Coronary heart disease or IHD is one of the most common and serious cardiac diseases, characterized by unpredictability and severity of manifestations. The victims of this disease most often are men of active age - 45 years and older.
Disability or sudden death is a very likely outcome with ischemic heart disease. In our country alone, about 700 thousand deaths caused by various forms of ischemia are recorded annually. Globally, the mortality rate from this disease is almost 70%. This is why regular monitoring by a cardiologist is so important!
1 Blood test for ischemia
2 Tests for cardiac ischemia
3 Diagnostics of coronary artery disease in "MedicCity"
The development of coronary artery disease is provoked by an imbalance between the myocardial need for blood supply and the actual coronary blood flow.
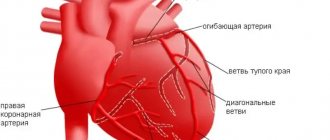
The main reason for insufficient blood supply and oxygen starvation of the heart muscle is narrowing of the coronary arteries due to atherosclerosis (atherosclerotic plaques in the lumen of blood vessels), atherothrombosis and (or) spasm.
The pathological process can affect either one or several arteries at once (multivascular lesion). Significant narrowing of the coronary arteries impedes the normal delivery of blood to the myocardial fibers and causes pain in the heart.
Without proper treatment and medical supervision, coronary ischemic heart disease, caused by a lack of oxygen and nutrients, can lead to myocardial infarction, cardiac arrest and sudden cardiac death.
Hungry Heart
The heart, like any other organ, is supplied by blood vessels called coronary arteries. Narrowing of the coronary arteries leads to insufficient nutrition of the heart muscle, to oxygen “starvation,” which doctors call “ischemia.” Ischemia can occur when the heart requires more nutrients, such as during exercise. In this case, the patient experiences an attack of chest discomfort or angina. If blood flow through the coronary artery is suddenly blocked by a thrombus, then acute oxygen deficiency occurs and necrosis of part of the heart muscle, the so-called myocardial infarction, occurs.
Classification of coronary heart disease
Depending on the symptoms, the following main forms of the disease are distinguished:
Coronary death . Symptoms develop rapidly: loss of consciousness, pupils are dilated and do not respond to light. No pulse, no breathing.
Post-infarction cardiosclerosis . Among the characteristic signs: heart rhythm disturbances, manifestations of acute (attack of suffocation - “cardiac asthma”, pulmonary edema) and chronic heart failure (swelling of the legs, shortness of breath). The patient complains of a feeling of lack of air, shortness of breath, and swelling of his legs and feet.
Acute coronary syndrome. New-onset angina, progressive angina, myocardial infarction, etc.
Myocardial infarction . Often severe pressing and burning pain behind the sternum, radiating to the jaw, left shoulder blade and arm. Lasts up to half an hour or more, does not go away when taking nitroglycerin under the tongue. The patient also develops cold sweats, blood pressure decreases, weakness, vomiting and fear of death may appear.
Angina pectoris . A person complains of chest pain - squeezing, squeezing, burning behind the sternum during physical activity and sometimes at rest. Possible symptoms of angina include pain in the neck, left shoulder blade, lower jaw or left arm. The pain is usually short-lived.
Angina pectoris is one of the most striking manifestations of coronary heart disease. Self-treatment of angina pectoris with folk remedies is unacceptable! Only a doctor, based on his professional experience and diagnostic techniques, can draw conclusions about a person’s condition and the necessary treatment measures!
1 Ultrasound of the heart for angina pectoris
2 Ultrasound of the heart in “MedicCity”
3 Blood tests for ischemic heart disease
If angina pectoris occurs for the first time, if angina attacks begin to occur more often, last longer and manifest themselves more strongly, we are talking about acute coronary syndrome and a high risk of developing myocardial infarction. Such patients should be urgently hospitalized by ambulance to a hospital, where coronary angiography will be performed on an emergency basis and blood flow in the arteries of the heart will be restored, which will avoid the occurrence of myocardial infarction and, as a consequence, disability.
Silent myocardial ischemia
IHD may not be accompanied by pain. This ischemia is called silent ischemia.
The manifestation of the disease in the case of silent myocardial ischemia is often myocardial infarction or sudden coronary death. Therefore, it is very important to be regularly examined by a cardiologist, especially for people at risk (diabetics, hypertension, smokers, obese people, the elderly, etc.).
Such hidden ischemia can be detected using some instrumental techniques, for example, ECG with exercise (Veloergometry, treadmill). It is during a stress test on the electrocardiogram that changes specific to coronary heart disease are especially pronounced.
Two faces of a terrible disease
Often in the specialized literature two different terms are used - “angina pectoris” and “myocardial infarction”. Angina pectoris and myocardial infarction are two manifestations of one disease - coronary heart disease (CHD). At the same time, many patients who have had a heart attack are well aware of the symptoms of angina pectoris and, conversely, patients suffering from angina pectoris have ever suffered a myocardial infarction. The danger of myocardial infarction is that it often strikes suddenly - in about half of the cases, myocardial infarction occurs without any obvious harbingers of impending disaster.
Detection of myocardial ischemia
Symptoms of coronary heart disease can be either pronounced or subtle.
Among the most characteristic symptoms of IHD are the following:
- Pressing pain and burning behind the sternum and in the heart area during physical activity;
- shortness of breath on exertion.
But sometimes IHD does not reveal itself until myocardial infarction! In this case, the classic symptoms of coronary heart disease may be noticed too late.
When the clock counts...
Angioplasty and stenting of arteries
- Cost: 100,000 - 250,000 rubles.
- Duration: 40 minutes
- Hospitalization: 1-2 days in hospital
More details
A fair question: can it effectively treat myocardial infarction? After all, its consequence is the necrosis of part of the heart muscle. If, during a developing heart attack, the cause of its occurrence is eliminated, that is, the patency of the clogged artery of the heart is restored, then the negative consequences of a heart attack can be significantly reduced.
The most accessible method of treating a heart attack is the administration of drugs that dissolve the clot. Such treatment can begin as soon as the doctor diagnoses a heart attack. But it is most effective only in the first hours from the onset of the disease. Later, the clot becomes more resistant to the drugs. In addition, after 6 hours from the onset of a heart attack, most of the cells in the affected area die and it is pointless to use drugs that are not sufficiently effective by this time. Another approach is mechanical removal of the obstruction in the coronary artery. To do this, using a special thin catheter, under X-ray control, the thrombus is recanalized and the lumen of the narrowed artery is expanded with a special balloon. This treatment method is called coronary angioplasty. Angioplasty is more effective than drug treatment late after a heart attack, with relatively “old” thrombosis.
National Society for the Study of Atherosclerosis
Myocardial infarction (necrosis or death of the heart muscle) is a serious complication of coronary artery disease, sometimes fatal. According to statistics in the United States, acute myocardial infarction leads to death on average in every third man aged 35-50 years [9]. Moreover, more than half of these deaths occur within the first 3-4 hours from the onset of a heart attack due to life-threatening arrhythmia (ventricular fibrillation), which without treatment always leads to death. We can say that myocardial infarction is a special case of ischemic heart disease. Myocardial infarction occurs due to blockage (thrombosis) of the artery supplying blood to one or another part of the heart muscle. As a rule, a heart attack is preceded by the rupture of an atherosclerotic plaque and the deposition of platelets on the surface of such an altered plaque. All this contributes to the fact that the lumen of the artery begins to close, and this leads to acute myocardial ischemia. Myocardial infarction is usually preceded by an increase in blood viscosity. If during a myocardial infarction a spasm of the coronary artery occurs at the site of the same plaque, this causes an even greater narrowing of the artery, up to its complete blockage.
Sometimes it is possible to develop myocardial infarction only as a result of prolonged spasm of atherosclerotically unchanged coronary arteries [9], for example, as a result of vasospastic angina (see below). As a result of myocardial infarction, a section of the heart muscle dies. Over time, this area is replaced by another tissue, scar (or so-called connective tissue), which does not contain muscle fibers. This condition is called post-infarction cardiosclerosis, in contrast to atherosclerotic cardiosclerosis, when muscle tissue is replaced by connective tissue without a previous myocardial infarction. During a myocardial infarction, both the entire section of the heart muscle can die, in its entire thickness (transmural myocardial infarction), or only one of its layers: the inner (subendocardial infarction), middle (intramural infarction) or outer (subepicardial infarction). If an infarction occurs in only one of the layers of the heart muscle, this does not exclude the possibility that a transmural infarction will not subsequently develop in the remaining layers. The prognosis for life and preservation of sufficient contractile function of the myocardium as a result of a myocardial infarction depends, first of all, on the area of dead myocardium (large-focal or small-focal infarction). And this, in turn, is determined by the number of affected arteries and the location of the blockage in the artery itself. If the blockage occurs at the mouth of an artery that supplies blood to a large area of the myocardium, then the prognosis can be very dismal. Thus, the more distant from the mouth the part of the artery is affected, the safer the prognosis. On average, a scar is formed within 1.5-2 months, after which the patient’s ability to work can be restored.
Manifestations of myocardial infarction
The disease can begin in different ways: both against the background of general well-being, and as a worsening of angina attacks. Sometimes myocardial infarction is the first manifestation of coronary artery disease. The patient is restless, sweating, pale, and may experience nausea and vomiting. The painful attack is much more severe and longer lasting than normal angina attacks. Previously helpful medications stop working. The pain can be so unbearable that it can lead to painful shock with loss of consciousness and a sharp drop in blood pressure. If a painful attack is not relieved by 3 tablets of nitroglycerin, you should urgently call an ambulance. Sometimes myocardial infarction does not manifest itself at all. It is in such cases that they say that the patient suffered a myocardial infarction “on his feet.”
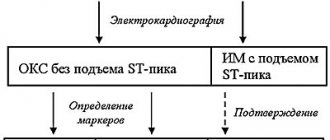
Diagnosis of myocardial infarction
To diagnose myocardial infarction, the same methods are used as for diagnosing coronary artery disease in general. Tests with dosed physical activity are strictly contraindicated due to the high risk of developing various complications and death of the patient. In most cases of myocardial infarction, characteristic changes appear on the ECG. An additional method for diagnosing myocardial infarction is to identify its biochemical markers - biological substances (enzymes) that appear or significantly increase only in this disease. Biochemical markers of myocardial infarction are creatine phosphokinase (CPK) and its components (fractions), as well as troponin and some others. Already 4 hours after the onset of the disease, especially with unclear manifestations of the disease and a questionable ECG, the remaining doubts can be resolved with the help of markers.
Treatment of myocardial infarction
Myocardial infarction is an absolute indication for hospitalization of a patient in a cardiology hospital for treatment and round-the-clock medical supervision. Only timely medical intervention can reduce the risk of severe consequences of a heart attack. In the hospital, treatment is usually carried out to limit the area of infarction (intravenous administration of nitroglycerin, β-blockers, calcium ion antagonists), increase cardiac output (dobutamine, dopamine, adrenaline), reduce blood viscosity and coagulability (heparin), normalize blood pressure, and eliminate arrhythmia. Painkillers, including narcotics, are usually administered by emergency medical technicians. If necessary, their administration is continued in the hospital. Hospitalization in a cardiology hospital, where specialists are proficient in interventional diagnostic and treatment methods, is considered ideal. When a patient is admitted to such a hospital, he may be prescribed coronary angiography, which will make it possible to accurately determine which artery caused the heart attack. The patient can then undergo TLBAP and/or stenting of this infarction-related artery in order to restore blood flow through it. With this sequence of events, the consequences of even severe myocardial infarction can be minimized.
But, unfortunately, interventional cardiology departments are not yet available in all medical hospitals in our country. In a number of cardiology hospitals, and ideally at home, doctors from the cardiology emergency medical team perform so-called systemic thrombolysis. This method involves the intravenous administration of drugs that can eliminate (“dissolve”) blood clots in the coronary arteries. Systemic thrombolysis is more common than TLBAP and coronary artery stenting. In the departments of interventional cardiology, in turn, there is the opportunity to perform intracoronary thrombolysis, i.e. injection of a clot-dissolving drug (thrombolytic) directly into the coronary arteries. Thrombolysis is an alternative to TLBAP and coronary artery stenting, but it does not eliminate stenoses. Typically, coronary bypass surgery is not performed during acute myocardial infarction, which is associated with an increased operational risk of death of the patient. As an exception, surgery is performed in cases where it is necessary to eliminate life-threatening complications of myocardial infarction, for example, rupture of the interventricular septum, etc. Recently, attempts have been made aimed at restoring the number of muscle cells lost as a result of myocardial infarction. To do this, donor “progenitors” of muscle cells, so-called stem cells, are introduced into the myocardium. These cells are introduced either during heart surgery, injecting them into the scar zone, or injected into the coronary arteries when performing coronary angiography. Currently, such scientific material is being accumulated.
Complications of myocardial infarction
As with any other disease, complications occur as a result of myocardial infarction. The development of complications is determined by the area of the infarction and which particular area of the myocardium is affected. Deadly complications are external ruptures of the heart, that is, rupture of its outer walls. If one of the inner walls (septa) of the heart ruptures, this condition is potentially life-threatening. Much again depends on the size of the defect formed and on how the heart copes with the consequences caused by the presence of this defect. Sometimes, to save the patient's life in such cases, emergency heart surgery is required. The main method for diagnosing cardiac ruptures is echocardiography. As a result of a heart attack, cardiac aneurysms can form. An aneurysm is a bulging formation on the surface of the heart that passively bulges outward during heartbeat. Aneurysms may be composed of scar tissue (true aneurysm) or tissue surrounding the heart (false aneurysm). The danger of an aneurysm is that blood clots can form in its cavity. Fragments of these blood clots can spread through the bloodstream, causing heart attacks in other internal organs (brain, kidneys, liver, lungs, etc.). This spread of blood clot fragments throughout the body is called thromboembolism. Therefore, all patients with a cardiac aneurysm are advised to take anticoagulants - medications that prevent the formation of blood clots. In addition, the area of the aneurysm can be a source of persistent and life-threatening cardiac arrhythmias. Diagnosis of cardiac aneurysms is carried out using ECG, echocardiography and chest x-ray. Treatment of cardiac aneurysms is only surgical. During the operation, the aneurysm is excised, and the surrounding myocardium is sutured together. Aneurysm plasty can also be performed: after excision of the aneurysm, a biological or synthetic patch is sutured in its place. Excision or repair of aneurysms is performed simultaneously with coronary bypass surgery. Another dangerous complication of myocardial infarction is cardiogenic shock - a condition in which the heart cannot cope with its pumping (contractile) function. This condition occurs when at least 50% of the contractile myocardium mass dies as a result of a heart attack. Only in a small percentage of cases, according to some data up to 20%, can the patient’s life be saved [9].
Cardiogenic shock is a special case of post-infarction heart failure, that is, a decrease in the pumping function of the heart due to myocardial infarction. As a result of the death of any part of the myocardium, as mentioned above, a scar is formed, which, unlike the rest of the myocardium, cannot fully contract and contribute to the pumping function of the heart. A scar is like a big patch on a balloon: on the one hand, the balloon seems to be intact, but on the other hand, it is not at all necessary that this balloon can now be fully inflated. A situation is created when the myocardium, which has not suffered from a heart attack, is forced to take on the function of the dead myocardium, while some zone of the heart will contract more intensely, and another less. Over time, healthy myocardium will begin to lose its “contractile” positions, especially when performing physical activity. Ultimately, heart failure will arise and gradually progress - the inability of the heart to fully cope with its pumping function. Blood will begin to linger in the veins of the pulmonary (small) and then systemic circulation. As a result, shortness of breath will appear as a consequence of stagnation of blood in the vessels of the lungs, as well as edema, hepatomegaly (enlargement of the liver, manifested by heaviness in the right hypochondrium), ascites (increase in the volume of the abdomen due to stagnant liquid part of the blood). All these signs (symptoms) of heart failure usually become noticeable in the evening, when the body is as “tired” as possible after everything it has done during the day. Unfortunately, post-infarction heart failure, along with the progression of atherosclerosis of the coronary arteries and subsequent myocardial infarctions, does not increase the life expectancy of patients with coronary artery disease.
Non-fatal complications of myocardial infarction are various disturbances in the conduction of the heart impulse (blockade), which sometimes requires the installation of a temporary pacemaker. Sometimes, on the contrary, after myocardial infarction various arrhythmias appear that require appropriate antiarrhythmic therapy (treatment). In patients who have suffered a transmural myocardial infarction, in approximately 30% of cases [9], non-infectious inflammation of the heart sac or membrane (pericardium) is observed - pericarditis. It manifests itself as short-term pain in the heart area, usually with a deep breath. The duration of pericarditis during myocardial infarction is usually 3-5 days.
There is another rare complication of myocardial infarction - the so-called Dressler syndrome. (A syndrome is a collection of symptoms or signs of a disease.) It occurs days, weeks and even months after a myocardial infarction. Dressler's syndrome is a response of the body's immune system to tissues of its own heart that have changed as a result of a myocardial infarction. This complication manifests itself as non-infectious pericarditis, as well as non-infectious inflammation of the outer membrane of the lungs (pleurisy) and other tissues. Treatment for Dressler syndrome is medication.
Unstable angina
Unstable angina (synonyms: progressive, variant) is a borderline state between ordinary (stable) exertional angina and myocardial infarction. It is characterized by an increase in frequency and severity of angina attacks. Sometimes unstable angina is also called a pre-infarction condition. Attacks of angina pectoris with this type of coronary artery disease occur at lower loads than before, at rest or at night. Unstable angina, as a rule, is based on the same thrombosis of the coronary arteries as in myocardial infarction, only reversible. Unlike myocardial infarction, with unstable angina, a small lumen remains in the affected artery and blood still flows through it beyond the site of thrombosis. But this amount of blood is still not enough for the myocardium supplied by this artery, which leads to more frequent and worsening pain attacks. Unstable angina will certainly resolve either towards stable exertional angina or towards myocardial infarction. According to American scientists, approximately a third of patients with unstable angina will develop myocardial infarction within 3 months from the moment of its onset in the absence of appropriate treatment [9]. That is why unstable angina requires active inpatient treatment, both medicinal and surgical. Diagnosis of the disease is the same as for myocardial infarction.
Vasospastic angina
Vasospastic angina (synonyms: Prinzmetal's angina, spontaneous angina) is a condition caused by involuntary contraction (spasm), often of large coronary arteries, unchanged by atherosclerosis. Spasm of the coronary arteries leads to myocardial ischemia, which is manifested by angina pectoris. Vasospastic angina usually affects young people. A painful attack most often occurs in the early morning hours, sometimes it is accompanied by cardiac arrhythmias and usually goes away after taking nitroglycerin or nifedipine. Outside of an attack, the ECG in such individuals does not differ from the ECG of healthy people. Holter ECG monitoring can help in diagnosing the disease. This disease can only be reliably diagnosed using drug provocation (ergonovine test). To prevent attacks of vasospastic angina, medications that dilate the coronary arteries, for example, nifedipine, are prescribed. A prolonged attack of vasospastic angina can result in myocardial infarction. SYNDROME X Syndrome X (X) is a condition manifested by angina pectoris. The complaints of patients and the results of instrumental diagnostic methods are the same as with typical angina pectoris. What distinguishes these two diseases is that in syndrome X, coronary angiography does not reveal any changes in the coronary arteries. This is explained by the fact that syndrome X is caused by spasm of small coronary arteries not visible on a coronary angiogram. The final diagnosis is established by exclusion.
Sudden cardiogenic death
This term refers to sudden death caused by heart disease (from the Greek words kardia - “heart” and genesis - “origin, occurrence” [2]). In approximately 20% of cases, sudden cardiogenic (cardiac) death is the first and only manifestation of coronary artery disease [9]. Typically, patients with severe damage to the coronary arteries and severe cardiac dysfunction die. The immediate cause of death is sudden blockage of the coronary arteries, accompanied by life-threatening arrhythmia (ventricular fibrillation). As mentioned above, in the absence of timely treatment, ventricular fibrillation always ends in death. The diagnosis of IHD in deceased patients can be suspected by questioning relatives, and confirmed during a pathological examination.
Bypass pipeline
If blood flow cannot be restored using such a minimally traumatic method as coronary angioplasty, then they resort to open surgery - coronary artery bypass surgery. In this case, veins or arteries taken from other parts of the body are brought from the aorta, the main blood supply, to the arteries of the heart, so as to bypass (bypass) the area of narrowing or blockage. Similar methods can be used in the treatment of angina pectoris. Moreover, in developed countries they are already widely used. The advantage of surgical methods over medication is that they quickly and completely eliminate the symptoms of the disease.
Light at the end of the vessel
We can say that there is a certain category of people in whom the presence of atherosclerosis is very likely. In the vast majority of cases, narrowing of the coronary arteries occurs due to the development of deposits on the walls of the vessel - atherosclerotic plaques - narrowing its lumen. Increased blood cholesterol levels, a hereditary predisposition to cardiovascular diseases, excess weight, smoking, hypertension, diabetes mellitus are risk factors for atherosclerosis.
Bypass surgery, angioplasty or medications
Which method is better - coronary bypass surgery, coronary angioplasty or drug treatment? Each of these methods has its own indications. Sometimes it is necessary to use different treatment methods at different stages. Of course, drug prevention and therapy are necessary in almost all cases. Coronary angioplasty can also be used successfully in most patients. Briefly, treatment methods for ischemic heart disease can be grouped as follows:
- Medicines . Some of them are necessary to reduce blood cholesterol or high blood pressure. Other medications help people with angina avoid attacks during exercise. Some drugs prevent heart rhythm disturbances that often accompany coronary artery disease. A number of drugs are necessary for the prevention of heart failure after myocardial infarction;
- Thrombolytic therapy . This type of treatment is used to eliminate a blood clot in acute myocardial infarction, when blood flow is obstructed by a blood clot. Thrombolytic agents dissolve clots and restore patency of the coronary artery. Thrombolytic therapy is often combined with angioplasty;
- Angioplasty is a method of expanding the internal lumen of blood vessels using a special balloon. In this case, through a small puncture, the doctor inserts a thin tube (catheter) and brings it to the narrowed area of the vessel, monitoring the process using x-rays. The balloon, expanding under pressure, pushes apart and flattens atherosclerotic plaques, creating conditions for normal blood flow. In some cases, after this, a metal frame is installed - a stent, which, being implanted into the wall of the artery, does not allow it to narrow again.
- Bypass operation . During bypass surgery, a new blood supply is created that bypasses the blocked section of the artery. Shunts are usually created from the patient's own vein or artery, for example from the patient's leg. Bypass surgery is usually performed surgically, although more gentle, non-surgical bypass methods have recently been developed.
All these techniques have been successfully used for many years by doctors at the Center’s Cardiovascular Surgery Department. In this case, proprietary developments are used, including a unique vascular stent developed by the head of the department Z.A. Kavteladze and his employees and now produced by WILLIAM COOK (USA).
Coronary heart disease, angina pectoris and rules of life
Coronary heart disease, angina pectoris and rules of lifeUsually a well-functioning heart is practically undisturbed, but there may come a time when the heart suddenly makes itself felt.
Most often this is associated with the development of a serious disease – coronary heart disease.
What is coronary heart disease?
IHD - coronary heart disease (angina pectoris, unstable angina, myocardial infarction) - is a consequence of narrowing and blockage of the main arteries of the heart with atherosclerotic plaques. Over time, there are more and more of them, and when the lumen of the vessel is blocked by 50% or more, difficulty in blood flow occurs. As a result, the delivery of oxygen and nutrients to the heart muscle decreases, oxygen starvation (hypoxia) develops, which leads to myocardial ischemia. The larger the size of the atherosclerotic plaque, the smaller the lumen of the vessel and the less blood flows through it, the more pronounced the myocardial hypoxia, which means the more pronounced ischemia (angina).
If, due to physical activity or emotional stress, you experience pain or a feeling of pressure or heaviness behind the sternum, you have a high probability of having angina pectoris (formerly called angina pectoris).
It is strongly recommended that you be examined by a cardiologist or physician.
Know that an attack of angina can be triggered by exercise, emotional stress, cold air and smoking.
Under the influence of these external influences, the pulse (heart rate) increases and blood pressure (BP) increases, which entails an increase in the myocardial oxygen demand against the background of a decrease in its delivery to the heart cells, thus developing myocardial ischemia, which the patient feels as angina pectoris.
How to diagnose angina?
The diagnosis of coronary artery disease and angina is made on the basis of a thorough survey and complaints.
To confirm the diagnosis and clarify the severity of the disease, additional methods are needed:
— taking an electrocardiogram (ECG) at rest and at the height of an attack
— carrying out stress tests (treadle test or test on a bicycle ergometer)
— according to indications (in case of high pulse, abnormal heart rhythm), 24-hour ECG recording is performed (Holter ECG monitoring)
— Sometimes coronary angiography (contrast study of the arteries of the heart) is required.
Warning signs of angina development:
— sudden discomfort, pain, or burning sensation;
— Pain can be triggered by walking, any physical activity, anxiety, emotional stress, cold air, smoking, less often pain appears at rest;
— pain most often occurs behind the sternum, but can radiate (radiate) to the left arm, left half of the lower jaw, teeth, shoulder, back or upper abdomen;
— pain occurs predominantly in the form of mild attacks (3-5 minutes), attacks can be repeated with varying frequency;
— usually the pain disappears 2-3 minutes after stopping walking or other physical activity, or taking nitroglycerin;
— attacks of angina may intensify with increased blood pressure, smoking, late intake or withdrawal of medications.
Types of angina:
V If your attacks appear during the day after the same load, with the same frequency and are of the same type, then you have stable angina.
V If your attacks become more frequent, occur with less stress and even at rest, become stronger, more severe and last longer, and are poorly controlled by the usual dose of nitroglycerin, then you should suspect unstable angina .
You need urgent medical consultation.
V If the pain becomes more intense and lasts for more than 15 minutes, repeats in waves at rest and does not go away after taking three nitroglycerin tablets, there is severe weakness and a feeling of fear, blood pressure and pulse fluctuate sharply, then you should suspect myocardial infarction. In this situation, urgent consultation with a doctor and immediate call for emergency medical assistance is necessary!
To improve your well-being and prevent the development or further progression of IHD, determine whether you have risk factors.
Factors that increase your risk of developing CHD
(check your risk factors):
Factors you cannot control
[] age/gender: men over 45 years old, women over 55 years old
[] early development of IHD in close relatives: - in men under 55 years of age, - in women under 65 years of age
Factors you can control
[] elevated blood pressure
[] smoking
[] elevated blood cholesterol levels
[] elevated blood glucose levels (diabetes)
[] excessive alcohol consumption
[] passive lifestyle
[] overweight
[] stressful situations
Inform your doctor about the risk factors you have identified and ask for advice on what you should do to correct them and subsequently control them well.
Treatment of coronary artery disease and angina has two goals:
the first is to improve the prognosis and prevent the occurrence of serious complications - myocardial infarction, sudden death - and prolong life;
the second is to reduce the severity of clinical symptoms - the frequency and intensity of angina attacks and, thus, improve the quality of life.
You should:
* learn to stop an attack of angina:
— interrupt the load, stop,
— take nitroglycerin under the tongue;
* be informed:
— about the potential undesirable effects of nitrates,
— about the possibility of developing hypotension after taking nitroglycerin;
— about the need to immediately call an ambulance if an angina attack persists at rest and/or is not relieved by nitroglycerin for more than 15-20 minutes;
— about the nature of angina, the mechanism of its development and the significance of this disease in the prognosis of life and recommended methods of treatment and prevention,
* to prevent an attack of angina, take nitrates (nitroglycerin) before exercise, which usually leads to angina.
How can you reduce the high likelihood of progression of coronary artery disease, angina,
as well as the development of serious cardiovascular complications
(myocardial infarction, unstable angina, sudden death, heart failure, cerebral stroke)?
STEP 1 relieving an attack of angina
If you have an angina attack:
V stop physical activity, stop walking, sit down, calm down and relax,
V put one nitroglycerin tablet under the tongue or use nitroglycerin in the form of a spray,
V Before taking nitroglycerin, you should sit down, because the drug may cause dizziness or decreased blood pressure,
V crush the nitroglycerin tablet and let the tablet dissolve completely; if the pain does not stop, then after 3-5 minutes repeat taking nitroglycerin either in the form of a tablet (up to 3 tablets) or in the form of a spray (spraying into the mouth up to 3 times)
V If an attack of angina cannot be relieved within 15 minutes after taking 3 tablets of nitroglycerin, you should immediately seek emergency medical help, and immediately chew 1 tablet of aspirin with water (aspirin prevents the formation of a blood clot). You may be developing a myocardial infarction!
REMEMBER!
You should always have a sufficient number of nitroglycerin tablets with you and they should always be at hand, no matter where you are at the moment!
STEP 2 regular blood pressure checks
People with elevated blood pressure levels and untreated developed myocardial infarction in 68 out of 100 cases and cerebral stroke in 75 out of 100 cases.
Monitor blood pressure levels carefully:
* at least once a year – with a single unstable increase in blood pressure discovered by chance;
* at least once a month - if you feel well, but have a tendency to frequently increase blood pressure;
* at least 2 times a day – in case of exacerbation, poor health, stable increase in blood pressure
Aim for a blood pressure level below 140/90 mmHg.
If you have suffered a myocardial infarction, suffer from angina pectoris, intermittent claudication, then strive for a lower blood pressure level - below 130/80 mm Hg.
In people with good blood pressure control:
* 42% fewer brain strokes;
* 20% less lethal and other serious cardiovascular complications (myocardial infarction, unstable angina, sudden death);
* 50% less heart failure;
* 14% fewer deaths from any other non-cardiac cause.
STEP 3 regular monitoring of cholesterol levels in the blood
Check your blood cholesterol levels and, if they are elevated, discuss with your doctor the possibility of taking cholesterol-lowering medications.
Criteria for optimal lipid levels in the majority of patients with coronary artery disease, patients who have had myocardial infarction, or surgery on the vessels of the heart, carotid arteries or arteries of the lower extremities:
* Total cholesterol - less than 4.0 mmol/l
* LDL cholesterol – less than 1.8 mmol/l
* Triglycerides – less than 1.7 mmol/l
* HDL cholesterol – for Men – 1.0 mmol/l or more
* HDL cholesterol - for Women - 1.2 mmol/l or more
STEP 4 heart rate control
In case of coronary artery disease, angina pectoris, or after a myocardial infarction, it is very important to control the pulse rate (heartbeat).
The optimal heart rate should be between 55-60 beats per minute.
This optimal heart rate is usually maintained with special medications prescribed by the attending physician.
STEP 5 proper nutrition
Change your eating pattern: eat healthy foods with less animal fat (60-105 g/day for men and 45-75 g/day for women) and rich in vegetables, fruits, complex carbohydrates, dietary fiber, fish.
Exclude from the diet: fatty meats, strong meat broths, any fat, sausages (even the so-called doctor's ones!), sausages, ready-made dumplings, canned meat, mayonnaise, internal organs of animals, brains, caviar, butter, hard margarine, fatty cottage cheese , cream cakes, creamy ice cream.
STEP 6 more movements
Move more and be physically active (at least 30 minutes of moderate exercise on most days of the week). If you have heart problems and are taking medications, talk to your doctor before changing your level of physical activity.
If you have been physically inactive for a long time, or if you are over 40 years old, or have angina pectoris, then the mode and level of physical activity should be determined by your doctor or physical therapy specialist, determining the pulse safety zone.
Physical activity is useful: aerobic, dynamic and moderate intensity - cycling, measured walking, swimming, team sports (football, volleyball), etc.
Optimal training walking tempo (number of steps per minute) depending on physical load tolerance (according to a load test on a bicycle ergometer)
Amount of load performed
during bicycle ergometer test, W 50 75 100 125
Function class
angina III II II I
Optimal pace
number of steps per minute 99-102 105-108 111-114 118-121
(or average) or 100 or 105 or 110 or 120
STEP 7 monitor the status of other risk factors
> Monitor your weight and measure your waist circumference (a waist circumference greater than 102 cm for men and greater than 88 cm for women indicates abdominal obesity, which is associated with a risk of cardiovascular complications).
> Stop smoking.
> Learn to control your psycho-emotional stress (avoid conflict situations, devote time to auto-training and relaxation methods).
> Maintain normal blood glucose levels: < 6 mmol/L (110 mg/dL)
STEP 8 Take medications prescribed by your doctor regularly
Today, the doctor has at his disposal a sufficient number of highly effective and safe drugs to reduce high blood pressure, prevent angina pectoris and prevent the development of serious cardiovascular complications.
REMEMBER!
Interruptions in taking medications reduce the effectiveness of preventing the development of myocardial infarction, unstable angina, and heart failure.
For the treatment of coronary artery disease and angina pectoris, different classes of medications are used today, the action of which is aimed at preventing the development of myocardial ischemia and angina attacks, vascular thrombosis, preventing the progression of atherosclerosis, reducing blood pressure and pulse rate (heart rate).
Take medication as directed by your doctor!
If the disease, despite active drug therapy, progresses, it is necessary to use modern interventional and surgical methods to restore blood supply to the myocardium:
V balloon angioplasty – expansion of the vessel at the site of stenosis by inflating the balloon
V stenting of the coronary arteries - installation of a special stent (tube) that allows for a long time to expand the artery of the heart and ensure normal blood flow
V coronary artery bypass grafting is used for a certain localization of atheromatous plaque and significant and multiple narrowing of the coronary vessel, when the first two methods are not effective
MAIN!
Treatment of coronary heart disease through lifestyle changes and highly effective medications prescribed by a doctor must be constant, long-term and daily.
STEP 9 keep a self-monitoring diary
A self-monitoring diary must be kept in order to promptly notice negative changes in the course of the disease and immediately contact your doctor.
The diary should record: blood pressure level, pulse rate, number of angina attacks, amount of nitroglycerin in the form of tablets or spray inhalations that were taken to relieve (relieve) an angina attack or prophylactically, for example, before physical activity, going outside to prevent it development.
The diary will allow you and your attending physician to evaluate the effectiveness of treatment, prevent exacerbation of the disease and, if necessary, correct therapy.
IF YOU FOLLOW THESE RULES AND MANAGE YOUR LIFE SMARTLY, YOUR ILLNESS WILL ALWAYS BE UNDER GOOD CONTROL!
Provocative diagnosis
If a person has several risk factors for ischemic heart disease, further examination is necessary to find out whether the person is experiencing ischemia or not. To do this, various so-called “provocative tests” are carried out, for example, tests with physical activity. By comparing the parameters of the heart at rest and under heavy loads, a conclusion is made about the need for further examination. At the next stage, a study of the heart vessels is usually performed - coronary angiography. Provocative tests, drug tests, and coronary angiography are included in the extensive arsenal of diagnostic methods of our clinic’s specialists. Based on the results of coronary angiography, the doctor chooses treatment tactics. After such a comprehensive examination, you can quite accurately predict the risk of a heart attack and take the necessary measures to prevent it.
REMOVAL OF ANGINE ATTACKS
Angina can manifest itself in different ways, and the complaints of different people often differ. The main symptom is sudden chest pain, although patients describe it differently. This may be a feeling of discomfort, a burning sensation, aching, bursting or squeezing pain that radiates to the left arm, under the left shoulder blade, to the stomach, back, neck, jaw, throat, and rarely to the right arm. The attack usually lasts from 1 to 15 minutes.
Most often, pain occurs during fast walking, when climbing stairs, when leaving a warm room in the cold, during severe anxiety, or if you had a bad dream. An attack can occur not only during stress, but also at rest. Nocturnal attacks of angina pectoris are often observed. In this situation, a spasm of the large coronary vessels that pass along the surface of the heart occurs. Rest angina is a more severe form of the disease.
To relieve an attack of angina, you must:
A) stop physical activity, eliminate other factors that provoke angina pectoris; If an attack occurs while walking or other physical activity, then you need to stop and give yourself a rest. If possible, it is better to sit or lie down comfortably. Sometimes these measures are quite enough to relieve an attack.
B) take a sublingual nitroglycerin tablet or capsule. It is possible to use aerosol forms of nitroglycerin or isosorbide dinitrate specially designed to relieve angina attacks;
C) if there is no effect from the first dose of nitroglycerin taken, its administration can be repeated twice with an interval of 5 minutes. Prescribing nitroglycerin in this regimen requires mandatory monitoring of blood pressure, since it can provoke severe hypotension.
It is best to take nitroglycerin at the very beginning of pain, but not at its height. In this case, the medicine may not have the desired effect.
Nitroglycerin also has its side effects, including headache, dizziness, noise and a feeling of fullness in the head, short-term palpitations. In some cases, fainting and very rarely collapse may develop.
Validol, Valocordin, Corvalol are not very effective in these cases and only create a favorable sedative background.
D) In addition to nitroglycerin, you can put an aspirin tablet under your tongue.
An attack of angina is a very alarming signal, and to avoid dangerous consequences, visit a therapist as soon as possible.
It is important to know! First aid for angina pectoris should be provided as soon as possible. If after 20 minutes the pain has not subsided, you must call an ambulance. If even one attack has been recorded, it is necessary to be constantly monitored by a doctor, who will prescribe further treatment and tell you how to prevent angina pectoris.