What is angina?
In Russia, the classification given in the Clinical Guidelines of the Ministry of Health for Coronary Heart Disease of 2021 has been adopted. According to this classification, angina occurs:
- voltage, stable, indicating functional class (FC);
- vasospastic (other names - spontaneous, variant, Prinzmetal's angina);
- microvascular.
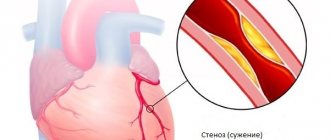
In the International Classification of Diseases, 10th revision (ICD-10), in addition to the above-mentioned options, there is also unstable angina, which can be either new or progressive. This type is usually mentioned in cases of progression of coronary insufficiency. The greater the degree of stenosis of the coronary arteries, the more severe the attacks will be
Angina pectoris: general information
If, as you age, you begin to notice that heart pain occurs after physical activity, immediately consult a cardiologist. There is a high probability that you are developing a heart disease called angina pectoris FC 2. Attacks of pain pass, so many people tend to ignore them. However, the result and direct consequence is myocardial infarction. An even worse option: sudden cardiac arrest. Do not expose yourself to mortal risk - get examined using professional diagnostic equipment at the first symptoms of angina pectoris! Now you have a unique opportunity to undergo a free consultation with a specialist and a set of preparatory examinations when enrolling in a course of enhanced external counterpulsation or shock wave therapy of the heart:
Promotion
Just until the end of autumn, undergo a free consultation and a set of preparatory examinations* when registering for a course of enhanced external counterpulsation or shock wave therapy of the heart.**
Send a request
* Check the details of the Promotion by phone. **Has contraindications; consultation with a doctor is required.
Enhanced external counterpulsation (EECP) Cardiac shock wave therapy (SWTS)
Hurry up to apply, the promotion period is limited.
How to distinguish the types of angina from each other
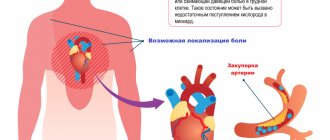
The main symptom of any type of this condition is pressing, squeezing pain in the left side of the chest, which can “radiate” to the left side of the face, neck, shoulder or shoulder blade.
Stable exertional angina
An attack of pain in the heart that occurs as a result of a decrease in arterial blood flow to the myocardium during exercise or stress. A decrease in blood supply to the heart muscle leads to a sharp decrease in the amount of oxygen supplied to the heart, which causes pain.
Signs of stable angina pectoris
- An attack is triggered by physical or emotional stress.
- Duration - from two to five minutes.
- The pain goes away after the action of the factor that caused it ceases or after taking nitrates.
Sometimes atypical manifestations are possible - shortness of breath (increased breathing rate), a feeling of suffocation, a burning sensation or heat in the chest.
The severity depends on the functional class (FC):
- 1st FC - attacks occur only with excessive stress;
- 2nd FC - attacks occur during normal exertion: fast walking, climbing stairs (more than two flights), after a heavy meal, stress;
- 3rd FC - attacks occur with minor exertion: walking at an average pace, climbing 1-2 flights of stairs;
- 4th FC - attacks occur at rest.
New or acute angina
After the first attack occurs, and up to three months after it, they speak of new-onset angina. During this period, the doctor draws conclusions about the severity of the pathology (determines the functional class) and the prognosis - the possibility of transition to unstable angina. In an acute attack, symptoms can range from mild to severe.
Unstable angina
Progressive exertional angina, or unstable angina, is said to occur when:
- the number of attacks increases;
- attacks appear at rest or after a heavy meal;
- the duration of attacks increases (up to 15-20 minutes or more);
- response to nitroglycerin decreases.
Progressive angina may precede myocardial infarction.
Vasospastic or variant angina
This type is spoken of when an attack occurs for no apparent reason - when it cannot be associated with the action of provoking factors. The cause of myocardial ischemia is a sudden spasm of the coronary arteries. More often, attacks of variant (vasospastic) angina occur in older women and occur at night or in the morning. Taking nitroglycerin is ineffective.
Microvascular angina
The clinical picture is no different from exertional angina. This diagnosis is made only after functional and instrumental research methods - echocardiography (ultrasound of the heart), coronary angiography or CT angiography. Based on the results of these studies, one can judge the condition of the coronary vessels. The main difference between microvascular angina and other types is the absence of damage to the coronary arteries.
Giving up bad habits, dosed physical activity and other prevention methods help prevent or delay the onset of any type of angina. Once diagnosed, angina requires treatment regardless of type
Publications in the media
Variant angina is angina characterized by the appearance of pain at rest and accompanied by a transient rise in the ST segment. This type of angina is caused by transient spasm of the coronary arteries, so it usually occurs unrelated to physical activity. Statistical data. The prevalence is unknown, but the disease appears to be quite rare.
Etiology and pathogenesis • The tone of the coronary vessels depends on the balance of vasodilator and vasoconstrictor factors. Vasodilating factors include nitric oxide (NO), the so-called endogenous relaxing factor. In the presence of atherosclerosis and hypercholesterolemia, the production of this factor by the endothelium apparently decreases, or it breaks down to a greater extent, i.e. endothelial vasodilator function decreases. This leads to an increase in the activity of vasoconstrictor agents, which contributes to the development of spasm of the coronary arteries. Severe spasm causes transmural ischemia, which is characterized by dyskinesia of the left ventricular wall, detected by echocardiography, and ST segment elevation on the ECG • Variant angina can occur with stable angina pectoris in 50% of patients. Its appearance is often noted in patients in the acute period of myocardial infarction, as well as after coronary artery bypass surgery and percutaneous transluminal coronary angioplasty.
Clinical manifestations • Typical anginal pain behind the sternum, occurring more often at night or in the early morning hours, the duration of the attack can be more than 15 minutes. Sublingual administration of nitroglycerin in most cases stops an attack of variant angina. The appearance of pain at night or early in the morning without connection with external factors is typical • At the height of pain, the appearance of ventricular arrhythmias or AV blockades is possible. Fainting due to ventricular arrhythmias or AV block may be diagnostic of variant angina • A characteristic associated symptom is migraine, which occurs in 25% of patients. In 25% of patients, variant angina is combined with Raynaud's phenomenon • The disease can occur in waves - after several attacks, a long period of remission is possible, and then resumption of attacks of variant angina.
Instrumental data • If it is possible to record an ECG during a painful attack, an elevation of the ST segment is recorded (usually in several leads at once), and its return to the baseline after relief of the pain syndrome • Daily ECG monitoring can also reveal episodes of ST segment elevation • ECG during a test with physical load provokes angina pectoris with ST segment elevation in 30% of patients in the active phase of the disease • Provocative tests: cold, test with hyperventilation, pharmacological tests with dopamine, acetylcholine. A cold test can detect an attack of angina and ECG changes in 10% of patients (place the hand up to the middle of the forearm in water at a temperature of +4 ° C for 3–5 minutes; the test is considered positive if ischemic changes appear on the ECG during immersion or over the next 10 minutes ) • Coronary angiography allows you to identify transient local spasm of the coronary artery, usually located at the site of atherosclerotic lesion (and regardless of the degree of its severity).
TREATMENT
Drug therapy • Sublingual nitroglycerin is used to relieve an attack of variant angina. In case of exacerbation of the disease (increased frequency of attacks), it is possible to use long-acting nitrates: isosorbide mononitrate is prescribed in a dose of 10-40 mg 2-4 times / day, and retard forms - 40-120 mg 1-2 times / day • Slow calcium blockers may be recommended channels - long-acting preparations of nifedipine (10–30 mg/day), verapamil (480 mg/day), diltiazem (360 mg/day). A combination of nifedipine and verapamil, nifedipine and diltiazem is possible, as well as a triple combination: long-acting nitrates + 2 slow calcium channel blockers • There has been a positive effect of using a-blockers, amiodarone, guanethidine, clonidine in case of variant angina • b-blockers can prolong an attack of variant angina, therefore, they are not indicated for this category of patients • For patients with variant angina, as with other forms of coronary artery disease, the use of acetylsalicylic acid is indicated for the prevention of MI.
Surgery. If severe atherosclerotic narrowing of the arteries is detected by coronary angiography, coronary bypass grafting or balloon dilatation is recommended. However, there is evidence that rates of operative mortality and postoperative MI in patients with variant angina are higher than in patients without variant angina.
Forecast. Spontaneous remission (disappearance of attacks) occurs quite often, sometimes lasting for years. A number of patients develop MI within 3 months. To a large extent, the prognosis of patients with variant angina is influenced by the severity of atherosclerosis of the coronary arteries.
Synonyms. Prinzmetal's angina • Vasospastic angina • Spontaneous angina.
ICD-10 • I20.8 Other forms of angina
Angina at rest: signs and symptoms
It is characterized by the manifestation of characteristic symptoms in a calm state - at night and especially in the morning after waking up. Typically, angina at rest is diagnosed using 24-hour monitoring. Most often, attacks are caused by increased blood pressure and psycho-emotional stress. Unfortunately, any troubles at work or family quarrel can provoke an attack. And sometimes it is enough to change the position of the body.
This type includes vasospastic angina, the cause of which is a sudden spasm of the coronary vessels. And also post-infarction - manifesting itself 10-14 days after the heart attack.
Symptoms of angina in women and men
Pain
Most patients report the following symptoms of an angina attack. First of all, cutting, pressing pain in the chest. Many people complain that their heart “burns” or their throat “tightens.” At the same time, you instinctively want to press your hand or fist to your chest. Often the pain migrates to the left shoulder, neck, arm, and shoulder blade. It may grow or disappear suddenly. Symptoms clearly and distinctly appear during exercise, when the patient is diagnosed with IHD angina pectoris FC 2.
Pain can occur after physical exertion, stress, high blood pressure, or overeating. At night - due to stuffiness or low air temperature. Often the attack is accompanied by arrhythmia.
External symptoms and signs of angina pectoris
It is quite simple to identify an attack by its external manifestations. Pay attention to the following signs of angina: the person turns pale, sweat appears on the forehead, his face expresses suffering; fingers lose sensitivity, hands become cold; the patient breathes intermittently and rarely; the onset of an attack is accompanied by a rapid pulse.