Introduction
Microvascular angina (MVA) is a disease of the cardiovascular system, accompanied by chest pain typical of angina and electrocardiographic changes characteristic of myocardial ischemia, without damage to the epicardial coronary arteries, according to angiography [1]. SWS is characterized by prolonged pain in the heart area not only during and after physical activity [2], but also at rest, often accompanied by a decrease in the pain threshold and a change in the emotional status of patients. Despite the fact that the prognosis for MVA is usually favorable, angina pectoris significantly worsens the quality of life of patients and poses a significant burden on the healthcare system. Diagnosis of MBC in real clinical practice is often based on history and clinical data, which leads to false-positive or false-negative results. With coronary angiography, only the epicardial arteries can be seen, and it is not possible to assess the state of the microvasculature [3]. Considering the widespread prevalence of MHS among patients with heart pain, an in-depth study of this pathology, its diagnosis and treatment is necessary.
Unstable angina
Unstable angina is a concept under which several clinical situations are united: their common feature is the presence of attacks of pain in the chest.
Recently, unstable angina has been defined as an exacerbation of coronary heart disease (impaired blood circulation in the arteries designed to provide the heart muscle (myocardium) with the necessary supply of blood), threatening the development of myocardial infarction (death of a section of the heart muscle due to impaired circulation in it) or sudden death.
Symptoms of unstable angina
The main symptom of unstable angina is pain:
- the nature of the pain is quite strong, squeezing or pressing, often a feeling of heaviness or lack of air is felt;
- localization (location) of pain - behind the sternum or in the precordial region, that is, along the left edge of the sternum; pain radiates to the left arm, left shoulder or both arms, neck area, lower jaw, between the shoulder blades, left subscapular area;
- duration – more than 10 minutes.
Factors causing pain:
- it is impossible to determine a clear connection between pain and certain physical activity or other conditions (for example, pain appears in windy weather or after eating), a painful attack often occurs at rest or with minimal physical activity (bending over, walking around the apartment);
- the end of a painful attack - often after repeated administration of nitroglycerin;
- attacks occur more frequently than before.
Heart rhythm disturbances gradually develop:
- increased heart rate, palpitations;
- heartbeats become irregular and intermittent.
Shortness of breath occurs, which occurs with minimal physical activity and even at rest, and a feeling of lack of air.
Forms
There are several forms of unstable angina:
- new-onset angina (a disease manifested by discomfort or pain in the chest of a compressive, pressing nature, which is most often localized behind the sternum and can radiate (give) to the left arm, neck, lower jaw, epigastric (“under the stomach”) region);
- progressive angina (increasing intensity and/or duration of painful attacks, their occurrence with significantly less physical activity or at rest, the addition of shortness of breath, feeling of lack of air);
- post-infarction angina (occurring 24 hours and up to 8 weeks after the development of myocardial infarction (death of part of the heart muscle due to cessation of blood flow in this area)) or postoperative angina (within one to two months after a successful operation to restore blood flow).
In practice, the Braunwald classification (1989) is often used, dividing unstable angina into three classes (the higher the functional class, the greater the likelihood of developing complications:
- Class I - new angina or worsening of existing angina within a month;
- Class II - angina at rest during the previous month;
- Class III - angina at rest during the last 48 hours.
Depending on the conditions of occurrence, the following are also distinguished:
- class A - secondary unstable angina. This group includes patients in whom unstable angina develops in the presence of factors that aggravate ischemia (anemia (anemia), increased body temperature, infection, low blood pressure, uncontrolled hypertension, heart rhythm disturbances, emotional stress and others);
- class B - primary unstable angina. This group includes patients in whom unstable angina develops without extra-cardiac conditions that increase ischemia;
- class C - post-infarction unstable angina. This group includes patients in whom angina develops in the first 2 weeks of myocardial infarction.
Causes
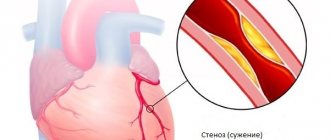
The main cause of unstable angina is the rupture of the so-called unstable atherosclerotic plaque (a formation consisting of a mixture of fats (primarily cholesterol (a fat-like substance that is a “building material” for the body’s cells) and calcium), which provokes the formation of a blood clot with incomplete closure of the lumen of the vessel .
The presence of a thrombus (blood clot) in the artery supplying the heart prevents adequate blood supply to the heart muscle, which leads to the appearance of pain and a full-blown clinical picture (set of symptoms) of unstable angina.
Plaque rupture is promoted by:
- accumulation of large amounts of fat and insufficient collagen content in it (a protein that forms the basis of connective tissue);
- inflammation and blood “fluidity” factors.
Place of MVS in the structure of IHD
Cardiovascular diseases (CVD) still maintain a leading position in the structure of mortality around the world [4, 5]. Thus, according to Rosstat data for 2021, mortality from CVD was 633 cases per 100 thousand population. A year earlier, this figure was 622.1 cases per 100 thousand population. The annual mortality rate from coronary heart disease (CHD) among the Russian population is 27%. However, only 40–50% of patients with coronary artery disease know about their disease and receive comprehensive treatment. In more than half of hospitalized patients diagnosed with acute coronary syndrome, coronary angiography reveals unchanged coronary arteries, which indicates a different origin of anginal pain, not excluding AVS [6]. It is now widely accepted that obstructive disease of the epicardial arteries is not the only cause of myocardial ischemia [7, 8]. In a retrospective analysis of the NCDR Cath registry, only 37.6% of patients were diagnosed with obstructive epicardial artery disease, while 69% of patients were confirmed to have transient myocardial ischemia using noninvasive diagnostic tests [9]. It should be noted that chest pain with intact coronary arteries is not always a consequence of MVA, therefore, diagnostics require the use of high-resolution optical systems.
Pathophysiology of coronary microvascular dysfunction (CMD)
The myocardium is an aerobic muscle tissue that requires a continuous supply of oxygenated blood to produce the energy needed to maintain the pumping function of the heart. Under basic cardiac conditions, 60–70% of the required oxygen can be obtained from arterial blood, so the increased myocardial oxygen demand can only be met by increasing coronary blood flow. The proximal coronary bed consists of epicardial arteries with a diameter of 5 to 0.5 mm and gives rise to intramural vessels. The distal coronary bed is represented by prearterioles, arterioles with a diameter of 40 to 400 μm and capillaries with a diameter of less than 10 μm, which constitute the main coronary circulatory system [10]. At rest, the tone of the coronary microvasculature is high, but arteriolar diameter can change rapidly, responding to increased myocardial oxygen demand and increasing coronary blood flow [11]. Capillaries and venules are an important component of the coronary microcirculation, therefore, structural and functional disorders at this level (for example, a drop in blood pressure in the capillary network or microembolization) can cause the development of myocardial ischemia. Depending on the clinical picture, different pathogenetic mechanisms of microvascular dysfunction are distinguished (Table 1) [12].
According to A. Faccini et al., inflammation is another potentially important cause of the development of CMD [13]. Coronary microvascular spasm, originally described in [14], can, like epicardial spasm, cause myocardial ischemia in the absence of increased myocardial oxygen demand and initiate resting angina. Today, there is no doubt that MWS is a heterogeneous syndrome, the development of which may be based on various pathogenetic mechanisms. Proposed mechanisms of CMD include altered regulation of coronary microcirculation by the autonomic nervous system and generalized vascular disorders. Thus, in one of the large studies by P. Ong et al. [15, 16] during testing of patients for acetylcholine, every fourth patient experienced microvascular spasm, characterized by ischemic changes on the ECG without visible changes in the diameter of the epicardial coronary arteries. AL Arrebola-Moreno et al. [17] reported that coronary microvascular spasm induced by intracoronary acetylcholine leads to disturbances in myocardial perfusion and contractility. In the VR study, Taqueti et al. [18] found a direct connection between CMD and the development of heart failure in patients with preserved ejection fraction. However, in most cases, MWS develops as a result of isolated CMD [19], which is the only (or predominant) mechanism responsible for the development of an attack of angina or asymptomatic myocardial ischemia [20].
Clinical picture and diagnosis of MWS
MWS is characterized by a triad of symptoms: 1) typical angina caused by physical activity, in combination or in the absence of rest angina and shortness of breath; 2) the presence of signs of myocardial ischemia according to electrocardiography (ECG), Holter monitoring (HM), stress tests in the absence of other diseases of the cardiovascular system; 3) unchanged or slightly changed coronary arteries (arterial stenosis less than 50%) [21]. Angina attacks can occur quite often, up to several times a week, but remain stable. Pain occurs both during physical activity, emotional stress, and at rest and is poorly relieved by nitrates. Thus, MVA is a form of chronic angina and, according to ICD-10, belongs to code I20.8 “Other forms of angina.”
There are 4 clinical criteria to suspect MWS [22]:
clinic of myocardial ischemia: anginal attacks or equivalent symptoms (for example, shortness of breath) during exercise or at rest;
absence of obstruction of the coronary arteries: narrowing of the artery lumen by 50% or less or fractional blood flow reserve of more than 0.8, according to computed tomography or invasive coronary angiography;
objective confirmation of myocardial ischemia (ischemic changes on the ECG at the time of the attack); anginal pain, ischemic changes on the ECG and/or echocardiographic study (EchoCG), decreased myocardial perfusion during stress tests;
confirmation of microvascular disorders: coronary blood flow reserve less than 2.0–2.5 (depending on the measurement technique); microvascular spasm during an acetylcholine test (ischemic changes on the ECG in the absence of epicardial spasm); increase in microvascular resistance indicators; slowing of coronary blood flow with a TIMI score of 25 or more.
If all 4 criteria are present, the diagnosis of MWS is most convincing. The presence of criteria 1 and 2 indicates the possibility of MVS, but MVS can be diagnosed only by obtaining objective evidence of myocardial ischemia (criterion 3) or impaired coronary microvascular function (criterion 4).
Myocardial ischemia is usually diagnosed by performing stress tests (the most commonly used are bicycle ergometry (VEM), treadmill test and 24-hour HM) by identifying horizontal depression of the ST segment more than 1 mm from the J point on the ECG [23]. It is very important to understand that the diagnosis of MBC in patients with chest pain should not be made solely by exclusion based on the results of coronary angiography. An integrated approach is required, taking into account all non-invasive and invasive research methods to verify myocardial ischemia [24]. Clinical guidelines suggest the following algorithm for confirming myocardial ischemia. The diagnosis is made on the basis of a combination of complaints, medical history (cardiovascular risk factors), and detected hidden coronary insufficiency. If angina is suspected, it is recommended to calculate the pre-test probability of coronary artery disease based on the nature of chest pain, age and gender of the patient [25]. However, a number of large studies in recent years have shown that this approach leads to a significant overestimation of the risk of coronary artery disease and is accompanied by the prescription of unnecessary additional diagnostic tests.
All patients with suspected coronary heart disease undergo an ECG as a first step [26]. In uncomplicated ischemic heart disease, specific signs of ischemia without exercise are most often absent. The only fairly specific sign is the appearance of a Q wave after a myocardial infarction. Isolated changes in the T wave are not very specific and are most often not taken into account. When performing an ECG with exercise, a specific sign of myocardial ischemia is horizontal or oblique depression of the ST segment with a depth of at least 0.1 MV, duration of at least 0.06–0.08 s from the J point in one or more ECG leads. Signs of vasospasm include transient elevation of the ST segment by at least 0.1 MV in two or more leads [27]. However, the sensitivity of the method decreases in patients with cicatricial changes on the ECG, with intraventricular blockades and left ventricular (LV) hypertrophy. I would like to note that a stress ECG test on a bicycle ergometer or treadmill is not informative in cases of complete blockade of the left bundle branch, the presence of a pacemaker and WPW syndrome, in which changes in the ST segment cannot be interpreted. In addition, false-positive results are often found in patients with resting ECG changes due to LV hypertrophy, electrolyte imbalance, rhythm and conduction disturbances [28].
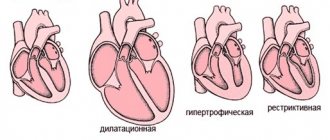
All patients with coronary heart disease or suspicion of it are recommended to undergo echocardiography, which allows assessing the systolic and diastolic functions of the left ventricle, identifying valvular pathology, excluding hypertrophic cardiomyopathy, aneurysm of the ascending aorta, and congenital heart pathology [22, 26]. However, with MWS, local zones of hypokinesis are not recorded on echocardiography at rest due to the large number of small affected areas, but one of the early signs of IHD, namely microvascular dysfunction, may be impaired LV diastolic function [29]. Other disadvantages of echocardiography are the low quality of visualization of the basal segments of the LV and false-positive results for pathological changes in the apical region [30]. The presence of tachycardia/arrhythmia in a patient significantly complicates the interpretation of echocardiography results. It should be noted that the disadvantage of all ultrasound methods for studying myocardial blood flow is the dependence of the interpretation on the qualifications and experience of the specialist performing the study. The sensitivity of echocardiography at rest in detecting myocardial ischemia, according to various authors, is 7.5–26.7%. The absence of such a sign as impaired regional and global contractility in patients with MWS can be explained by the peculiarities of the spread of ischemia, when it is limited to individual small areas of the myocardium [31].
According to modern European and Russian recommendations, CM is recommended for patients with chest pain and suspected arrhythmia. 12-lead CM may be useful if vasospastic angina is suspected. The diagnostic value of this method for routine examination of a patient with suspected myocardial ischemia is low. ST segment depression on the resting ECG can be interpreted as a sign of transient ischemia. However, ST segment depression is not associated with a poor prognosis, does not provide additional information compared with stress testing, and is often not even confirmed as a sign of transient ischemia by imaging stress testing. It should be noted that ST segment depression on the resting ECG may be due to LV hypertrophy. In this regard, CM cannot be used for a reliable diagnosis of myocardial ischemia, since the results of the study do not exclude or confirm IHD, including MVS [5, 22].
Stress tests are very important for verifying latent forms of myocardial ischemia by provoking ischemia with pharmacological or physical stress. The options for stress testing are varied. During their implementation, the myocardial oxygen demand increases (treadmill test, VEM, dobutamine test) or oxygen delivery to the myocardium decreases (tests with dipyridamole and adenosine) [22, 29].
The treadmill test is a more physiological method and has advantages over VEM due to the ability to dose-increase the load using the standard Bruce protocol to values greater than with VEM. A reliable sign of myocardial ischemia when performing VEM is horizontal or oblique ST segment depression of 1 mm or more [5]. The probability of diagnosing coronary artery disease is close to 90% if, during exercise, depression of the ST segment of the ischemic type reaches 2 mm or more and is accompanied by a typical attack of angina. VEM is indicated only for patients who are able to perform adequate physical activity on an exercise bike. Therefore, VEM is not possible if the patient has joint diseases or significant stenosis of the arteries of the lower extremities. Due to the relatively low sensitivity of VEM for ischemic heart disease, its negative result also does not exclude this diagnosis. The rate of false-positive results reaches 15% [24, 25]. Numerous studies have reported lower sensitivity of VEM and higher false-positive rates in women compared with men. The sensitivity and specificity of the treadmill test and VEM are approximately the same. False-negative tests lead to underestimation of angina symptoms.
Compared to stress ECG tests, stress echocardiography is more preferable. This is one of the most informative and cheapest methods for non-invasive diagnosis of myocardial ischemia, which has proven its high diagnostic value [32]. This method can be applied using all stress agents and has high sensitivity (80–85%) and specificity (84–86%) in the diagnosis of stenoses exceeding 50%. The capabilities of radioisotope methods in detecting MVS are being widely studied, but so far they have not become routine due to their complexity and high cost [21].
An important place in the diagnosis of cardiac arrest is occupied by positron emission tomography (PET) of the heart with stress testing [33]. According to most experts, PET of the heart at rest is not very informative. Disruption of myocardial blood flow can only be detected under conditions of functional load, which makes it possible to detect a decrease in blood flow in areas of the myocardium caused by endothelial dysfunction or vasospasm of the microvascular bed [34]. The distribution of the radiopharmaceutical against the background of stress allows us to identify even small areas of the LV in which myocardial hypoperfusion is noted. There are different types of stress tests: exercise test on a bicycle ergometer or treadmill, pharmacological test with vasodilators, transesophageal pacing and cold test. In clinical practice, during PET perfusion studies with 13N-ammonium, a pharmacological test with adenosine is most often used. According to the literature, PET using pharmacological stress tests has high specificity (78–100%) and sensitivity (87–97%) in the diagnosis of myocardial ischemia [33, 34]. The PET method, like single-photon emission computed tomography (SPECT), provides information about the presence or absence of myocardial ischemia, its location and severity, and scar changes. At the same time, PET, unlike SPECT, is characterized by higher image quality, has unique capabilities for calculating blood flow (in ml/min/g), which allows non-invasive assessment of blood flow reserve and provides a lower radiation dose. However, PET is generally less used due to its low availability and high cost. To date, studies are being conducted combining the PET method with intravenous pharmacological load. The radiopharmaceutical adenosine triphosphate, available on the pharmacological market, is used as a load; it has proven itself as a vasodilator, has a short decay period, and rarely causes side effects. The use of dobutamine seems inappropriate for MWS, since the expected effects of decreased myocardial contractility due to the ischemia it causes are extremely rare, as is the case with the use of stress echocardiography [21, 23]. The diagnosis of vasospastic angina is made on the basis of transient ischemic changes in the ST segment during an attack of angina (characteristic rises in the ST segment during an attack). To exclude vasospastic angina, it is possible to provoke coronary spasm during coronary angiography [35] by administering acetylcholine chloride [23]. The test for vasospasm is considered positive if: a) an anginal attack occurs; b) ischemic changes on the ECG; c) pronounced vasoconstriction of the epicardial arteries [36]. If a test with acetylcholine is accompanied by pain and ischemic changes on the ECG, but there is no spasm of the epicardial arteries, then we can talk about vasoconstriction at the level of the microvasculature.
Angina pectoris
Atherosclerosis
Diabetes
Stroke
23447 May 20
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Angina pectoris: causes, symptoms, diagnosis and treatment methods.
Definition
Angina is a clinical syndrome manifested by a feeling of tightness or squeezing pressing pain in the chest, which is most often localized behind the sternum and can radiate (“give”) to the left arm, neck, lower jaw, and to the epigastric region (epigastric region).
Pain occurs during physical activity or exposure to other factors that increase the heart's need for oxygen, and lasts from 1 to 15 minutes. It goes away with rest (when you stop exercising) or 1-3 minutes after taking nitroglycerin.
Translated from ancient Greek, angina means “narrow (weak, cramped) heart.”
Causes of angina
The development of angina is based on three mechanisms:
- atherosclerotic lesions of the coronary arteries;
- transient vascular thrombus formation;
- decreased coronary blood flow due to spasm or increased tone of the coronary arteries.
Angina pectoris makes itself felt during physical activity or stressful situations when there is a narrowing of the lumen of the coronary artery by 50-70%.
The severity of angina depends on the degree of coronary artery stenosis, its location and extent, the number and number of affected arteries. An atherosclerotic plaque can block a vessel completely or partially. With an increase in blood pressure, the inner layer of the coronary arteries (endothelium), damaged by the atherosclerotic process, can be easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
The formation of a blood clot, especially against the background of a vessel spasm, can lead to its complete or partial blockage.
When myocardial tissue is damaged, pain mediators (serotonin, histamine, bradykinin, etc.) are released, which affect pain receptors.
There are modifiable (those that can be influenced) and non-modifiable factors that can provoke the development of angina. Modifiable diseases include dyslipoproteinemia (violation of the normal ratio of blood lipids), arterial hypertension, diabetes mellitus, smoking, low physical activity, obesity, and stress. Non-modifiable factors - male gender, age, family history of cardiovascular diseases (myocardial infarction or ischemic stroke in close relatives - up to 65 years (for women) and up to 55 years (for men)).
Classification of the disease
The most widespread classification of angina pectoris, developed
on the basis of WHO expert recommendations
:
- Stable angina pectoris (indicating functional class from I to IV).
- Class I – the patient tolerates physical activity well, angina attacks occur only during high-intensity exercise; Class II - slight limitation of usual physical activity, angina attacks occur when walking on level ground for a distance of more than 500 m, when climbing more than one floor; Class III – pronounced limitation of normal physical activity, attacks occur when walking at a normal pace on level ground for a distance of 100-150 m, or when climbing one floor; Class IV - angina occurs with little physical activity, walking on level ground at a distance of less than 100 m.
- Unstable angina:
- new-onset angina (less than 1 month from the onset of attacks);
- progressive angina (increasing attacks in frequency, duration, intensity with expanding localization and irradiation);
- early post-infarction (within 2 weeks after acute myocardial infarction) or post-operative angina.
- Spontaneous (vasospastic, variant, Prinzmetal) angina.
In practice, doctors also use the clinical classification of stable angina
:
- stable exertional angina (indicating the functional class);
- vasospastic angina;
- microvascular angina.
Symptoms of angina
Pain from angina can sometimes be perceived not as true pain, but as a feeling of discomfort, a feeling of heaviness, squeezing, tightness, distension, burning or lack of air.
Most often, the pain is localized behind the sternum or along the left edge of the sternum. It can radiate to the neck, lower jaw, teeth, interscapular space, and less often to the elbow or wrist joints, mastoid processes.
Pain with angina pectoris usually lasts from 1 to 15 minutes.
Pain occurs at the peak of physical or emotional stress. Stressful situations, due to increased activity of the sympathoadrenal system, lead to an increase in heart rate, increased blood pressure and myocardial contractility, which means the myocardial need for oxygen increases. After taking nitroglycerin or stopping the exercise, the pain stops, and the pain attack stops faster in a sitting or standing position.
As angina progresses, a moment comes when attacks occur even with minimal exertion, and then even under conditions of physical rest.
Angina at rest joins angina pectoris and is combined with it. In such cases, attacks occur during times of increased oxygen consumption by the heart muscle, for example, during REM sleep, when the heart begins to beat faster.
In some patients, an attack of angina may occur in a horizontal position due to increased blood flow to the heart.
Vasospastic angina develops independently of physical and emotional stress, is caused by spasm of the coronary arteries, and usually occurs at a younger age than exertional angina due to atherosclerosis of the coronary arteries. In patients with vasospastic angina, many typical risk factors for atherosclerosis cannot be identified. The disease may be accompanied by threatening disturbances in heart rhythm, leading to the development of myocardial infarction and/or sudden death.
A feature of vasospastic angina is very severe attacks, usually localized in a typical location. They occur at night or early in the morning, and also when exposed to cold on exposed areas of the body.
Microvascular angina is characterized by attacks that occur some time after physical activity, during emotional stress and at rest; they are poorly controlled by nitroglycerin. The cause of microvascular angina is considered to be dysfunction of small coronary arteries (100-200 μm in diameter) in the prearteriolar segment of the coronary bed. In more than 70% of cases, microvascular angina coexists with classical angina in patients with atherosclerotic stenoses.
Diagnosis of angina pectoris
The diagnosis of angina is established on the basis of a combination of complaints (pain characteristic of angina) and information received from the patient about the course of the disease.
For all patients with suspected coronary heart disease, the following questions are asked:
- current or past smoking;
- the presence of cardiovascular diseases and/or deaths from cardiovascular diseases in the patient’s immediate relatives (father, mother, siblings);
- previous cases of seeking medical help and the presence of previously registered electrocardiograms, studies and conclusions;
- the presence of concomitant diseases in order to assess additional risks;
- currently taken medications.
To clarify the diagnosis and existing complications, data from laboratory and instrumental examination methods are used.
All patients with suspected angina are recommended to have a lipid profile tested to detect dyslipoproteinemia:
- triglycerides (Triglycerides);
Treatment of MVS
Treatment of MWS includes standard therapy for coronary artery disease: β-blockers, nitrates, calcium antagonists, statins, antiplatelet agents, second-line drugs (angiotensin-converting enzyme (ACE) inhibitors, nicorandil, ivabradine, ranolazine, trimetazidine), non-drug treatments (spinal cord stimulation, psychotherapy) [37].
Traditional antianginal drugs are prescribed in the first stages of treatment. Short-acting nitrates are recommended to relieve anginal attacks, but they often have no effect. Thus, only less than 50% of patients noted an improvement in their condition when using sublingual nitroglycerin. Conversely, nicorandil, which opens potassium ATP channels and has nitrate-like effects, has been reported to have a beneficial effect in MWS [38].
In patients with dominant symptoms of angina pectoris, therapy with β-blockers, which have been proven to eliminate the symptoms of angina pectoris, seems rational. These are the drugs of first choice, especially in patients with obvious signs of increased adrenergic activity (high heart rate at rest or during exercise) [39]. However, patients with microvascular or epicardial spasm should use caution when using β-blockers (especially those lacking vasodilatory properties) because these drugs may increase coronary vasoconstriction by masking α-adrenergic receptors in the coronary vessels [37].
Another drug that reduces myocardial oxygen demand due to its rate-lowering effects is ivabradine [40]. Calcium antagonists as first-line drugs are indicated in case of variability in the threshold of angina pectoris, especially in the angiospastic genesis of myocardial ischemia. Patients with clinical signs of MWS and lipid metabolism disorders are shown statins, which are known to have a positive effect on endothelial function. ACE inhibitors improve exercise tolerance and relieve angina symptoms [41]. The positive effect of ranolazine on endothelial function is known. In the work of E. Rayner-Hartley et al. [42] assessed the effect of ranolazine on the quality of life of patients with severe refractory angina caused by MVA. Patients received ranolazine at a dose of 1000 mg/day together with sulodexide for 4 weeks. The use of ranolazine improved the quality of life and reduced the number of visits to medical care. To correct endothelial dysfunction, trimetazidine is also used, which improves the metabolism of cardiomyocytes during myocardial ischemia. In the study by S.A. Boldueva et al. [43] showed the effectiveness of using trimetazidine in patients with MWS, in addition to standard antianginal therapy, with improvement in the clinical picture, quality of life, myocardial perfusion and endothelial function.
Unfortunately, traditional therapy for MWS is not always effective; the quality of life remains low due to pain, and patients are often hospitalized. Therefore, all patients with MWS require active correction of traditional risk factors, such as hypertension, diabetes mellitus, smoking, obesity, sedentary lifestyle, and hyperlipidemia.
Syndrome X in cardiology (“microvascular angina”)
In approximately 10–20% of patients who undergo diagnostic coronary angiography due to acute or chronic cardiac ischemic syndrome, the coronary arteries are intact. Even if we assume that in some of them the symptoms of ischemia may be due to other cardiac and non-cardiac causes, then at least one out of ten patients with typical angina pectoris does not have hemodynamically significant stenoses of the coronary arteries. The presence of typical angina with unchanged coronary arteries was first described by N. Kemp in 1973 [1]. This syndrome is called “ X(X) syndrome” .
Cardiac syndrome X is a pathological condition characterized by the presence of signs of myocardial ischemia in the absence of atherosclerosis of the coronary arteries and spasm of the epicardial coronary arteries on coronary angiography (signs of myocardial ischemia: typical attacks of angina and ST segment depression ≥ 1.5 mm (0.15 mV) duration more than 1 minute established during 48-hour ECG monitoring). Thus, cardiac syndrome X is diagnosed in patients:
• with typical chest pain;
• with positive stress tests;
• with angiographically normal epicardial coronary arteries and no clinical or angiographic evidence of coronary artery spasm;
• with the absence of systemic arterial hypertension with and without left ventricular hypertrophy, as well as the absence of disturbances in the systolic function of the left ventricle at rest.
In rare cases, patients with syndrome X develop left bundle branch block with subsequent development of dilated cardiomyopathy. It should be noted that in the absence of changes in the coronary arteries during angiography, there is often occlusive pathology of the distal vessels (microvascular angina).
Some authors use the term “microvascular angina,” meaning that patients with typical angina have a normal coronary angiogram and reduced coronary reserve.
Syndrome X is usually classified as one of the clinical forms of coronary artery disease, since the concept of “myocardial ischemia” includes all cases of imbalance in oxygen supply and myocardial demand for it, regardless of the reasons causing it.
It should be noted that the capabilities of the angiography method in assessing the state of the coronary bed, in particular microvascular, are limited. Therefore, the concept of “angiographically unchanged coronary arteries” is very arbitrary and indicates only the absence of atherosclerotic plaques narrowing the lumen of the vessels in the epicardial coronary arteries. The anatomical features of the small coronary arteries remain “angiographically invisible.” Causes of cardiac syndrome X:
The etiology of cardiac syndrome X remains unclear and only some pathophysiological mechanisms leading to the development of typical clinical and instrumental manifestations of the disease have been established:
• increased sympathetic activation; • endothelial dysfunction; • structural changes at the microcirculation level; • metabolic changes (hyperkalemia, hyperinsulinemia, “oxidative stress”, etc.); • increased sensitivity to intracardiac pain; • chronic inflammation; • increased stiffness of arteries, etc.
There are a number of hypotheses that determine the pathogenesis of syndrome X. According to the first of them, the disease is caused by myocardial ischemia due to functional or anatomical disorders of microcirculation in intramuscular (intramural) prearterioles and arterioles, i.e. in vessels that cannot be visualized by coronary angiography. The second hypothesis assumes the presence of metabolic disorders leading to disruption of the synthesis of energy substrates in the heart muscle. The third hypothesis suggests that syndrome X occurs with increased sensitivity to painful stimuli (decreased pain threshold at the level of the thalamus) from various organs, including the heart.
Despite intensive research over the past 35 years regarding the pathogenesis of coronary syndrome X, many important questions remain unanswered.
Among patients with cardiac syndrome X, middle-aged people, mostly women, predominate. Less than 50% of patients with cardiac syndrome X have typical exertional angina, and the majority have atypical chest pain. Symptoms of cardiac syndrome X:
The main complaint includes episodes of angina-type chest pain that occurs during physical activity or is provoked by cold or emotional stress; with typical irradiation, in some cases the pain is longer lasting than with ischemic heart disease, and is not always relieved by taking nitroglycerin (in most patients the drug worsens the condition). Symptoms accompanying cardiac syndrome X resemble vegetative-vascular dystonia. Cardiac syndrome X is often found in people who are suspicious, with a high level of anxiety, against the background of depressive and phobic disorders. Suspicion of these conditions requires consultation with a psychiatrist. The diagnostic criteria for cardiac syndrome X include: • typical chest pain and significant depression of the ST segment during physical activity (including on the treadmill and bicycle ergometer); • transient ischemic depression of the ST segment ≥ 1.5 mm (0.15 mV) lasting more than 1 minute during 48-hour ECG monitoring; positive dipyridamole test; • positive ergometrine (ergotavin) test, a decrease in cardiac output against its background; • absence of atherosclerosis of the coronary arteries during coronary angiography; • increased lactate content during ischemia when analyzing blood from the coronary sinus area; • ischemic disorders during stress myocardial scintigraphy with 201 Tl.
Syndrome X resembles stable angina. However, clinical manifestations in patients with syndrome X are very variable, and in addition to exertional angina, attacks of resting angina can also be observed.
When diagnosing cardiac syndrome X, the following should also be excluded: • patients with spasm of the coronary arteries (vasospastic angina), • patients in whom non-cardiac causes of chest pain are documented by objective methods, for example:
- musculoskeletal causes (osteochondrosis of the cervical spine, etc.); — neuropsychic causes (anxiety-depressive syndrome, etc.); - gastrointestinal causes (esophageal spasm, gastroesophageal reflux, gastric or duodenal ulcer, cholecystitis, pancreatitis, etc.); - pulmonary causes (pneumonia, tuberculosis in the lungs, pleural overlays, etc.); - latent infections (syphilis) and rheumatological diseases.
Treatment of cardiac syndrome X:
Treatment for the group of patients with syndrome X remains not fully developed. The choice of treatment is often difficult for both treating physicians and the patients themselves. The success of treatment usually depends on the identification of the pathological mechanism of the disease and is ultimately determined by the participation of the patient himself. An integrated approach to the treatment of patients with cardiac syndrome X is often necessary.
There are various approaches to drug treatment: antianginal drugs, ACE inhibitors, angiotensin II receptor antagonists, statins, psychotropic drugs, etc. Antianginal drugs such as calcium channel blockers (nifedipine, diltiazem, verapamil, amlodipine) and β-adrenergic blockers (atenolol, metoprolol , bisoprolol, nebivolol, etc.) are necessary for patients with documented myocardial ischemia or impaired myocardial perfusion. Sublingual nitrates are effective in 50% of patients with cardiac syndrome X. There is evidence regarding the effectiveness of nicorandil, which has a bradycardic effect, the α1-blocker prazosin, L-arginine, ACE inhibitors (perindopril and enalapril), cytoprotectors (trimetazidine).
General advice on changing quality of life and treating risk factors, especially aggressive lipid-lowering therapy with statins (reducing total cholesterol to 4.5 mmol/l, LDL cholesterol less than 2.5 mmol/l), should be considered as vital components of any chosen treatment strategies.
Physical training. With cardiac syndrome X, tolerance to physical activity decreases, physical detraining and inability to perform exercise are observed due to a low pain threshold. Physical training increases the pain threshold, normalizes endothelial function and “delays” the appearance of pain during exercise in this category of patients.
Forecast.
The prognosis of patients with cardiac syndrome “X” is usually favorable. Complications typical for patients with coronary artery disease with stenotic atherosclerosis of the coronary arteries (in particular, myocardial infarction) are extremely rare. Survival with long-term follow-up is 95–97%, but in the majority of patients, repeated attacks of angina over many years have a negative impact on the quality of life. While not associated with increased mortality or an increased risk of cardiovascular “events,” cardiac syndrome X often seriously impairs patients' quality of life and poses a significant burden to the health care system. It must be emphasized that the prognosis is favorable in the absence of endothelial dysfunction. In these cases, the patient should be informed about the benign course of the disease. When excluding patients with left bundle branch block and patients with secondary microvascular angina due to serious systemic diseases such as amyloidosis or multiple myeloma, the prognosis of patients with cardiac syndrome X is favorable both in terms of survival and preservation of left ventricular function, but in some patients clinical manifestations of the disease persist for quite a long time.