Vegetovascular dystonia is a pathological condition in which the functioning of the autonomic nervous system is disrupted. Patients with this syndrome are often diagnosed with changes in the cardiovascular system, which is manifested, among other things, by periodic attacks of tachycardia. The patient's heart rate increases to 90 beats per minute or more, weakness and dizziness, a feeling of fear and anxiety also occur. However, in most cases, all symptoms disappear before the doctors arrive, and they disappear as suddenly as they begin. Treatment is based on maintaining a healthy lifestyle, monitoring the patient’s psychological state, and periodically taking medications.
Physiological aspects of vegetative-vascular dystonia
Vegetovascular dystonia is a common diagnosis. Normally, the heart works as an autonomous mechanism, constantly providing blood flow through the vessels. The frequency, strength and rhythm of heart contractions are regulated by the myocardial conduction system, endocrine glands and the autonomic nervous system. Together, these mechanisms ensure proper functioning of the heart muscle both at rest and during physical activity.
The autonomic nervous system is divided into sympathetic and parasympathetic divisions. When the first one is excited, the pulse rate increases, while the second one decreases. Tachycardia with VSD is associated with excessive activation of the sympathetic nervous system and at the same time inhibition of the parasympathetic, resulting in an imbalance.
REFERENCE! The work of the heart is also influenced by external factors. Thus, under conditions of hypoxia and after exercise, a slight acceleration of the heart rate is considered normal. Tachycardia, which needs to be eliminated with medication, is indicated by a rapid, up to 90 beats per minute, pulse in a state of complete rest.
Features of treatment and first aid
Having identified symptoms of tachycardia arising from VSD, the patient should consult a cardiologist. The specialist will prescribe a series of examinations to exclude other diseases. After diagnosis, a treatment regimen is drawn up based on the course of the disease. It mainly includes medications, psychotherapy sessions and traditional medicine.
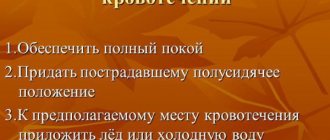
If the attack has already begun, then you need to remember the following algorithm of actions:
- postpone the work being done;
- try to calm down and not think about the bad;
- find a well-ventilated area;
- lie down with a cold object on your forehead.
To get rid of paroxysm faster, the following methods are suitable:
- take quick deep breaths and exhale 2 times slower;
- hold your breath, keeping your abdominal muscles tense;
- lightly press your finger on the root of the tongue to induce vomiting;
- hold your head under running cold water;
- apply force to the angle of the lower jaw;
- use sedative drops (Valerian, Corvalol);
If there is a lack of air, it is recommended to breathe for 10 minutes into a paper bag. If you cannot fight the attack and it progresses, then you need to call an ambulance.
Drug course of treatment
Drug treatment of tachycardia with VSD consists of taking effective sedative and antiarrhythmic drugs. You can see their features below:
- Tablets based on herbs with a sedative effect (hawthorn, motherwort, valerian, peppermint, lemon balm) are inexpensive and publicly available. The effect they have helps reduce nervous tension and normalize pulse and blood pressure. The advantage of such medications is the small number of contraindications and side effects, due to which they are used for a long time. You can purchase herbal preparations at any pharmacy without a doctor's prescription.
- Medicines with a sedative effect, made from chemical compounds, are more effective (Relanum, Prazepam). Doctors recommend using such remedies when you are often in stressful situations. They have an extensive list of adverse reactions, but have a pronounced calming effect, due to which the heart rate decreases and blood pressure stabilizes. Most types of these pills are prescribed by prescription.
- Drugs with an antiarrhythmic effect are used as a means of eliminating tachycardia. They stabilize the heart rhythm and prevent relapses. The downside of these medications is a large number of contraindications.
Medicines from the above groups are prescribed by the attending physician, focusing on the course of the disease. How to get rid of tachycardia during VSD using antiarrhythmic drugs? The following groups will help:
- Beta blockers reduce the effect of adrenaline on the heart muscle by blocking its receptors. They are cardioselective (Betacard, Betoftan, Corbis) and non-selective (Obzidan, Sotalol, Niolol). Medicines from the first group act on beta-1 adrenergic receptors, which are located in the heart muscle. Their blocking contributes to a drop in blood pressure and a decrease in heart rate. Non-selective drugs affect beta-1 and 2 adrenergic receptors. The impact is similar to the first group. The downside of these tablets is the increased risk of developing bronchospasm. In case of VSD, you can limit yourself to cardioselective blockers, since beta-2 receptors are localized in the bronchi and there is no need to affect them.
- Potassium channel blockers prevent the element from entering the heart cells, as a result of which electrical activity slows down, pressure drops and the severity of tachycardia decreases. The most relevant among them is Amiodarone. The drug has a small number of contraindications; it is successfully used to treat arrhythmia and high blood pressure in combination with heart failure. The downside of the drug is the high risk of developing adverse reactions (weakness, decreased visual acuity, thyroid dysfunction) with long-term use.
Medicines with an antiarrhythmic effect are prescribed not to eliminate the cause of the failure, but to stop tachycardia and prevent the development of complications. The following remedies can help reduce nervous tension and improve heart function:
- Nootropic medications (“Piracetam”, “Pantogam”, “Phenibut”) are used to increase the patient’s resistance to stressful situations, physical and mental overload and other external factors. Taking them will improve cognitive abilities and restore the balance between the sympathetic and parasympathetic departments, which will lead to the elimination of the cause of tachycardia.
- Daytime tranquilizers (Prazepam, Trimetozin, Gidazepam) cope well with attacks of panic and unreasonable fear. After taking them, sleep improves and nervous excitability decreases. Unlike simple tranquilizers, medications from this subgroup have a more pronounced anti-anxiety effect and are less sedative and hypnotic. Patients are able to take the medication during the day and do their daily work without causing discomfort drowsiness. By reducing tension in the nervous system, the influence of the sympathetic department is reduced and tachycardia is eliminated.
Frequent paroxysms of tachycardia gradually exhaust the heart. To prevent the development of complications, doctors advise combining sedatives and antiarrhythmic drugs with vitamin complexes:
- "Ascorutin" is rich in ascorbic acid and rutin. It is recommended to be used to normalize metabolic processes, strengthen the walls of blood vessels and the immune system.
- “Napravit” contains a high concentration of B vitamins, magnesium, potassium and other elements vital for the stable functioning of the heart and nervous system. If you take the pills for a long time, you can stop the development of atherosclerosis and complications caused by tachycardia.
- “Asparkam” is valued for the large amount of potassium and magnesium in its composition. Doctors recommend the drug to eliminate arrhythmia, improve cardiac patency and stabilize electrolyte balance. To increase effectiveness, it can be combined with antiarrhythmic drugs.
Psychotherapy
Tachycardia resulting from vegetative-vascular dystonia is effectively eliminated by treating mental problems. Psychotherapy will help solve the problem. Its essence is to improve the emotional state and increase the patient's resistance to stress to prevent attacks. The sessions are conducted by an experienced psychotherapist.
Stabilization of the condition is observed no earlier than the 5th visit to the doctor. In total, it is advisable to undergo at least 10 sessions so that the specialist can reduce the impact of factors affecting the patient’s psyche. In advanced cases, to improve the therapeutic effect, psychotherapy is combined with medications that have a sedative, antiarrhythmic and anti-anxiety effect.
Physiotherapy
Nervous tension, which is often the cause of the development of VSD, can be eliminated using physiotherapy methods:
- acupuncture;
- electropheresis;
- breathing exercises;
- back massage;
- healing baths;
- magnetic laser therapy.
ethnoscience
Increased heart rate caused by vegetative-vascular dystonia can be stopped using traditional medicine methods. They virtually do not cause adverse reactions and have a minimal number of contraindications, therefore they are in demand in the treatment of many pathologies. The list of the most effective recipes is below:
- Hibiscus tea is an aromatic drink made from the Sudanese rose. It has a pronounced sedative effect, due to which the heart rate decreases. Prepare a decoction by pouring 2 buds with 1 cup of boiling water. You can drink 1-2 cups of it every day.
- Collections of medicinal herbs are sold in virtually any pharmacy. They have a sedative, hypotensive and vasodilating effect. You can make the medicine yourself by collecting all the ingredients in the required quantity. To prepare the decoction, you will need to pour 50 g of the collection with 450 ml of boiling water. Take it 50 ml 5 times a day for no more than 1 month.
- The needles are rich in phytoncides, which help reduce blood pressure and eliminate arrhythmia by reducing the heart rate. After completing the course of therapy, patients experience loss of insomnia and increased resistance to stress. You can add pine needles in the form of oils (juniper, pine) to the bath.
- Juniper stabilizes heart function and relieves nervous tension. It is enough to eat 1 berry per day, increasing the dosage by 1 piece. every day. After 2 weeks, take in reverse order. Continue treatment for 28 days.
- Hawthorn decoction can reduce the intensity of manifestations of VSD, reducing blood pressure and heart rate. To prepare, simply mix 30 g of the plant’s fruits with 1 cup of boiling water. Then leave the medicine to infuse. After 20 minutes you can drink it in the morning and evening, ½ cup.
- Honey is a valuable source of B vitamins and other beneficial substances. It can be added to a glass of milk in an amount of 25-30 ml to obtain a good medicine with a sedative effect. It is best to drink it before bed.
Prevention
Compliance with the rules of prevention will prevent the development of further attacks of tachycardia and improve the general condition. Their list is below:
- devote at least 7-8 hours of sleep a day;
- periodically take 5-minute breaks at work;
- adjust the daily menu;
- try to avoid conflicts;
- apply self-hypnosis techniques;
- exercise.
Tachycardia, manifested against the background of VSD, occurs quite often, especially in the presence of disruptions in the nervous and endocrine systems. Its sinus variety does not require special treatment, but more serious forms must be identified immediately so that they do not lead to the development of severe complications. Arrhythmia can be reduced with medications, folk remedies and psychotherapy sessions. The doctor should select a course of treatment, focusing on the main cause of the failure in the autonomic nervous system.
Tachycardia - definition and classification
Tachycardia is an increase in heart rate. Normally, this figure is 60-90 beats per minute, but can vary depending on many factors. So, a tall person or someone who is overweight needs more oxygen and nutrients, so the heart will beat faster. Also, the pulse increases after intense exercise and during the hot season, in rooms with insufficient ventilation. Pathological tachycardia is considered to be an increase in heart rate for no apparent reason, which is accompanied by additional symptoms.
There are several classifications of tachycardia with VSD. The first of them identifies several varieties of the syndrome depending on the cause of its occurrence:
- intracardial - develops as a result of cardiac dysfunction;
- extracardiac - rapid pulse is a symptom of pathologies not directly related to the work of the heart.
It is also necessary to distinguish between the main types of tachycardia depending on the location of the focus in which the impulse occurs:
- paroxysmal (ectopic) - can be ventricular, if the impulse originates in the ventricles, or supraventricular, if it originates in the atria;
- sinus - the impulse comes directly from the sinus node.
With vegetative-vascular dystonia, extracardiac tachycardia is characteristic, that is, an acceleration of the pulse does not indicate pathologies of the cardiovascular system. There are also several variants of manifestation of this syndrome:
- single attacks, in which the pulse rate can reach up to 120-240 beats per minute, but the indicators quickly normalize;
- constant tachycardia - at rest, the heart rate per minute is 90-120 beats, and symptoms may remain unnoticed for a long time;
- sinus - frequent increase in heart rate to 120-130 beats per minute.
If untreated, tachycardia with VSD is dangerous, despite the fact that there is no organic damage to the heart. An increase in the load on the myocardium over time can lead to progressive hypoxia (coronary heart disease), and also cause a heart attack or stroke.
When the heart rate increases, panic attacks often occur, but it is worth remembering that even significant tachycardia caused by VSD is safe for health
State of the cardiovascular system in pathology of the upper gastrointestinal tract
Diseases of the digestive system occupy an important place in the structure of general morbidity, representing an important economic, social and medical problem. The results of epidemiological studies indicate a change in the structure of the main diseases of the upper digestive tract: a decrease in the incidence of peptic ulcers and an increase in the number of patients with gastroesophageal reflux disease (GERD) in the world are noted. Currently, GERD is recognized as the leading disease in gastroenterology in terms of frequency.
In recent years, increasing attention has been paid to “extraesophageal” manifestations of GERD, including cardiac ones. Cardiac manifestations of GERD are of greatest interest from both a scientific and practical point of view. They can be in the form of chest pain not associated with coronary heart disease (CHD) (so-called “non-cardiac chest pain”) and disturbances in the rhythm and conduction of the heart. Based on clinical studies, it is assumed that GERD is the second most common cause of chest pain (after coronary artery disease), although the actual frequency in different populations is unknown. Such chest pain requires differential diagnosis with coronary heart disease using costly and invasive technologies. Thus, every year almost 600 thousand Americans undergo coronary angiography for chest pain, while no significant changes are found in 10–30% of those examined. Similar data (30%) are provided by domestic authors (V. A. Kuznetsov et al., 2000). Timely diagnosis of the esophageal cause of chest pain has both economic and social aspects. The fact is that diagnosis of GERD is often carried out only on the basis of endoscopic research methods. This is fundamentally wrong, since in 60% of cases GERD occurs as an endoscopically negative variant (when the endoscopist describes a normal esophagus, and reflux can be very pronounced), but it is with this variant that atypical (cardiac) symptoms are more often observed, significantly affecting the quality of life of patients . At the same time, in older people, GERD can be combined with coronary artery disease (the frequency of combinations and associated conditions requires study). In this case, the isolation of the esophageal component of pain and its competent correction dramatically facilitate the course of coronary artery disease and, accordingly, the quality of life of patients.
Despite the fact that over the past 20 years there has been a significant increase in the number of studies devoted to gastroesophageal reflux disease, the number of studies on the “cardiac” manifestations of GERD remains small, and the study of the arrhythmic aspects of GERD has not received due attention. All of the above was a prerequisite for studying the nature of lesions of the cardiovascular system in pathology of the esophagus and cardia.
The interaction between the gastrointestinal tract and the cardiovascular system is of undoubted interest. The proximity of the location to the heart and the common innervation are capable of provoking arrhythmias and simulating coronary artery disease in case of fullness of the stomach or pathology of the esophagus such as viscero-visceral reflexes. Pathology of the upper gastrointestinal tract can lead to functional disorders of the cardiovascular system, arising indirectly through the ANS. Most clinical manifestations of VSD, including changes in sinus rhythm and partly ectopic arrhythmias, depend on an imbalance of autonomic influences. Thus, there is no doubt about the significant role of neurovegetative influences on the heart, which, when imbalanced, contribute to the occurrence and maintenance of paroxysmal atrial fibrillation (SH Hohnloser, A. van de Loo, M. Zabel 1994; P. Coumel 1992; Yu. R. Sheikh-Zade, 1990; N. P. Potapova, G. G. Ivanov, N. A. Bulanova, 1997; S. G. Kanorsky, V. V. Sibitsky, 1999).
Gastrointestinal diseases play an important role in the occurrence of ANS dysregulation. Yu. V. Nyavyarauskus (dissertation, 1987) described an increase in the tone of the parasympathetic nervous system, coinciding with exacerbations of chronic diseases of internal organs (cholelithiasis, hiatal hernia (HH), PU). This gives reason to believe that primary diseases of the internal organs in such patients were the main etiopathogenetic factors contributing to the development of autonomic sinus node dysfunction (ASND).
In total, we examined 99 patients, of which: the first group - 35 patients with pathology of the esophagus and cardia (GERD and/or hiatal hernia); second group - 31 people with a combination of GERD and/or hiatal hernia with peptic ulcer; third group - 33 patients with ulcer (conditional comparison group). The average age was 37.0±10.1 years.
In our study, patients with ulcer were selected as a comparison group.
PU is considered the most striking example of psychosomatic diseases due to the fact that changes in the autonomic nervous system play a significant role both in the occurrence of the disease itself and its clinical course. Autonomic disorders occur in 75–82% of patients with ulcer (A. M. Vein). In this case, changes in the ANS act as a mechanism through which psychosomatic interactions are realized.
All patients underwent a complete clinical and instrumental examination during the exacerbation period and 6–8 weeks after standard therapy for the underlying disease.
The condition of the esophageal mucosa was assessed according to the modified classification of M. Savary & G. Miller (1994), taking into account the extent of inflammatory changes in the esophageal mucosa.
During polypositional fluoroscopic examination with contrast (barium sulfate), a hiatal hernia was diagnosed, its size and nature were determined according to the classification of V. Kh. Vasilenko and A. L. Grebenev (1978), and complicated forms of the disease (strictures, ulcers, tumors) were excluded ).
To verify GERD, all patients underwent 24-hour pH monitoring of the esophagus and stomach using the Gastroscan-24 apparatus (NPO Istok, Fryazino, Moscow region).
Ultrasound examination of the heart (UltraMark-9, Canada) made it possible to exclude valvular pathology, multiple accessory chordae, hemodynamically significant valve prolapse, scar changes in cardiac tissue, and signs of heart failure.
A quantitative and qualitative analysis of a standard ECG was carried out; with 24-hour ECG monitoring (Brentwood Holter System, Canada), the qualitative indicators of the ECG and the characteristics of heart rate variability were assessed.
To clarify the functional state of the sinus node and conduction system of the heart, to identify and identify cardiac arrhythmias, a non-invasive transesophageal electrophysiological study (EPS) of the heart was performed using the Elcart device (Tomsk, Russia).
The state of the ANS was determined using the standardized questionnaire by A. M. Vein (1985) “Questionnaire for identifying signs of vegetative changes.” Each symptom was assessed using a five-point system, and the predominance of sympathetic or parasympathetic influences was determined. In addition, the vegetative indices of Kerdo and Hildebrant and minute blood volume (MBV) were assessed.
Of the 68 patients with pathology of the esophagus and cardia, 89.7% complained of heartburn, 51.5% had epigastric discomfort, and 66.2% had epigastric pain. The presence of chest pain was noted by 20.6%; feeling of a “lump in the throat” - 7.4%; palpitations and interruptions in heart function - 10.3% of those examined. According to endoscopic examination, stage 0 reflux esophagitis (RE) was detected in 22.1% of patients, stage I in 42.6%, stage II in 35.3%. Hernia was radiologically diagnosed in 28 people, in most cases cardioesophageal (92.9%) and unfixed (60.7%).
The success of the therapy was assessed using 24-hour pH measurements and endoscopy. There were no significant intergroup differences in 24-hour pH measurements of the esophagus in patients from the main groups.
It should be noted that 11 patients underwent simultaneous 24-hour monitoring of pH and ECG. The purpose of the study is to conduct a differential diagnosis of esophageal pseudocoronary pain from other possible causes, to establish a symptom index, i.e., the coincidence of cardiac symptoms (chest pain, interruptions) with episodes of GER according to 24-hour pH measurements.
In 81.8% of cases, episodes of chest pain were associated with GER and were not accompanied by changes in the ECG. A positive symptomatic index was noted in 63.6% of patients.
During the treatment, the endoscopic picture improved: the proportion of erosive lesions of the esophagus, stage II ER, decreased from 35.3 to 2.9% and stage I ER, from 42.6 to 27.9%.
Initially, a normal ECG was recorded in 16 to 24% of those examined. Automatic function disorders were determined in 25.7–38.7% of those examined; conduction disorders - from 15 to 23% and a combination of these 2 disorders - in 13-23%, without significantly different in individual groups.
When comparing qualitative ECG indicators using the Pearson test, significant intergroup differences were noted only for intraventricular conduction disorders (IVDC): the presence of GERD increased its frequency compared to patients with peptic ulcer disease (χI = 6.171; p = 0.013). This applied to both “pure” GERD and its combinations with hiatus hernia and peptic ulcer (χI = 6.467; p = 0.011; χI = 4.728; p = 0.03, respectively).
Ectopic activity, detected on average in 6% of cases on a standard ECG, was recorded much more often with Holter monitoring (HM) of the ECG. At the same time, ectopic activity in the combination of GERD and ulcer was higher than in isolated ulcer (χI = 5.295; p = 0.021) due to extrasystole (χI = 4.28; p = 0.039). According to HM, there was an increase in heart rate (HR) (minimum, maximum, average; no more than 7%) after the course of treatment. No significant intergroup differences were obtained. Taking into account the qualitative parameters of the ECG and CM, we can conclude that intraventricular conduction disturbances occurred significantly more often in patients with reflux disease and in its combination with ulcer compared with the comparison group. In addition, ectopic activity, including supraventricular extrasystole, was more typical for patients with ulcerative disease and ulcerative disease. At the same time, in individuals with ectopic activity compared to those without it, there were no significant differences in EPI indicators (although only patients in the first and second groups had patients with a high Wenckebach point) and autonomic tone, while differences were noted in some spectral parameters. Thus, for maximum heart rate F = 6.911 (p = 0.011); LF F = 4.102 (p = 0.047); SDNN F = 4.288 (p = 0.042). It can be assumed that increased ectopic activity in patients with GERD is associated with a simultaneous increase in sympathetic and parasympathetic influences on the heart, which does not contradict the literature data, since such changes in heart rate variability (HRV) are considered potentially unfavorable. The most arrhythmogenic situation is with a simultaneous increase in the sympathetic and parasympathetic tone of the ANS (RD Riley, EL Pritchett, 1997).
There are epidemiological studies devoted to studying the frequency of cardiac arrhythmias and conduction disorders. Thus, N.G. Gogolashvili conducted a survey of 673 indigenous residents of the Republic of Sakha (82.1% of residents of 5 typical villages). According to standard ECG data, nomotopic arrhythmias were observed in 49.9%; heterotopia - in 6.7% of those examined; cardiac conduction disorders - 9.5%; heart block - 6.9%. The frequency of arrhythmias and conduction disorders in the Yakut population was as follows: sinus arrhythmia - 33.9%; sinus bradycardia - 12.8%; sinus tachycardia -3.2%; AVB - 3.9%; SAB - 0.2%; blockade of the right bundle branch (complete and incomplete occurred equally); ventricular extrasystole (1-2 gradations) - 4.2%; supraventricular extrasystole - 2.7%; atrial fibrillation - 0.9%. All cases of atrial fibrillation were studied at the age of 40 years and older. In 42.2% of those examined with heterotopic cardiac arrhythmias, heart disease could not be detected. In men aged 16 to 39 years, cardiovascular diseases were not detected at all. HM was carried out by random sampling in 174 people. With CM, as in our study, an increase in heterotopic activity was observed: for example, ventricular extrasystole was noted in 37.6% and supraventricular in 34.9%. Paroxysmal tachycardia (1.4% of cases) and atrial fibrillation (1.4% of cases) were most rarely detected. To diagnose DSU, 46 patients underwent transesophageal pacing. Autonomic dysfunction was observed in 1.9%; sick sinus syndrome in 0.7% of those examined. According to the Research Institute of Therapy of the Siberian Branch of the Russian Academy of Medical Sciences, when studying the prevalence of ECG changes in the unorganized population of Novosibirsk (1563 men and 1550 women aged 25–64 years), AV conduction disorders were recorded in 1.9% of men and 1.7% of women; NVHD - in 4.3% of men and 2.2% of women; complete block of the left bundle branch - 0.1%; arrhythmias in 7.2% of men and 3.5% of women; T wave changes - 4.9% and 6.2%, respectively.
Cardiac endoscopy was performed to evaluate the function of the sinus and atriventricular (AV) nodes. The initial data exceeded the normative values: VVFSUmax in 25.7%; 30.3% and 45.2% of the compared groups and KVVFSUavg. in 20%, 18.2% and 22.58%, respectively. Dysfunction of the sinus node of vegetative origin was detected in 25.7% of patients in the first group; 30.3% - second and 45.2% - comparison group. The peculiarities of the functioning of the AV conduction system were determined: in 1 patient (2.9%) of the first group and in 2 patients (6.1%) of the second group, the appearance of the Wenckebach point was noted at frequencies exceeding 180 imp/min. Intergroup differences were significant for the indicators VVFSUaverage, VVVFSUmin and VVFSUmax differed in patients of the first group (p < 0.05) and the second group (p < 0.01) compared with patients with ulcer, the Wenckebach point was different (p < 0.05) in patients of the first group from the comparison group and VVFSUmin in patients of the first and second groups (p < 0.05).
During the treatment, there was a significant decrease in the indicators of CVVFSUaverage. due to a decrease in VVFSUmax for all 3 study groups, as well as VVFSUmin and VVFSUmax in the second main group, which indirectly indicates a decrease in the parasympathetic influence of the VNS.
EPI indicators of sinus node function turned out to be normal in all groups of patients and did not exceed acceptable values after the course of therapy. After a course of prokinetic therapy, AV conduction parameters did not differ from acceptable values. VVFSUmin after the course of treatment was significantly higher in patients with ulcer than in patients with pathology of the esophagus and cardia (p < 0.05).
When studying the autonomic support of the cardiovascular system, a predominance of vagotonia was obtained in all groups according to the Wein questionnaire, Kerdo index and IOC. After treatment, there was a significant decrease in the initial parasympathicotonia and a significant change in the autonomic indicators that indicated the initial eutonia - QWm and the Hildebrant index, which confirms an increase in the activity of the sympathetic circuit. No intergroup differences were found. The results obtained do not contradict the literature data. Thus, F.I. Komarov showed that with a newly diagnosed peptic ulcer or its exacerbation in the first 2 weeks, the tone of the sympathetic section of the ANS, caused by pain, predominates. Then, as the pain syndrome is relieved, the functional activity of the SNS is sharply reduced and the tone of the PNS begins to predominate. Other Russian researchers (E.V. Minakov, M.M. Romanov, 1999) noted significant differences in HRV indicators in patients with ulcer with different courses. The majority of patients with newly diagnosed ulcers were characterized by sympathicotonia; in patients with a mild course, HRV indicators were within standard deviations of values. In moderate and severe patients, parasympathicotonia was observed at rest. The data obtained to some extent echo the theory
G. Beigman, who believed that the prerequisite for ulcer formation may be not so much damage to the vagus nerve, but rather a violation of the balanced influence on the gastrointestinal tract of both parts of the ANS. Siberian colleagues (E.I. Beloborodova et al., 2002) also studied the state of autonomic tone in patients with ulcer using cardiointervalography. At rest, with mild and moderate course, a decrease in the sympathetic component was noted, with a severe course - an increase. The authors concluded that psychophysiological characteristics correlate with the severity of peptic ulcer disease: the severity of autonomic and psychological disorders increases in proportion to the severity of the disease, reaching maximum levels in severe cases. It was proposed to use autonomic and psychological indicators as criteria for predicting the nature of the course of duodenal ulcer in young people.
Most heart rate variability indicators initially did not differ from normative values, except for RMSSD (p < 0.001). There were intergroup differences in only one indicator: iSDNN was significantly different in patients with a combination of GERD and PU from patients with isolated PU (p < 0.05).
Against the background of successful therapy of the underlying disease, a significant increase in iSDNN and PNN50 was noted; a decrease in iSDANN and normalization of RMSSD (p < 0.01) was observed in all studied groups.
Analysis of the frequency characteristics of HRV showed an initial excess of the normative values of ULF in patients with GERD and ulcer and LF in all groups and a decrease in VLF indicators, an increase in HF in pathology of the esophagus and cardia. After treatment, ULF and VLF indicators increased in all groups (p < 0.001), only the ultra-low frequency spectrum did not reach normal values. The initially elevated LF spectrum normalized during treatment (p < 0.001). A decrease in the high-frequency spectrum was noted (p < 0.001). Our data from the study of HRV in patients with ulcer did not differ from the results obtained by E. V. Minakov et al. Correlation and factor analysis performed in the patients we studied revealed fewer associated variables compared to the parameters presented. Thus, the time with pH < 4.0 in the esophagus (%) correlated only with the rMSSD indicator (-0.36*) only in patients with reflux disease. While the analysis revealed that HRV indicators were more influenced by factors such as minimum, maximum and average heart rate, although in some models the duration of GER, HRVFSUmax, and SBP level were also important. The results of a study of HRV in healthy and cardiac patients established the dependence of HRV indicators mainly on heart rate (I. S. Yavelov, N. A. Gratsiansky, 1999). There is evidence of a linear relationship between average heart rate and HRV indicators obtained both from daily ECG monitoring (healthy individuals) and from analysis of short sections of ECG recording (patients with unstable angina). In the study, the presence of this connection was confirmed for patients with GERD (HH). Apparently, this dependence has a general tendency, since there is an opinion that heart rhythm depends to a greater extent on autonomic regulation than on nosology. Of the HRV characteristics, the closest correlation was obtained for iSDNN and rMSSD. To the least extent, the minimum and maximum heart rate were associated with VLF values in the second group and indicators of functional activity of the sinus node (CVVFSUmax and VVFSUmax, QVm) rMSSD and LF in the third group.
Summarizing the results of the study of the ANS, obtained from the study of various autonomic indices and HRV, we can say that all the patients studied had signs of a mixed type of ANS imbalance. The dynamics of these parameters indicate a decrease in excessive sympathetic and parasympathetic influences and the restoration of the sympathetic-parasympathetic balance in the treatment of the underlying pathology. Thus, during treatment there was a small but significant increase in heart rate. One of the reasons for the decrease in parasympathetic activity could be the stabilization of the patients’ condition as a result of treatment of the underlying pathology. At the same time, the ratio of sympathetic and parasympathetic influences on sinus rhythm changed significantly towards harmonization of the influences of both sections of the ANS.
All of the above allows us to talk about the relationship between vegetative and electrophysiological changes, which, apparently, largely determines the state of the body and the nature of the course of the disease. The work carried out used non-invasive research methods, which, while inferior in accuracy to invasive ones, have a number of advantages, namely: accessibility, safety, possibility of repeated use, relative simplicity and non-invasiveness. All this increases the value of these techniques. It is possible to use HRV indicators to assess the effectiveness of treatment.
conclusions
- In patients with GERD, atypical (cardiac) symptoms are observed in 29.4% of cases.
- Standard ECG recordings in patients with GERD, including those in combination with ulcerative ulcers, more often (compared to patients with ulcerative ulcers) reveal NVIDs.
- When recording ECG daily in patients with a combination of GERD and peptic ulcer, supraventricular extrasystole is recorded significantly more often than in patients with peptic ulcer.
- With parallel 24-hour monitoring of intraesophageal pH and ECG, the symptom index is 60–80%, which confirms the connection between heart rhythm disturbances and GERD.
- The initial indicator of the time to restore sinus node function during EPI is significantly higher in patients with ulcer than in patients with pathology of the esophagus and cardia.
- In patients with pathology of the upper gastrointestinal tract, a study of autonomic tone and HRV reveals an imbalance of the ANS with a predominance of parasympathetic influences.
- Against the background of normalization of 24-hour monitoring of intraesophageal pH, ECG and CM, there is an improvement in conductivity parameters, a decrease in the frequency of heart rhythm disturbances and harmonization of autonomic influences.
- In patients with GERD, the maximum duration of reflux is associated with an ultra-low frequency spectrum of heart rate variability.
- The duration of esophageal acidification is associated with RMSSD heart rate variability.
- Treatment with prokinetics for 6–8 weeks led to QT prolongation in the group of patients with GERD in combination with ulcer, but within the normative values.
A. Yu. Kuzmina Research Institute of Therapy, Novosibirsk
Causes of increased heart rate with VSD
Patients with vegetative-vascular dystonia periodically suffer from pulse and blood pressure disturbances. These attacks can be spontaneous, but in most cases they can be predicted in advance. So, tachycardia can be provoked by the following changes:
- sudden changes in weather conditions, including in the off-season;
- eating large amounts of food;
- intense physical activity, as well as sudden movements and changes in body position;
- violation of the diet (instant coffee, alcoholic and carbonated drinks are especially dangerous);
- any stressful situations.
A healthy lifestyle and a stable psychological state are the main conditions for preventing another attack. However, increased concern for one’s own health can cause the development of cardioneurosis. In this condition, the patient constantly listens to the rhythm of the heart, counts the pulse and measures the pressure, which can activate the next exacerbation.
Signs of an attack
Normally, a person does not feel the work of the heart. When the first symptoms of tachycardia appear, the patient’s pulse quickens, as if after running or with strong excitement. There is also a feeling of fear and anxiety, which is largely provoked by the presence of additional symptoms. Despite the fact that tachycardia with VSD is not a life-threatening condition, it often becomes a reason to call doctors. The patient is concerned about the following signs:
- severe weakness;
- frequent and strong heartbeat;
- pain in the chest area, which raises suspicion of myocardial infarction;
- heavy breathing, shortness of breath;
- headache and dizziness;
- panic attacks, which further aggravate the clinical picture.
The most common type of syndrome is sinus tachycardia. It is characterized by an increase in the excitability of the sinus node, as a result of which the heart rate increases to 120-130 beats per minute. This clinical picture can develop at any age and is not a cause for concern if it is not accompanied by additional signs.
REFERENCE! Sinus tachycardia, which most often occurs with VSD, does not cause heart rhythm disturbances. Any manifestations of arrhythmia indicate the need for additional diagnostics of the condition of the heart and blood vessels.
3. Symptoms of paroxysmal tachycardia
A heart attack usually begins with a delay in the pulse and then a strong shock, which the patient himself clearly feels. After this, rapid heartbeat develops. Duration of attack
- from a few seconds to a day or more. Sometimes the attack is limited to the initial shock. The patient reflexively presses his hand to his chest, slouches, and thereby blocks the development of this condition.
An attack in dynamics gives a high heart rate and may be accompanied by dizziness, noise in the head, sensations of general freezing, weakness and tightness in the sternum, and a decrease in the temperature of the extremities. An attack is often accompanied by an increase in blood pressure. A characteristic symptom is also polyuria (excretion of a large amount of urine) at the end or within several hours after the heart rate normalizes.
About our clinic Chistye Prudy metro station Medintercom page!
Necessary examinations
If an attack of tachycardia occurs for the first time, a complete diagnosis of the cardiovascular system is indicated. An increased heart rate also causes additional symptoms that need to be taken into account. The patient’s condition can be assessed using a series of studies:
- electrocardiography is one of the main methods for diagnosing myocardial function;
- echocardiography - examination of the condition of the heart using ultrasound;
- if necessary, tonometry using MRI.
VSD is identified as an independent disease. It was placed in a separate category in the ICD-10 classification. Heart rate disturbances caused by a deficiency of the autonomic nervous system do not pose a threat to the patient's life. A set of examinations that are offered after the first attack, as well as to monitor the condition of the heart and blood vessels, do not show any serious abnormalities.