What is angina?
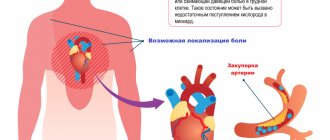
Angina pectoris is not an independent disease, but a syndrome that is a manifestation of coronary heart disease (CHD). Coronary heart disease occurs due to insufficient blood supply to the heart muscle. Angina pectoris is a kind of heart signal about oxygen deficiency of the heart. How does the heart give this signal? The signal is felt in the form of attacks of short-term sudden acute squeezing, pressing, burning pain in the region of the heart. In some patients, the pain is accompanied by a state of general discomfort, a feeling of lack of air, and interruptions in the functioning of the heart.
What triggers an angina attack?
At first, attacks can be mild, short-term, 1-2 minutes each, during very heavy or intense physical activity, running, climbing stairs, going out into the cold, walking against the wind. An attack can be triggered by emotional disorders, smoking, staying in a stuffy space, overeating, taking energy tonics or excessive doses of alcohol.
How to distinguish angina from myocardial infarction?
| Typical angina pectoris | Typical myocardial infarction |
| Pain in the center of the chest, in the middle third of the sternum, can spread to the left arm, shoulder blade, lower jaw, and upper abdomen. | The pain is similar to that of angina pectoris, but more often it is felt as more intense, unbearable, tearing and affects the entire left half of the chest. |
| Discomfort is mild or moderate. | Severe discomfort, increased sweating, dizziness, nausea, increasing feeling of lack of air, fear of death. |
| An attack of angina is more often associated with previous physical activity or emotional arousal. | Myocardial infarction can occur at any time, including at rest. |
| The pain attack takes about 3 – 15 minutes. | A painful attack with discomfort and suffocation lasts for at least 15 – 30 minutes or more, and there is a tendency for symptoms to increase. |
| With rest, the pain usually goes away. | In a state of physical rest, the pain does not go away completely and intensifies when talking and deep breathing. |
| The use of nitroglycerin under the tongue or in the form of an aerosol from 1 to 3 doses interrupts an attack of angina. | Symptoms do not completely resolve after 3 doses of nitroglycerin. |
Symptoms, course
With angina, pain is always characterized by the following symptoms:
- has the nature of an attack, that is, it has a clearly defined time of onset and cessation, subsidence;
- occurs under certain conditions and circumstances;
- begins to subside or completely stops under the influence of nitroglycerin (1 - 3 minutes after its sublingual administration).
Conditions for the occurrence of an attack of angina pectoris: most often - walking (pain when accelerating, when climbing a mountain, during a sharp headwind, when walking after eating or with a heavy load), but also other physical effort, and/or significant emotional stress . The conditioning of pain by physical effort is manifested in the fact that as it continues or increases, the intensity of the pain inevitably increases, and when the effort stops, the pain subsides or disappears within a few minutes.
The above three features of pain are sufficient to make a clinical diagnosis of an attack of angina and to distinguish it from various pain sensations in the heart and generally in the chest that are not angina.
It is often possible to recognize angina pectoris at the first visit of the patient, while to reject this diagnosis requires observation of the course of the disease and analysis of data from repeated questions and examinations of the patient. The following signs complement the clinical characteristics of angina, but their absence does not exclude this diagnosis:
- localization of pain behind the sternum (most typical!), rarely - in the neck, in the lower jaw and teeth, in the arms, in the shoulder girdle and shoulder blade (usually on the left), in the heart area;
- the nature of the pain is pressing, squeezing, less often - burning (like heartburn) or the sensation of a foreign body in the chest (sometimes the patient may experience not pain, but a painful sensation behind the sternum and then he denies the presence of pain itself);
- simultaneous with an attack of increased blood pressure, pallor, perspiration, fluctuations in pulse rate, the appearance of extrasystoles.
All this characterizes angina pectoris. The thoroughness of the medical questioning determines the timeliness and correctness of the diagnosis of the disease. It should be borne in mind that often a patient, experiencing sensations typical of angina, does not report them to the doctor as “not related to the heart,” or, on the contrary, focuses on diagnostically minor sensations “in the area of the heart.”
Angina at rest, in contrast to steiocardia at exertion, occurs independently of physical effort, more often at night, but otherwise retains all the features of a severe attack of angina pectoris and is often accompanied by a feeling of lack of air and suffocation.
In most patients, the course of angina is characterized by relative stability. This is understood as a certain duration of occurrence of signs of angina, attacks of which during this period have changed little in frequency and strength, occur when the same or similar conditions occur, are absent outside of these conditions and subside under conditions of rest (angina pectoris) or after taking nitroglycerin. The intensity of stable angina is classified by the so-called functional class (FC).
IFC includes persons whose stable angina is manifested by rare attacks caused only by excessive physical stress. If attacks of stable angina pectoris also occur during normal loads, although not always, such angina is classified as FC II, and in the case of attacks during light (domestic) loads, it is classified as FC III. IV FC is recorded in patients with attacks with minimal loads, and sometimes in their absence.
Angina pectoris should alert the doctor if: an attack occurs for the first time, but especially if attacks that occur for the first time become more frequent and intensify from the very first weeks of the illness; the course of angina pectoris loses its stability: the frequency of attacks increases, they occur in conditions other than before (at lower loads, stress), they also appear outside of stress (at rest, in the early morning), as if they move from FC I - II to FC III - IV FC; that is, the course of angina has changed, acquiring significantly new characteristics.
ECG changes (decreased ST segment, T wave inversion, arrhythmias), as well as a slight increase in the activity of serum enzymes (CPK, LDH, LDH1, AST), are usually absent in such cases, but the presence of these signs additionally confirms the instability of angina. Pre-infarction angina does not always result in heart attack (the probability of developing a heart attack is about 30%); this must be taken into account in clinical diagnosis.
Occasionally, the so-called variant (vasospastic) form of angina occurs, characterized by the spontaneous nature of the attack, sharp rises in the ST segment recorded on the ECG, refractoriness to beta blockers (anaprilin and obzidan), but sensitivity to calcium ion antagonists (verapamil, phenigidine, corinfar).
The basis for the diagnosis of any of the forms and variants of the course of angina pectoris is a correctly constructed and carefully conducted questioning of the patient. In unclear cases, a test with physical activity (bicycle ergometer test) is performed in order to identify hidden coronary insufficiency. The tactics for establishing a diagnosis are determined by the following schematic sequence of solving the main issues:
- Is the nature of the pain coronary (anginal)?
- Are there signs of pre-infarction angina?
- Is the current exacerbation during coronary heart disease related to the influence of extracardiac (concomitant) diseases?
Only a convincingly reasoned negative answer to the first of three questions gives the right to search for another cause (source) of pain: the discovery of another disease in a patient as the source of his pain cannot exclude the presence of simultaneous attacks of angina pectoris as a manifestation of coronary heart disease. About pain in the heart area of a non-anginal nature ( see Cardialgia.)
Complications of angina pectoris itself are not observed if it does not become an expression of the progression of cardiosclerosis and if it does not turn out to be the first manifestation of a developing myocardial infarction. Therefore, an attack of angina pectoris that lasts for 20 - 30 minutes, as well as unstable angina pectoris, require an electrocardiographic examination in the next few hours (days) and determination of the presence of reactive changes in the activity of a number of enzymes in the blood, body temperature ( see Myocardial infarction
).
First aid for an angina attack
If an angina attack occurs, you must follow the instructions received from your attending physician or (if there were no such instructions) follow the algorithm:
- Note the time of onset of the attack.
- Measure blood pressure, heart rate and pulse.
- Sit (preferably in a chair with armrests) or lie in bed with the head of the bed raised.
- Provide fresh air (free your neck, open a window).
- Take acetylsalicylic acid (aspirin 0.25 g), chew the tablet and swallow.
You should not take acetylsalicylic acid (aspirin) if you are intolerant to it (allergic reactions) and have already taken it that day, as well as if there is a clear exacerbation of gastric and duodenal ulcers.
6. Take 0.5 mg of nitroglycerin. If in the form of a tablet, put it under the tongue and dissolve; if in the form of a capsule, bite it, do not swallow; if in the form of a spray, inhale (inject) one dose under the tongue without inhaling.
If, after taking nitroglycerin, severe weakness, sweating, shortness of breath, or a severe headache appears, then you need to lie down, raise your legs (on a bolster, pillow, etc.), drink one glass of water and then do not take nitroglycerin.
You should not take nitroglycerin if you have low blood pressure, severe weakness, sweating, severe headache, dizziness, acute impairment of vision, speech or coordination of movements.
7. If the pain has completely disappeared and the condition has improved after taking aspirin and 1 dose of nitroglycerin after 5 minutes, limit physical activity and discuss further treatment with your doctor.
8. If the pain persists for more than 10-15 minutes, you must take nitroglycerin a second time and urgently call an ambulance!
ATTENTION ! If aspirin or nitroglycerin is not available and the pain persists for more than 5 minutes, call an ambulance immediately!
9. If pain persists even after taking the second dose of nitroglycerin after 10 minutes, you need to take nitroglycerin a third time. Wait for an ambulance.
Causes of angina
The main cause of angina is atherosclerosis.
Atherosclerotic plaques that arise on the walls of the coronary arteries lead to a decrease in the lumen of blood vessels. Under normal conditions, the heart muscle has enough nutrition, but when the heart works hard, it is not possible to provide the necessary blood flow, hence the pain. If the lumen is narrowed significantly (and with severe atherosclerosis, the narrowing can reach 75% or more), attacks are possible even in the absence of load. The risk of developing atherosclerosis, and, consequently, the occurrence of angina, is increased by the following factors:
- sedentary lifestyle;
- poor nutrition (tendency to salty, fatty, heavy foods);
- overweight (obesity);
- smoking and alcohol abuse.
The performance of the vascular system is affected by age, heredity, and some chronic diseases (primarily diabetes and hypertension). The risk of angina increases due to emotional instability (nervous tension leads to increased stress on the heart).
Risk factors for developing angina
The following factors lead to narrowing of the coronary vessels and insufficient blood supply to the myocardium:
- atherosclerosis - deposition of cholesterol plaques in the walls of blood vessels;
- hypotension ー low blood pressure;
- coronary artery thrombosis;
- age-related changes in blood vessels.
In the vast majority of cases, angina is caused by atherosclerotic lesions of the coronary arteries. It develops due to disturbances in the metabolism of cholesterol and other lipids: excess animal fats in the diet, lack of plant foods. Therefore, proper nutrition is the basis for successful prevention of angina pectoris.
Nicotine also constricts blood vessels, so smokers develop angina more often.
The risk group for the development of angina pectoris includes:
- people over 55 years of age;
- men;
- smokers;
- people who abuse alcohol and drugs;
- people with pathologies of the cardiovascular system (heart defects, heart failure);
- with pathologies of the respiratory system (bronchial asthma, chronic obstructive diseases);
- overweight.
All these factors increase the risk of developing atherosclerosis, cardiac ischemia and angina. Most of them can be eliminated through lifestyle changes.
Treatment methods for angina pectoris
The course of treatment for angina pectoris is prescribed individually, depending on the general condition of the patient and the form of the disease. A cardiologist treats angina pectoris. Treatment of angina pectoris is aimed at reducing the risk of myocardial infarction, reducing the frequency of attacks and normalizing quality of life. First of all, factors contributing to the development of atherosclerosis must be eliminated. Treatment of angina includes:
Lifestyle change
Treatment of angina will be more successful if the patient changes his lifestyle. You should stop smoking and provide the necessary physical activity. and follow an appropriate diet.
Drug therapy
Drug therapy for angina includes:
- nitrates. These drugs dilate blood vessels and thus reduce the load on the heart. This group of drugs includes nitroglycerin;
- antiplatelet drugs that prevent the formation of blood clots (acetylsalicylic acid has a similar effect);
- beta blockers, which reduce heart rate. As a result, the myocardial oxygen demand decreases;
- statins, which lower cholesterol levels and slow down the development of atherosclerosis;
- other drugs.
Revascularization
If the risk of myocardial infarction is high, revascularization is performed - surgical treatment aimed at restoring coronary blood flow. For revascularization, balloon angioplasty and coronary artery bypass grafting are used.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Methods for diagnosing angina pectoris
Treatment of angina begins with diagnosing the condition of the coronary vessels. For this purpose, procedures such as:
ECG
Electrocardiography (ECG) is a basic diagnostic procedure in cardiology. Patients with angina pectoris are also recommended to undergo daily ECG monitoring.
More information about the diagnostic method
Treadmill test
Exercise tests such as the treadmill test and bicycle ergometry are also widely used to diagnose heart conditions.
More information about the diagnostic method
Echocardiography
If cardiac abnormalities are detected, echocardiography (ultrasound of the heart) is performed.
More information about the diagnostic method
Coronary angiography
The condition of the coronary vessels is determined by coronary angiography (x-ray examination of the heart vessels with the introduction of a contrast agent).
More information about the diagnostic method
Blood chemistry
Laboratory diagnosis of angina pectoris involves, first of all, a biochemical blood test. Indicators such as cholesterol, hemoglobin, AST, ALT, and other indicators are assessed.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.