Anemia is called megaloblastic if precursor cells (megaloblasts) are “to blame” for its origin. The term is characteristic of the division of all types of anemia based on the principle of morphological changes in cellular composition. In the International Classification of Diseases, such a diagnosis is mentioned only in the section “Other anemia associated with nutrition” and is coded D53.1.
For practicing doctors, the clinical classification of anemia depending on the cause is more understandable and acceptable:
- from blood loss;
- from disruption of red blood cell production;
- from increased destruction of red blood cells.
In this list, megaloblastic anemia is included in the second group, along with aplastic, iron deficiency, sideroblastic and caused by chronic diseases.
According to medical statistics, a tenth of all anemias belong to this group. The incidence increases with age from 0.1% in young people to 4% after 70 years. Hematologists note the low detection rate of the disease. This is associated with the masking of the main symptoms by the widespread unjustified use of vitamin B12 for various pathologies.
Subtypes of megaloblastic anemias
According to more detailed criteria for the mechanism of impaired erythrocyte synthesis, this type of anemia is divided into 2 subtypes.
Anemia associated with a lack of vitamin B12 and folic acid:
- due to the lack of sufficient quantities in food products;
- due to disruption of the absorption process in the intestines;
- due to altered transport and metabolism;
- due to increased needs of the body.
Another type is megaloblastic anemia, which is not related to B12 and folic acid deficiency; the causes are poorly understood.
Vitamin deficiency may be congenital or acquired. Their content is reduced under the influence of drugs from the groups of antiviral, anti-tuberculosis drugs, and drugs for relieving seizures.
The destructive effects of alcohol and drugs have been proven.
Treatment of other diseases starting with the letter - m
| Treatment of malaria |
| Treatment of manic-depressive syndrome |
| Treatment of Marseilles fever |
| Treatment of mastitis |
| Treatment of mastopathy |
| Treatment of meningococcal infection |
| Migraine treatment |
| Treatment of multiple myeloma |
| Treatment of skeletal myeloma |
| Treatment of mycosis of the lungs |
| Treatment of mycoplasmosis |
| Treatment of myocarditis |
| Treatment of thrush |
| Treatment of urolithiasis |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.
Mechanism of disruption of red blood cell formation
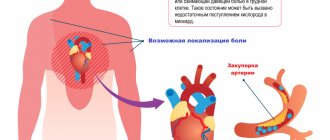
The disease is associated with changes in the DNA synthesis of bone marrow cells, which is why instead of proper red blood cells, erythroblasts are produced, which cannot bind molecular oxygen and carry it throughout the body to organs and tissues.
At the same time, the process of cell maturation or the biochemical synthesis of hemoglobin is not damaged, as in other anemias. The main changes occur in cell division, the balance between the nucleus and protoplasm is disrupted. Nuclear chromosomes are delayed in development and disrupt the structure of the nucleus.
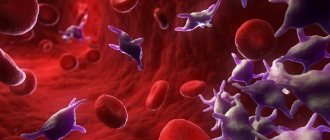
Megaloblasts are much larger in size, the nucleus is not located in the center, the nucleus can be divided into segments
The body itself destroys “low-quality” abnormal cells in the bone marrow; they live half as long as a normal red blood cell. Under the influence of the hormone erythropoietin, the consumption of vitamins B12 and folic acid increases, since they are enzymes of this process. Erythroblasts accumulate in the peripheral blood. At the same time, there is an increase in the process of destruction of granulocytes and platelets in the spleen and intestinal epithelium.
What diseases can it be associated with?
Megaloblastic anemia develops against the background of malabsorption in the digestive system caused by diseases of the stomach, small intestine and competitive absorption of cyanocobalamin in the intestine.
This is observed in the following conditions:
- violation of the secretion of internal factor in atrophic gastritis caused by hereditary, toxic, immunological factors,
- during gastrectomy,
- with partial resection of the stomach;
- for tumors,
- with blind loop syndrome,
It should be remembered that hyperchromic anemia in elderly people often occurs due to tumor processes (stomach cancer), for which an instrumental examination of the digestive system is performed (fibrogastroscopy, colonoscopy, X-ray examination, etc.). Megaloblasts are found in the bone marrow of leukemia. With metastases of malignant neoplasms to the bone marrow (except for stomach cancer), normochromic anemia usually occurs.
The role of vitamin B12 in the development of anemia
The composition of vitamins in the body depends on the processes of “internal production”, the amount supplied with food, and the possibility of absorption. B12 and folic acid are not synthesized independently. The average level of B12 in the blood is maintained due to sufficient accumulation (4 mcg is absorbed daily).
For a deficiency to occur, it must not be supplied in food for years or the destruction process must sharply intensify. The importance for biochemical processes is associated with the presence in the vitamin formula of two essential coenzymes (methylcobalamin and deoxyadenosylcobalamin).
Methylcobalamin is necessary for DNA synthesis, and through this process they ensure the normal process of hematopoiesis, the “ripening” of red blood cells, leukocytes and platelets. Its deficiency leads to the megaloblastic type. Deoxyadenosylcobalamin is an active enzyme in fat metabolism. With a deficiency, the structure of the nerve roots of the spinal cord is disrupted.
All membranes of the spinal cord pass on to the nerve roots, a lack of vitamin causes the destruction of the protective coating
In order for vitamin components to be released from food products, pancreatic protease enzymes are needed. Only they are capable of destroying molecules blocked by protein. For further absorption in the large intestine, constant acidity and calcium ions are required. In the form of transcobalamin, it is delivered to liver cells and bone marrow.
The liver accumulates the vitamin and releases it into the intestines with bile. B12 deficiency, in addition to anemia and neurological symptoms, contributes to disruption of the stomach and intestines.
B12 anemia: treatment
Treatment tactics for B12-deficiency anemia are developed by CELT specialists according to diagnostic results and individual patient indications. If the diagnosis is confirmed, treatment will be carried out for life, and every five years an endoscopic examination of the gastric mucosa will be required, eliminating the risk of developing malignant neoplasms.
In order to compensate for the deficiency of the vitamin, the patient is prescribed intramuscular administration. Treatment of diseases and disorders that initiated the development of anemia is carried out:
- elimination of helminths;
- taking digestive enzymes;
- operations for diverticula and malignant tumors;
- food with a high content of animal protein;
- taking glucocorticoids for disorders of the production of internal factor.
If you start treating anemia in a timely manner, your blood counts will return to normal in one and a half to two months. Neurological symptoms persist for up to six months; if treatment was started at an advanced stage, they are irreversible and cannot be cured.
The Department of Hematology at CELT welcomes candidates, doctors and professors of medical sciences with over twenty-five years of practical and scientific experience. You can make an appointment with them online or by contacting our operators. No less experienced and qualified specialists perform septoplasty in the otolaryngology department.
At CELT you can consult a hematologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
By making an appointment with a hematologist, you can get a comprehensive consultation. The doctor is competent to treat various blood diseases, most of which can be identified in the early stages and prescribe timely treatment to cope with the disease quickly and easily.
The role of folic acid in the development of anemia
Folic acid in the form of salts (folates) enters the body with food. Unlike B12 reserves, folates run out within a month (up to 4 months are possible) after delivery from the duodenum ceases. Absorption of folic acid occurs in the small intestine. The carrier protein delivers the vitamin to the liver and bone marrow.
The further role of folates depends entirely on the presence of cyanocobalamin. With a lack of B12, they cannot participate in the process of DNA synthesis in cells. Accordingly, the synthesis of blood elements is disrupted. Abnormal megaloblasts develop.
Prevention and prognosis
To prevent the development of anemia, the following recommendations must be followed:
- Eat right by eating foods rich in vitamins B9 and B12.
- Lead a healthy lifestyle, give up alcoholism.
- Avoid situations that could lead to parasite infection.
- Treat all diseases of the digestive system in a timely manner.
As for the prognosis, with timely treatment it is favorable and it is possible to completely get rid of anemia.
Who develops B12 deficiency with folic acid
The most common causes of deficiency are:
- vegetarianism and passion for fashionable diets for weight loss;
- diseases of the stomach and intestines associated with diarrhea and impaired absorption of food;
- diphyllobothriasis is a disease from the group of helminthiasis, infection with tapeworm eggs occurs through dirty hands, fish, in the Russian Federation, focal areas along northern rivers, in the Urals and the Far East;
- pregnancy with uncompensated expenses (anemia can be transmitted to the fetus);
- chronic alcoholism.
The broad tapeworm lives in the human body for years, sucking out vitamins
Clinical symptoms
The symptoms are best studied for Addison-Biermer anemia. There are 2 stages of flow:
- initial (preclinical) - there are no patient complaints, manifestations can be detected by chance only by laboratory tests, especially if they are carried out after stressful situations;
- clinical - typical symptoms appear.
Common symptoms of anemia include:
- dizziness;
- complaints of general malaise, weakness;
- nausea and loss of appetite;
- inflammation and burning sensation of the tongue;
- the appearance of painful ulcers on the oral mucosa (stomatitis);
- yellowing of the skin due to an increase in the level of bilirubin in the blood and damage to liver cells.
Megaloblastic anemia is characterized by damage to the nervous system (due to destruction of the spinal cord roots), which manifests itself:
- tingling in fingers;
- impaired skin sensitivity;
- difficulty in movement.
In case of brain damage and severe course, the following are possible:
- memory impairment;
- hallucinations, delusions;
- increased irritability;
- coma.
Diagnostics
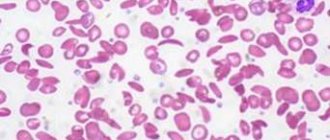
A general blood test allows you to suspect anemia at the preclinical stage. The general analysis reveals:
- decrease in the number of red blood cells;
- increasing their size;
- high color index (more than 1.1);
- unchanged hemoglobin content;
- under a microscope, remnants of nuclei in the form of rings and inclusions are detected in erythrocytes;
- decrease in the number of reticulocytes, neutrophils, platelets;
- all cells are increased in size.
Analysis of bone marrow punctate is carried out before the start of treatment with vitamin injections, since the morphological structure changes within 24 hours after the first administration of the drug.
In the bone marrow composition:
- cells of the erythrocyte lineage predominate;
- a discrepancy is detected between their nucleus and cytoplasm;
- disruption of other lineages is confirmed by large neutrophils and megakaryocytes.
In biochemical tests
- moderate increase in free bilirubin;
- serum iron is slightly increased;
- an increase in LDH (lactate dehydrogenase enzyme, indicating increased destruction of red blood cells) is detected.
Conducting a quantitative analysis for the content of B12 and folic acid is possible only in specialized laboratories in hematology departments. This study allows us to determine the exact cause of anemia.
Publications in the media
Anemia is a decrease in the Hb content per unit volume of blood, often with a simultaneous decrease in the number of red blood cells (or the total volume of red blood cells). The term “anemia” without detail does not define a specific disease, but indicates changes in blood tests, i.e. anemia should be considered one of the symptoms of pathological conditions. Frequency. 157 per 100,000 population in 2001
General signs • Hb content <100 g/l, erythrocyte count <4.0´1012/l, serum iron content <14.3 µmol/l • The isolated existence of one symptom or their combination is possible. For example, thalassemia is not characterized by a decrease in the number of red blood cells.
Classification criteria • Based on the morphology of erythrocytes, microcytic, normocytic and macrocytic anemias are distinguished (-cytic indicates the size of erythrocytes). An objective evaluation criterion is the average erythrocyte volume (MEV); normal is 80–94 femtoliters (fl) • Based on the degree of saturation of erythrocytes Hb (or serum iron content), hypochromic, normochromic and hyperchromic anemias are distinguished (-chromic indicates the color of erythrocytes). An objective assessment criterion is the average Hb content in the erythrocyte (ASGE); Normal is 27–33 picogram (pg).
Based on the combination of the first and second criteria, anemia is distinguished: •• Hypochromic microcytic (low SER and SSGE) •• Macrocytic (increased SER) •• Normochromic normocytic (SER and SSGE within normal limits) • Based on the degree of erythrocyte regeneration, anemia is distinguished between hyporegenerative (regenerative) and hyperregenerative. Determined by the number of blood reticulocytes or reticulocyte index • By the degree of hematopoietic effect of erythropoietin. Both the content of erythropoietin and the sensitivity of immature erythroid cells to it are taken into account.
Pathogenetic classification • Anemia due to impaired Hb synthesis and iron metabolism (hypochromic microcytic) •• Iron deficiency anemia (IDA) •• Thalassemia •• Sideroblastic anemia •• Anemia in chronic diseases (60% normochromic normocytic) • Anemia due to impaired DNA synthesis (hyperchromic macrocytic with megaloblastic type of hematopoiesis) •• Pernicious anemia and other B12-deficiency anemias •• Folate deficiency anemia • Other pathogenetic mechanisms (usually normochromic normocytic anemia) •• Anemia combined with a decrease in the bone marrow response to erythropoietin ••• Aplastic anemia • •• Disorders characterized by cellular infiltration of the bone marrow (myelophthisic anemia) ••• Anemia due to erythropoietin deficiency •• Hyperregenerative anemia ••• Acute posthemorrhagic anemia ••• Hemolytic anemia.
Abbreviations • SSGE - average Hb content in erythrocytes • SEV - average erythrocyte volume.
ICD-10 • D50–D53 Nutrition-related anemias • D55–D59 Hemolytic anemias • D60–D64 Aplastic and other anemias
APPLICATIONS
Congenital dyserythropoietic anemia • Type I (*224120, 15q, CDAN1, r gene). Clinical picture: moderate developmental delay, macrocytic dyserythropoietic anemia, mild hemochromatosis, bone marrow Gaucher cell-like macrophages. Laboratory tests: N-acetylglucosaminyl transferase II deficiency • Type II (*224100, 20q, CDAN2 gene, HEMPAS, r). Clinical picture: dyserythropoietic anemia, multinucleated erythroblasts, lysis of red blood cells upon serum acidification, bone marrow Gaucher cell-like macrophages. Laboratory tests: N-acetylglucosaminyl transferase II deficiency (EC 2.4.1.138) • Type III (*105600, 15q21, CDAN3, Â, r gene). Clinical picture: congenital dyserythropoietic anemia, macrocytosis, giant multinucleated bone marrow erythroblasts, jaundice; increased risk of myeloma or monoclonal gammopathy. Laboratory findings: hemosiderinuria, abnormal nuclei and intracytoplasmic inclusions in erythroblasts, highly polyploid giant mononuclear erythroblasts, elevated serum thymidine kinase levels. ICD-10 • D64.4 Congenital dyserythropoietic anemia
Megaloblastic thiamine-sensitive anemia (*249270, 1q23.2–q23.3, TRMA gene, r) is combined with diabetes and sensorineural hearing loss. Clinical picture: megaloblastic anemia, sensitive only to thiamine, ring-shaped sideroblasts, diabetes, sensorineural hearing loss, dysphonia, progressive optic atrophy, transposition of internal organs, generalized edema, congenital septal heart defects. Laboratory tests: aminoaciduria, a-ketoglutarate dehydrogenase deficiency, iron accumulation in erythroblast mitochondria. ICD-10. D53.1 Other megaloblastic anemias, not elsewhere classified
Anemia myelophthisis is a normochromic normocytic anemia that occurs when normal bone marrow is replaced by pathological tissue. Etiology • Lymphoma • Leukemia • Multiple myeloma • Tuberculosis • Granulomatosis • Metastasis of a malignant tumor to the bone marrow. Diagnostics. The appearance of immature leukocytes and nucleated red blood cells in the peripheral blood in a disproportionately large number relative to the severity of anemia, metastatic cells (solid tumor metastases). Bone marrow puncture and trephine biopsy confirm the diagnosis. Treatment is etiotropic and symptomatic. Synonyms • Myelopathic anemia • Leukoerythroblastosis. ICD-10 • D61.9 Aplastic anemia, unspecified
Anemia due to erythropoietin deficiency is normochromic (sometimes hypochromic) normocytic hyporegenerative anemia. Erythropoietin deficiency occurs in chronic renal failure when the level of end products of nitrogen metabolism in the blood increases and creatinine clearance is less than 45 ml/min. The severity of anemia usually depends on the severity of renal failure (it is most severe with primary damage to the glomerular apparatus). Etiology and pathogenesis • The synthesis of erythropoietin is suppressed by a high content of uremic toxins (in anemia as a result of chronic diseases, this effect is mediated by cytokines), which leads to the suppression of erythropoiesis • The sensitivity of the bone marrow to erythropoietin is reduced • The lifespan of erythrocytes is shortened (minor hemolysis) • Nutritional deficiency of folic acid is possible acid or iron • Uremic hemorrhagic diathesis; possible hemorrhages in the pleura, pericardium, brain •• When the endothelium of the renal vessels is damaged (malignant arterial hypertension, periarteritis nodosa, acute ischemia), microangiopathic hemolytic anemia occurs with fragmentation of erythrocytes and thrombocytopenia (in children it occurs acutely in the form of hemolytic-uremic syndrome). Treatment is etiotropic and pathogenetic • Recombinant erythropoietin is the drug of choice. Initial dose: 50–100 units/kg IV or SC 3 times a week. After 2–3 months of treatment, the erythrocyte count increases in most patients. It is necessary to monitor the concentrations of iron and folic acid in the blood, because their deficiency can lead to secondary complications • Blood transfusions (use with caution). ICD-10. B63.8 Anemia in chronic diseases classified elsewhere (specify the cause of chronic renal failure)
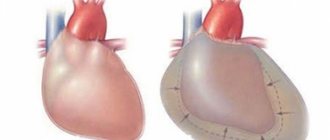
Microangiopathic hemolytic anemia is a secondary or congenital anemia that develops due to narrowing or obstruction of small blood vessels, which leads to mechanical damage to red blood cells during their interaction with the vascular endothelium. Etiology • Arterial hypertension • Chronic kidney disease • Prosthetic heart valves • Hemolytic-uremic syndrome • Disseminated intravascular coagulation (DIC) • Congenital microangiopathic hemolytic anemia (276850, r): polymorphic symptoms, possible involvement of the central nervous system; occurs due to fibrin deposition or the formation of platelet thrombi in the arterioles and capillaries of most organs; Characterized by thrombocytopenia, episodes of fever and petechial rash, glomerulopathy, megakaryocytosis (bone marrow). The clinical picture is determined by the underlying disease. The diagnosis is confirmed by identifying fragmented red blood cells in a peripheral blood smear in the form of schizocytes, spur cells and other abnormal forms of red blood cells. Treatment is etiotropic and restorative. ICD-10 • D59.4 Other non-autoimmune hemolytic anemias
Acute posthemorrhagic anemia is a normochromic normocytic hyperregenerative anemia that occurs as a result of acute blood loss over a short period of time. The minimum blood loss that poses a danger to the health of an adult is 500 ml. The severity of the clinical picture is determined by the amount of blood lost, the speed and source of bleeding. Etiology • Trauma • Surgical interventions • Ectopic pregnancy • Impaired hemostasis • Various diseases of internal organs accompanied by acute bleeding (for example, peptic ulcer of the stomach and duodenum). Clinical picture • General signs of anemia (tachycardia, shortness of breath, drop in blood pressure and venous pressure, pallor of the skin and mucous membranes). The severity of these changes does not correspond to the severity of anemia, because they often appear in response to a cause of bleeding (such as pain or injury) • Sudden dry mouth is an important sign of acute bleeding. Treatment is aimed at restoring blood volume • Surgical stop of bleeding • Blood transfusions. ICD-10 • D62 Acute posthemorrhagic anemia
Anemia in chronic, infectious and oncological diseases (as a rule, normochromic normocytic hyporegenerative anemia, in 40% of cases - hypochromic microcytic anemia) ranks second in frequency after IDA. Etiology and pathogenesis • Shortening of the period of circulation of mature forms of erythrocytes in the blood • Impaired utilization of iron (its release from the depot is impaired) • Relative deficiency of erythropoietin (the effect is mediated by the suppression of its production by cytokines - b- and g-IFN) • Altered bone marrow response to erythropoietin. The clinical picture is determined by the underlying disease (for example, rheumatoid arthritis, tuberculosis, cancer). Diagnosis • Moderate anemia (Hb concentration 80–100 g/l) • Serum ferritin concentration is normal or slightly increased (unlike IDA) • Fe2+ content in the blood serum is reduced, but TIVR is also reduced (unlike IDA) • Amount reticulocytes are reduced (hyporegenerative anemia). Treatment is etiotropic. ICD-10 • D63* Anemia in chronic diseases classified elsewhere •• D63.0* Anemia in neoplasms (C00-D48+) •• D63.8* Anemia in other chronic diseases classified elsewhere
Reticulocyte index. Calculation method: 0.5´(reticulocyte content´Ht of the patient/normal Ht). The content of reticulocytes is expressed as a percentage of the number of red blood cells; 0.5 — correction factor taking into account the severity of anemia; instead of Ht, you can use the volume of cell mass (BCV).