insufficiency is determined by the interaction of a number of factors:
- presence of atherosclerotic plaque ;
- spasm of the coronary arteries;
- extracoronary thrombosis.
It is known for certain that the appearance of an atherosclerotic plaque is the morphological basis of ischemic myocardial damage in 90% of cases. Severe attacks of angina occur when the coronary vessels are damaged by 70-80%. When an artery spasms, a contraction of the smooth muscle vascular wall occurs, which creates an obstacle to normal blood flow in the myocardium. Coronary artery spasm is influenced by the sympathetic nervous system .
Thrombosis is of utmost importance . Thrombi form mainly on the surface of an atherosclerotic plaque at the site of disruption of the integrity and structure of the endothelial layer in the form of destruction and ulceration of the plaque.
Prevention
Prevention of coronary insufficiency essentially comes down to preventing the development of atherosclerosis and avoiding chronic stress. The importance of preventive measures increases greatly with age. Here's what you can do to significantly reduce the risk of progression and development of severe consequences of the pathology:
- Regular blood tests for lipid levels and cholesterol levels;
- Reducing the consumption of fatty foods;
- Regular moderate physical activity - at least 150 minutes per week;
- Getting rid of bad habits;
- Timely consultation with a doctor if appropriate cardiac symptoms appear;
- Minimizing stressful situations.
First aid for exacerbation
In the event of an acute attack, you should immediately call an ambulance. The patient's heart can stop at any moment, and it is impossible to resume its work without specialized equipment.
When the main task is completed, attention must be paid to stabilizing the patient’s condition. While waiting for an emergency team, you must:
- Provide peace. The patient should be immediately placed on a bed or sofa. If severe shortness of breath or cough occurs during an attack, the patient should be seated in a chair.
- Eliminate possible chest tightness. During heart attacks, even small loads, including clothing, have an impact on the chest area. The patient needs to completely expose the upper part of the waist, remove not only things, but also jewelry (beads, chains, pendants). If possible, measure your blood pressure
Provide fresh air. In acute coronary insufficiency, a squeezing sensation occurs in the chest area, making breathing difficult. By opening all windows, you can increase the flow and circulation of oxygen in the room. This will ease the patient's breathing and the stress on the heart.- Give medicine. The most common and effective remedy is Validol. It is able to reduce pain until the ambulance arrives. Validol is placed under the patient's tongue, and its effect begins within a few minutes.
Nitroglycerin is the second option for a heart attack. It also needs to be placed under the tongue. It acts faster, already within the first minute. If the pain has not decreased or the changes were insignificant, then after 10 minutes the tablet must be given again. This drug is contraindicated in people with low blood pressure.
There are many causes of coronary insufficiency. It can be triggered by both serious internal damage to the body and external factors. To maintain heart health, you need to take care of yourself, take preventive measures and give up bad habits.
Sources
- Coronary Heart Disease - nhlbi.nih.gov.
- Cardiovascular Therapy and Prevention, 2016; 15(2): 93–99 https://dx.doi.org/10.15829/1728-8800-2016-2-93-99.
- Kurdgelia T. M., Kislitsina O. N., Bazarsadaeva T. S. Sudden cardiac death: epidemiology, risk factors and prevention // BMIK. 2014. No. 3.
- Guide to faculty therapy: textbook / S. A. Boldueva, I. V. Arkharov, E. L. Belyaeva, E. G. Bykova, T. V. Ermolova, M. I. Ivanova, I. A. Leonova, A. P. Makhnov, N. S. Shvets, O. Yu. Chizhova; edited by S. A. Boldueva. — 3rd ed., add. and processed - St. Petersburg: Publishing house of North-Western State Medical University named after. I. I. Mechnikova, 2021. - p. 6-32; 64-76.
- Picard F., Sayah N., Spagnoli V., Adjedj J., Varenne O. Vasospastic angina: A literature review of current evidence. //Arch Cardiovasc Dis - 2021 - Vol.112 - No. 1 - p.44-55
Tests and diagnostics
Electrocardiography plays an important role in the diagnosis of acute and chronic heart failure , which is carried out at rest and under conditions of dosed physical activity. A characteristic sign indicating the presence of a pathology with coronary circulation in a patient is the registration of ST segment depression during maximum physical activity or 2-5 minutes after it. Arrhythmia that occurs during a stress test is also an indirect sign of cardiac circulatory pathology.
The condition of the coronary vessels can be assessed by performing coronary angiography , which allows one to identify areas of stenotic or occlusive vascular damage. The essence of the method is to administer an X-ray contrast agent and subsequently assess the patency of the arteries of the heart.
Laboratory diagnosis is based on determining blood levels of creatinine kinase , glucose, electrolytes, triglycerides, ALT, AST, total cholesterol and lactate dehydrogenase . Crucial importance is given to determining the level of markers of myocardial damage as a result of hypoxia and the concentration of troponins I and T. Detection of high concentrations allows one to suspect myocardial infarction or other damage to the heart muscle.
Differential diagnosis is carried out with the following diseases:
- esophagitis;
- esophageal spasm;
- ulcerative lesions of the digestive tract;
- pulmonary embolism;
- osteochondrosis of the thoracic spine;
- osteoarthritis of the shoulder joint;
- aortic dissection , etc.