Angina pectoris, or as it is colloquially called “angina pectoris,” is one of the forms of coronary heart disease (CHD). Manifests itself in the form of pressing, squeezing or burning pain in the chest area. Pain can spread to the left arm, lower jaw, neck, and left subscapular region.
An attack of pain can be triggered by:
- physical activity (even if you just walked quickly or climbed the stairs);
- increased blood pressure;
- rapid heartbeat;
- inhaling cold air;
- emotional overstrain;
- an overly filling lunch.
Usually the pain goes away after a few minutes if you sit or lie down quietly, or after 2-3 minutes if you take nitroglycerin under the tongue.
What is angina
Angina pectoris is a specific pain syndrome characteristic of myocardial ischemia. There are stable and unstable angina, as well as exertional and resting angina.
Stable angina is one that occurs in an unchanged form. We can say that this is a “habitual” symptomatology for a person. However, this situation cannot be considered the norm: serious treatment is required, often surgical.
Unstable angina is either angina that has arisen for the first time, or one where the nature of the pain syndrome and sensations differs significantly from the usual state. This is an extremely dangerous condition, fraught with a high risk of developing a heart attack, and requiring an immediate call to the ambulance.
Angina pectoris is one of the manifestations of atherosclerosis and coronary heart disease, which is manifested by severe chest pain during physical activity and stress. However, chest pain is not always a manifestation of angina.
It is important to note symptoms such as:
- squeezing, pressing or burning nature of the attack;
- impact under the left shoulder blade or in the arm, neck, lower jaw;
- lack of oxygen and dizziness;
- obvious interruptions in the functioning of the heart: fluctuations in heart rate and blood pressure.
Most often, pain with angina pectoris manifests itself during walking, climbing stairs, physical effort, and stress. The attack lasts from 1 to 15-20 minutes and is facilitated by taking nitroglycerin. Symptoms may appear all at once or separately.
Angina at rest, unlike the previous type, is characterized by a sudden and prolonged attack, which is activated without external provoking factors, sometimes during sleep. In this case, we can add to the main symptoms: an uncontrollable panic attack, a pronounced feeling of suffocation, a violation of the autonomic functions of the body. We will write more about this type of angina in the following articles.
In addition to extremely unpleasant symptoms, such manifestations indicate a high risk of myocardial infarction, as well as the development of heart failure.
Cardiovascular diseases claim half of human lives - exactly the same as all other causes combined.
Reminder for patients suffering from angina pectoris
When the patient unites with the disease, the doctor is powerless; if the patient fights his illness together with the doctor, the disease recedes
What is angina?
Angina pectoris is the most common form of coronary heart disease, manifested by attacks of chest pain. Pain of a squeezing, pressing or burning nature, which occurs during physical or psycho-emotional stress, is localized behind the sternum and can be transmitted under the left shoulder blade, to the left arm, neck or lower jaw. As a rule, the pain goes away with rest or after taking nitroglycerin.
What are the causes of angina?
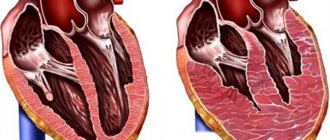
The main cause of angina is atherosclerosis - a narrowing of the coronary (coronary) arteries of the heart that supply the heart with blood. Atherosclerosis is the accumulation of cholesterol and other substances in the vascular wall, which, forming so-called atherosclerotic plaques, narrow the lumen of the vessel. Sometimes an attack of angina can cause a spasm - a sharp narrowing of the coronary artery due to tension in the muscle layer of the vessel wall. During physical or emotional stress, the heart contracts more often and more strongly, requiring more oxygen and nutrients, but due to the narrowing of the coronary vessels, the heart's need for oxygen is not satisfied. Ischemia occurs - oxygen starvation of the heart. The heart gives an alarm signal and pain occurs.
Why is angina pectoris dangerous?
A prolonged uncontrolled attack of angina can develop into myocardial infarction - a serious and dangerous disease. Therefore, it is necessary to follow the doctor’s recommendations to avoid situations that provoke an attack and to stop it in a timely manner. Remember that by changing your lifestyle and taking highly effective medications, you can prevent the occurrence of angina attacks, reduce the risk of developing myocardial infarction and thereby prolong your life. Treatment under the supervision of a physician should be long-term and irregular.
What can cause an angina attack?
- Increased physical activity
- Emotional stress
- Increased blood pressure
- Exposure to cold
- Smoking
What to do if you have an angina attack?
- Stop physical activity
- Sit down
- Take a nitroglycerin tablet under the tongue or inject one or two doses of nitroglycerin aerosol (Nitromint or another similar drug) onto the tongue.
- if after 5-7 minutes the pain has passed, take a second nitroglycerin tablet or inject one or two doses of nitroglycerin aerosol onto the tongue and call emergency medical assistance by phone. 103
How to deal with angina pectoris
- elimination of clinical symptoms (pain)
- prevention of myocardial infarction
- increasing the quality and duration of the patient using medications, if indicated, interventional cardiac surgical methods for treating the disease.
Causes of angina
The cause of angina is the partial blocking of the lumen of the arteries by atherosclerotic plaques, resulting in severe oxygen starvation of the heart cells, which causes pain. An additional role is played by vasospasm, which can be provoked, for example, by nervous strain or sudden exposure to cold.
It is the presence of atherosclerotic plaques that is the leading factor in the development of angina pectoris. The development of coronary heart disease is a complex and multicomponent process, which is provoked and accelerated due to risk factors:
- arterial hypertension,
- smoking, obesity,
- cholesterol metabolism disorder,
- diabetes,
- low physical activity and poor nutrition.
In the case of atherosclerosis, angina begins to manifest itself when an atherosclerotic plaque fills the artery by more than 50% - preventing the normal passage of blood through the heart and, accordingly, the saturation of the heart muscle with oxygen. This leads to the development of an imbalance in the functioning of the heart.
With physical and psycho-emotional stress, the situation worsens. The heart begins to work more actively - it contracts more often and stronger. In this state, it requires more oxygen and nutrients. However, due to vasoconstriction, this need is not satisfied, which leads to oxygen starvation and, as a result, pain.
We feel pain thanks to the instinct of self-preservation. She is a kind of alarm signal. Therefore, any pain attack is a rational reason to consult a doctor.
Rehabilitation for angina pectoris
Home page › Medical rehabilitation › Rehabilitation for angina pectoris
Angina pectoris is one of the forms of coronary heart disease. It usually manifests itself in attacks of sudden pain in the chest area and shortness of breath. The danger of angina lies in patients’ neglect of the precise instructions of the attending physician. This often leads to the development of acute myocardial infarction and even death, because angina pectoris is the last step before serious heart damage. Postponing treatment of angina pectoris indefinitely is guaranteed to lead to the development of severe complications.
Rehabilitation after angina pectoris in the medical rehabilitation department will prevent the risk of myocardial infarction and chronic heart failure. Timely contact with specialists in 80 percent of cases allows you to stop the course of the disease and achieve a full recovery.
The Vorovsky sanatorium is one of the well-established sanatorium and resort institutions in Russia in the cardiovascular field with many years of work. Patients undergoing rehabilitation programs for angina pectoris are offered comprehensive and systematic courses of treatment, which are based on solving the following problems:
- Identify and neutralize the cause of the attacks;
- Reduce the risks of complications;
- Develop an individual control plan during the course of an attack;
- To achieve restoration of the patient’s physical activity;
- If possible, get rid of the disease and prevent the risks of occurrence.
Rehabilitation after angina pectoris in the medical rehabilitation department is divided into several periods:
- Primary examination and diagnosis;
- Determination of the components of the course of treatment;
- Gradual restoration of physical parameters.
During rehabilitation after angina pectoris, the following methods are used at the Vorovsky sanatorium:
- Daily diagnostic program;
- Suggestive therapy;
- Physical therapy complex;
- Diet therapy;
- Climatotherapy;
- Water procedures (swimming, showers, baths);
- Massage;
- Drug treatment;
- Physiotherapy.
An integrated approach to the prevention, treatment and rehabilitation after angina pectoris allows you to achieve a prolonged effect and get rid of the symptoms of the disease in the shortest possible time. Particular attention is paid to systematic and comprehensive diagnostics; this approach allows you to monitor all progressive and regressive reactions in real time, promptly change loads and adjust the course of treatment.
Contraindications to visiting a sanatorium-resort establishment are:
- Acute infectious and inflammatory processes;
- Malignant neoplasms;
- Aortic dissection;
- Angina pectoris type III-IV;
- The need for surgical intervention.
The Vorovsky sanatorium is open to visitors all year round. Well-groomed territory, comfortable rooms, attentive staff, a varied menu and a rich entertainment program will turn treatment into relaxation. The sanatorium provides a complex of cosmetology and restorative programs for patients and their accompanying persons.
Send the discharge summary by email: [email protected] .
Risk factors and their control
Angina pectoris and the disease that causes it require not only the fastest possible treatment, but also control of risk factors. These include:
- Hyperlipidemia - imbalance in cholesterol metabolism. It is characterized by an increased concentration of low-density lipoproteins and fatty acids - triglycerides. And also by lowering the level of high-density lipoproteins - “good” cholesterol.
It is observed in most patients with angina pectoris. Reducing cholesterol levels in the body helps reduce the number of attacks.
- Obesity - characterized by a body mass index of more than 26 and, often, occurs due to constant poor nutrition: consumption of high-calorie foods high in animal fats, cholesterol and “fast” carbohydrates, such as sugar and flour. And, on the contrary, a lack of vegetables, fruits, whole grains, legumes, and herbs in the diet.
In addition, large body weight increases the load on the heart, increasing the risk of an attack. To control this factor, it is necessary to adhere to the principles of rational or therapeutic nutrition: limit the consumption of cholesterol, animal fats, processed foods and salt. Increase your consumption of vegetables, fruits and other whole plant foods containing fiber, natural antioxidants, polyphenols, and flavonoids.
Excess body weight is usually just the “tip of the iceberg”. This is a manifestation of serious imbalances in the functioning of the body.
- Physical inactivity - insufficient physical activity, combined with poor nutrition, contributes to the risk of obesity and cholesterol accumulation. Together, these factors contribute to the development and frequency of angina pectoris.
- Arterial hypertension - is a frequent companion to coronary heart disease, which, in itself, implies oxygen deficiency of the myocardium. When blood pressure rises, myocardial tension occurs, causing the heart to have an even greater need for oxygen. This provokes an attack of angina pectoris.
Controlling blood pressure will help keep the heart and blood vessels relatively calm - reducing the frequency and power of attacks.
- Anemia is not a risk factor, but a condition that aggravates the course and makes it difficult to control IHD. It is characterized by a decreased level of hemoglobin and a general weakening of the body. This results in the impossibility of sufficiently supplying the heart with oxygen. Controlling the normal level of hemoglobin in the blood helps alleviate the course of the disease: for women the norm is 120-150 g/l, for men - 135-165 g/l.
- Tobacco addiction - smoking increases several risk factors at once: it causes oxygen starvation, increases blood pressure and causes spasms of the arteries. The habit harms a healthy body, and in the presence of atherosclerosis it leads to early manifestations of angina pectoris and significantly increases the risk of acute myocardial infarction.
- Diabetes mellitus type 2. This disease seriously worsens the course and prognosis of IHD. We will devote a separate article to this condition, but for now we draw attention to it as a serious risk factor.
The combination of 2 or more items from the list, even weakly expressed ones, increases oxygen starvation of the heart, and, accordingly, the risk of developing and the severity of symptoms of angina pectoris. The presence of risk factors should be taken into account when determining treatment tactics and secondary prevention of angina pectoris.
Diagnosis of angina pectoris
To diagnose angina pectoris, as well as exclude other possible diseases, complaints and the nature of pain are analyzed, laboratory blood tests and a functional examination of the heart are performed, and the patient’s physical condition is analyzed.
It is also important to determine the severity and severity of the process. To do this, if a diagnosis of acute coronary syndrome is made, a study of the vascular bed of the heart is performed - coronary angiography. Based on the results, the question of surgery or intravascular intervention is decided.
Laboratory blood diagnostics help determine the level of:
- total cholesterol and lipid fractions,
- high and low density lipoproteins,
- triglycerides,
- creatine kinase,
- glucose,
- markers of systemic inflammation (SII),
- indicators of the coagulation system - coagulograms,
- electrolytes,
- troponin - in acute situations.
Particular attention in the study is paid to the presence of cardiac troponins I and T - markers that indicate myocardial damage. Their presence confirms that the patient is suffering a microinfarction or acute myocardial infarction.
Functional research methods allow you to determine the condition of the heart:
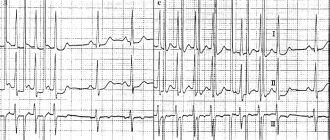
- ECG - examination at the peak of an angina attack determines conduction and rhythm disturbances. Signs of myocardial oxygen starvation may also be detected.
- Daily ECG monitoring - records the level of oxygen starvation during an attack of angina, heart rate, arrhythmia. Indicators help determine the specific diagnosis and stage of the disease.
- EchoCG - reveals local ischemic changes and disorders of myocardial contractility.
- Bicycle ergometry or treadmill - determines the maximum possible physical activity for the patient without the threat of developing ischemia. The load is set using an exercise bike or treadmill, and the results are recorded by an ECG device.
- Stress echocardiography (Stress-ECHO) is a study of myocardial contractility using the ultrasound method, under conditions of dosed physical activity. At the same time, an ECG is recorded. Allows you to make a primary diagnosis of IHD and clarify indications for surgical treatment.
For a detailed study of the vascular bed of the heart, the following are used:
- Coronary angiography is an X-ray method in which a contrast agent is injected into the arteries of the heart using a special catheter.
- multislice computed tomography is a type of computed tomography in which X-ray “slices” of the heart and blood vessels are obtained at high speed. More than 100 such “slices” can be performed between contractions of the heart chambers.
These studies allow us to obtain information about the state of the vascular bed of the heart: which arteries are passable, which are completely or partially blocked, and in what place. Based on the information received, the doctor makes a decision about whether the patient has coronary artery disease, the need for surgical intervention and the timing of treatment.
I 20.0 – Unstable angina – example of writing a call card
Patient, 64 years old
Reason for calling – Chest pain (history of coronary artery disease)
Complaints, medical history
Complaints of general weakness, pressing pain behind the sternum, burning sensation radiating to the left shoulder, back (between the shoulder blades), sweating, feeling of lack of air.
The feeling worsened for about 6 hours, the pain arose at rest, intensified with the slightest physical activity, short-term relief after taking isoket spray. I took isoket spray about 10 doses, bisoprolol 10 mg, lisinopril 10 mg, cardiomagnyl 1 tablet. This is not the first time this condition has happened; he was previously treated as an inpatient. During physical activity, she notes infrequent short-term attacks of chest pain, which are relieved with rest after taking nitrates, after 5-10 minutes.
Anamnesis of life
Hypertension stage III. IBS. PEAKS (2012). Diabetes mellitus type II. Cerebrovascular disease.
Regularly takes enalapril 10 mg/day, bisoprolol 10 mg/day, cardiomagnyl 1 tablet/day, maninil 1 tablet/day.
Comfortable blood pressure – 140/90
Physical examination
Condition: moderate;
Consciousness – clear, Glasgow scale – 15 points, behavior – calm;
Pupils – normal, D = S, reaction to light – lively, no gaze paresis, no nystagmus;
Skin – pale, dry, clean;
Heart sounds are muffled, rhythmic, no murmurs. The pulse in the peripheral arteries is of satisfactory quality, rhythmic;
Nervous system – without pathology, no meningeal symptoms;
The pharynx is calm, the tonsils are normal;
Excursion of the chest - normal, type of breathing - normal, percussion - pulmonary sound, auscultation - vesicular breathing, no shortness of breath;
There is no peripheral edema;
The tongue is clean and moist. The abdomen is soft, painless, participates in the act of breathing, there are no symptoms of peritoneal irritation, the liver is not enlarged, stool is formed, 1 time per day;
Urine output is normal, SSPO is negative.
Main pathology
Consciousness is preserved, the patient is adequate. The skin is pale and dry. Heart sounds are muffled and rhythmic. The pulse in the peripheral arteries is of satisfactory quality, rhythmic.
| time | 15-30 | 15-50 | 16-10 | 16-30 | Etc. peace |
| NPV | 18 | 16 | 16 | 16 | 16 |
| Pulse | 86 | 64 | 66 | 64 | 62 |
| Heart rate | 86 | 64 | 66 | 64 | 62 |
| HELL | 160/100 | 150/90 | 140/90 | 140/90 | 140/90 |
| Pace. ºС | 36,6 | ||||
| SpO2 | 95 | 98 | 98 | 98 | 98 |
Blood glucose – 6.5 mmol/l
Troponin test – negative
Electrocardiography
15-35 – Sinus rhythm 86 per minute. Signs of left ventricular hypertrophy. Signs of subepicardial damage to the anterior wall (ST depression I, II, aVL, V1-V4 1-2 mm). Negative dynamics with previous ECGs.
15-50 – Sinus rhythm 64 per minute. No dynamics from the previous ECG.
16-30 – Sinus rhythm 64 per minute. No dynamics from the previous ECG.
Diagnosis by the EMS team
IBS. Unstable angina III B (Braunwald). Post-infarction cardiosclerosis.
Therapeutic measures
- oxygen inhalation through nasal catheters
- 15-36 – peripheral vein catheterization
- 15-37 – Isoket spray s/l 1 dose every 5 minutes – 4 doses (no effect)
- 15-38 – Tav. Acidi acetylsalicylici 250 mg p/os
- 15-38 – Tav. Plavix 300 mg p/os
- 15-39 – Sol. Clexani 4000 ED IV
- 15-42 – Sol. Betaloc 10 mg IV
- 15-45 – Sol. Morphini hydrochloride 1% – 1 ml intravenously in fractions
- ECG monitoring
- hospitalization on a stretcher to the regional vascular center.
Treatment result
Improvement. The pain syndrome was relieved by the administration of morphine and did not recur during transportation.
Treatment of angina
Angina pectoris is an accompanying factor of coronary heart disease, so the main fight must be waged against it. Treatment of angina pectoris is aimed at relieving and preventing attacks and complications.
The first priority when an attack occurs is to take nitroglycerin. It helps relieve pain. If the attack does not stop, nitroglycerin can be used again. Drug therapy involves your doctor prescribing anti-ischemic drugs that help the heart cope with low oxygen levels. Anti-sclerotic drugs, antioxidants and antiplatelet agents are also prescribed.
Based on the diagnosis, a decision is made on additional treatment for cardiac conduction and rhythm disorders. For angina pectoris, surgical intervention is often prescribed: balloon angioplasty, stenting, coronary artery bypass grafting.