Silent myocardial ischemia
Silent ischemia is based on a discrepancy between the myocardial oxygen demand and the actual perfusion of the heart muscle. Under the influence of certain reasons (emotional stress, physical activity, etc.), cardiomyocytes begin to feel oxygen starvation and compensatoryly switch to an oxygen-free type of energy synthesis - anaerobic glycolysis. This type of glucose metabolism leads to rapid energy depletion of cells and the accumulation of compounds that normally irritate nerve endings that are involved in the formation of the sensation of pain in the cerebral cortex. With BBIM this sensation does not occur. There are several pathogenetic hypotheses, but none of them fully explains the mechanism of development of painless attacks.
The painlessness of ischemic episodes is associated with reduced sensitivity of intracardial nerve endings due to diabetic neuropathy, partial death of neurons during infarction, and the effects of drugs and toxins. The paradox is that painless ischemia also occurs in relatively healthy individuals who do not have a history of factors that can reliably disrupt the conduction of nerve fibers of the heart (without a heart attack, other cardiovascular events, diabetes, chronic or acute intoxication).
The absence of pain is also associated with insufficient strength and duration of myocardial ischemia. It has been experimentally proven that ischemia causes pain only when certain threshold values are reached - for a duration of at least 3 minutes. However, cases of anginal pain with minimal manifestations of ischemia and, conversely, the absence of any symptoms with extensive long-term disturbances in cardiac muscle perfusion are also known.
“Silent” ischemia is also explained by a failure in the formation of pain sensations due to a decrease in the number of intramuscular receptors for adenosine (the main activator of pain receptors released during cardiac ischemia) or a decrease in the sensitivity of these same receptors to it. However, it is impossible to reliably establish exactly how the number of receptors changes from the onset of the disease to the moment the patient seeks help. It is also unclear why, with the same concentration of adenosine, in some cases the ischemia is “silent”, while in others it is accompanied by pain.
The absence of pain is also associated with an increase in the activity of the anti-pain system, which has a neurohumoral regulation mechanism. Reduction of pain due to activation of the nervous component is realized by increased activity of the reticular formation and thalamus in the brain. The humoral component is manifested by an increase in the plasma concentration of natural opioids - endorphins, which reduce susceptibility to pain. It has been established that patients with BBIM have a higher level of endorphins in the blood plasma both after exercise and at rest than patients with clinical manifestations of ischemia.
Publications in the media
Silent myocardial ischemia is a condition in which the presence of ECG signs of myocardial ischemia is not accompanied by pain. One of the forms of IHD. Statistical data. Episodes of silent myocardial ischemia are detected in almost all patients with unstable angina and in 40% of patients with stable angina. Silent myocardial ischemia occurs more often in older people with diabetes.
The etiology and pathogenesis are similar to those of stable angina pectoris
• Episodes of painful and silent myocardial ischemia can be observed in the same patient with the same degree of atherosclerosis of the coronary arteries.
• The reasons for the absence of pain during ischemia are currently unclear •• A possible mechanism for the occurrence of painless myocardial ischemia is considered to be a change in the level of the pain threshold (its variability) •• In patients with diabetes, the main cause of painless myocardial ischemia is damage to the autonomic nervous system of the heart (neuropathy).
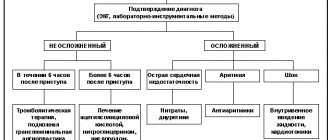
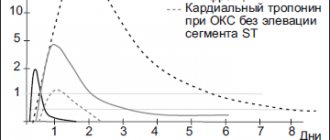
Diagnostics. The main method is daily ECG monitoring. It is recommended for patients with a high functional class of stable angina pectoris, unstable angina and post-infarction cardiosclerosis, as well as persons without clinical manifestations of coronary artery disease in the presence of several risk factors simultaneously. In a number of patients, ST segment elevation on the ECG can be detected during exercise testing, as well as during stress echocardiography.
Treatment. In the presence of a clinical picture of exertional angina, unstable angina or isolated painless myocardial ischemia (without clinical manifestations of coronary artery disease), treatment is carried out using generally accepted methods and means (acetylsalicylic acid, nitrates, beta-blockers, slow calcium channel blockers). The effectiveness of treatment is assessed based on 24-hour ECG monitoring or exercise testing.
Prognosis • A positive stress test with ECG in patients with silent myocardial ischemia may indicate a poor prognosis (high risk of developing MI, sudden cardiac death, severe angina pectoris) • Detection of episodes of silent myocardial ischemia in patients after a previous MI indicates a higher risk of developing recurrent MI • The combination of episodes of silent myocardial ischemia with cardiac arrhythmias, especially ventricular extrasystole, is regarded as a harbinger of possible sudden death.
Synonym. "Silent" myocardial ischemia.
ICD-10 • I25.6 Asymptomatic myocardial ischemia.
Diagnostics
Daily ECG monitoring is considered an important diagnostic method. It is recommended for patients with unstable angina, functional class of stable angina pectoris, post-infarction cardiosclerosis. Also used if there is no IHD clinic, but there are several risk factors. In some cases, it is possible to detect elevation of the 5T segment on the ECG by performing an exercise test. A diagnostic method such as stress echocardiography is also relevant.
Etiology and pathogenesis
The etiology and pathogenesis are the same as for stable angina pectoris. The reasons for the absence of pain during ischemia remain questionable. Episodes of painful and silent myocardial ischemia can be recorded in the same person with the same degree of atherosclerosis of the coronary arteries. It is assumed that the mechanism of development of the condition in question is a change in the level of the pain threshold. In diabetes mellitus, the cause of silent myocardial ischemia is damage to the autonomic nervous system of the heart, which is called neuropathy in the medical literature.
Forecast
If a stress test is positive (with an ECG) in people diagnosed with silent myocardial ischemia (SMI), this indicates a poor prognosis. There is a high risk of myocardial infarction. There may be cardiac death. This also indicates severe exertional angina. The discovery of cases of silent myocardial ischemia in patients after a heart attack indicates a higher risk of developing a recurrence of acute myocardial infarction. If episodes of BMI are combined with cardiac arrhythmias, especially ventricular extrasystole, then sudden death is very high.
Epidemiology
Cases of silent myocardial ischemia are found in almost 100% of patients diagnosed with “unstable angina” and in less than half of those with stable angina pectoris. If there is no angina pectoris, typical signs of myocardial ischemia on the ECG are recorded in those who have atherosclerotic lesions of the coronary arteries in 15% of cases, according to information obtained by daily ECG monitoring. Elderly people diagnosed with diabetes are at risk.
Treatment
In cases of unstable angina, exertional angina, isolated painless myocardial ischemia (without clinical coronary heart disease), therapy should be carried out using generally accepted means and methods. The following drugs have an effect:
- nitrates,
- p-blockers,
- acetylsalicylic acid,
- slow calcium channel blockers.
The effectiveness of the prescribed therapy should be assessed based on the data obtained from daily ECG monitoring or from the tests mentioned above.
Myocardial infarction
Heart attack
To this day, people sometimes hear, mainly from people of the older generation, something like the following popular cardiological phrases: “This way you can get a heart attack, that is, heart rupture” (usually meaning shock from surprise or, say, from good news).
We bow to our indestructible grandfathers and grandmothers, and may all the news only bring joy to their tired hearts. However, given the exceptional importance of the topic, it is still worth making certainty in the terminology.
A heart attack is not a rupture of the heart. Moreover, we are not even necessarily talking specifically about the heart: no sweeter, say, an infarction of the brain or spinal cord, an infarction of the kidney or intestines.
And the definition that one of the largest search engines on the Internet gives to a heart attack with automatic importunity: “... cessation of blood flow due to spasm of the arteries or their blockage” is also incorrect. A heart attack is not a “cessation of blood flow,” but the result of such a cessation; the result is always pathological and, as a rule, severe.
Therefore, we will strive for accuracy of definitions and clarity of formulations. The topic is really too serious.
Any living tissue, as we know, consists of cells. For normal operation and effective performance of their functions, these cells must breathe, eat and get rid of waste products of metabolism (metabolism). All these processes are ensured by blood flow or, more precisely, by perfusion - constant “impregnation”, through the flow of blood through the tissue, for which the system of capillaries, the smallest blood vessels, is responsible. Arterial blood enters the capillary system, bringing nutrients and oxygen bound by red blood cells to the tissue. Then, through the small, large and main veins, the blood is drained to the lungs, liver, kidneys - for a new cycle of filtration, detoxification, enrichment and gas exchange.
The pumping function, that is, pumping blood under pressure through this complex vascular system, is performed by the heart muscle, or myocardium. The contractile activity of the heart begins in the womb, in the first weeks of pregnancy, and continues non-stop until the last minute of a person’s life. The opposite is also true: the last minute occurs due to the fact that the rhythmic alternation of contractions (systole) and relaxations (diastole) stops.
However, the myocardium, as a hollow pumping muscle (which is anatomically and histologically very complex) consists of living tissues that also need nutrition and oxygen. In this sense, the myocardium is no different from other organs: it itself needs tissue perfusion of blood, continuous and quite intense, given its lifelong work 24/7 without weekends or holidays. The blood supply to the heart is carried out through a special arterial-venous circuit. Due to its external resemblance to the attribute of monarchy, the myocardial circulation is called coronary, or coronary.
Insufficient volume of blood flow through tissue (any tissue, not just the heart) is called hypoperfusion. The widely known term “ischemia” was interpreted differently at different stages of the development of medicine; Today, ischemia is understood as a pathological state of tissue that develops as a result of hypoperfusion, and the obligate (mandatory for the use of the term or diagnosis) signs of ischemia are violations of all the basic processes provided by the tissue blood supply - nutrition, oxygenation (oxygen saturation) and waste removal.
Thus, coronary heart disease (CHD) is chronic starvation and/or “clogging” of myocardial tissue, caused by insufficient functioning of the coronary circulatory circuit. There are many known risk factors and direct causes of the development of ischemic heart disease, as well as its clinical variants, but now something else is more important: this situation inevitably leads to overload, premature wear, degenerative-dystrophic changes in tissues and various malfunctions in the functioning of the heart muscle (for example, attacks angina). In conditions of constant ischemia, the myocardium, brain, kidney and any other organ simply cannot fully perform their functions - just as an athlete who is suffocating and living from hand to mouth will not be able to engage in professional sports.
A heart attack is a simultaneous mass death of cells in a local area of tissue. In other words, this is rapid focal necrosis, occurring as a result of a sharp reduction in blood supply (incomplete ischemia) or a complete cessation of perfusion (total ischemia).
Myocardial infarction is the death of one or more areas of the heart muscle, which occurs due to the fact that coronary blood has stopped circulating in these areas.
A wealth of information is now available regarding myocardial infarction. It is not always, as shown above, reliable and accurate, but in any case it is better than a complete misunderstanding of the normal and pathological processes occurring in one’s own body. We will not dwell on the details of epidemiology here, but we will briefly note the four most significant and alarming points.
Firstly, cardiovascular diseases (primarily ischemic heart disease and heart attacks) stubbornly hold the lead in statistical indicators of non-violent mortality: their share in the overall mortality structure, according to WHO estimates, exceeds 30%.
Secondly, the mortality rate in Russia is two and a half times higher than the European average; three times higher than in the USA; nine times higher than in Japan.
Thirdly, heart attacks are constantly “getting younger”: the average age of primary patients with coronary artery disease and heart attacks is steadily decreasing from year to year.
Fourth, 80% of myocardial infarctions were preventable.