Angina pectoris: general information
If, as you age, you begin to notice that heart pain occurs after physical activity, immediately consult a cardiologist. There is a high probability that you are developing a heart disease called angina pectoris FC 2. Attacks of pain pass, so many people tend to ignore them. However, the result and direct consequence is myocardial infarction. An even worse option: sudden cardiac arrest. Do not expose yourself to mortal risk - get examined using professional diagnostic equipment at the first symptoms of angina pectoris! Now you have a unique opportunity to undergo a free consultation with a specialist and a set of preparatory examinations when enrolling in a course of enhanced external counterpulsation or shock wave therapy of the heart:
Promotion
Just until the end of autumn, undergo a free consultation and a set of preparatory examinations* when registering for a course of enhanced external counterpulsation or shock wave therapy of the heart.**
Send a request
* Check the details of the Promotion by phone. **Has contraindications; consultation with a doctor is required.
Enhanced external counterpulsation (EECP) Cardiac shock wave therapy (SWTS)
Hurry up to apply, the promotion period is limited.
Doctor's advice
If, against the background of complete health, you begin to experience attacks of pressing, squeezing discomfort behind the sternum, shortness of breath when walking, decreased tolerance to physical activity (you go up to the fifth floor with stops), a burning sensation in the stomach that does not depend on food intake, I I strongly advise you to urgently consult a doctor or call an ambulance! New-onset angina can lead to a heart attack, so the danger of these symptoms should not be underestimated.
What is the algorithm for providing assistance before the medical team arrives?
Lay the patient down, provide rest, access to air, let him chew an acetylsalicylic acid tablet, if you have one, dissolve Nitroglycerin by placing it under the tongue.
What should an ambulance do upon arrival to a call (pre-hospital stage)?
- Anesthetize the patient with narcotic analgesics.
- Administer an anticoagulant (Heparin).
- Give a loading dose of a second antiplatelet agent (Clopidogrel, Ticagrelor, Prasugrel).
- Start an infusion of Nitroglycerin taking into account the blood pressure level.
- Administer beta blockers intravenously.
- If necessary (low gas concentration in the blood), start oxygen inhalation.
What is cardiac angina?
The disease is the most common form of coronary heart disease. Its danger should not be underestimated, because against its background heart failure develops quite quickly. Not far from a heart attack!
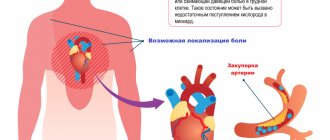
The disease develops in men after 55 years, in women - after 64. The reason is a partial (50-70%) narrowing of the coronary arteries that supply blood to the heart tissue. The narrowing occurs due to the deposition of atherosclerotic plaques on the walls of blood vessels and the formation of blood clots. They impede blood circulation, the heart lacks oxygen and nutrients. Especially during times of physical and emotional stress, when the heart muscle works actively and requires more oxygen. The arteries are not able to satisfy her need. That's when you experience attacks of pain.
Diagnostic procedures
The absence of specific symptoms does not allow the cardiologist to confirm the diagnosis during a physical examination. The doctor carries out differential diagnosis to exclude heart attack and non-ischemic heart pathologies from the patient’s history. Clinical guidelines suggest the following tests to confirm unstable angina:
- electrocardiography;
- general and biochemical blood tests;
- echocardiography;
- coronary angiography.
Cardiologists detect changes in the condition of the coronary arteries and decreased left ventricular function. Based on these data, the diagnosis is confirmed.
How does the disease develop?
It is at such moments that common signs of angina pectoris appear in women and men: you feel a lack of air, arrhythmia. At this time, chemical changes occur in the myocardium associated with metabolic disorders, a decrease in the synthesis of substances, and the accumulation of acids. The functions of the myocardium are gradually disrupted, and its metabolism changes.
What causes this disease? There are certain factors:
- high cholesterol levels;
- obesity when consuming excessive amounts of fats and carbohydrates;
- physical inactivity disrupts lipid volume;
- smoking causes oxygen starvation of cells and arterial spasm;
- arterial hypertension causes myocardial tension;
- anemia, intoxication contribute to oxygen starvation;
- diabetes mellitus increases the risk of ischemia;
- increased blood viscosity is a direct risk of blood clots;
- psycho-emotional stress (especially in women) worsens myocardial nutrition.
Symptoms
Main symptoms include:
- acute chest pain radiating from the left (or right) side to the lower jaw, arm, shoulder blade
- shortness of breath
- feeling of suffocation and lack of air
- feeling of fear, anxiety
- increased pain in the left chest area when trying to take a deep breath
- increased sweating
- tachycardia
- deviation of blood pressure from normal (low or high).
The main factors in the development of the disease that cause symptoms of angina pectoris include
- age (usually after 40 years)
- gender (men develop CHD on average 10 years earlier than women)
- hereditary factor.
An important role in the formation of the disease is played by excess body weight, a history of diseases such as diabetes, arterial hypertension, increased blood clotting, metabolic syndrome, emotional lability, lack of physical activity, smoking and alcoholism.
Stable angina (tension): signs and symptoms
If periodic attacks that occur as a result of exercise last more than 1 month, doctors diagnose “stable angina.” The pain is relieved after taking nitroglycerin.
Depending on how strong the load can cause an attack in the patient, functional classes of the disease are distinguished.
- Angina pectoris FC 1 is characterized by good tolerability, and signs of angina in men and women are noticeable only with excessive stress.
- Angina pectoris FC 2 is manifested by some limitation in normal activities: an attack begins when walking more than 500 m, climbing to the 1st floor, or emotional excitement. With coronary artery disease and angina pectoris FC 2, the first hours after waking up are difficult to bear. Cold weather also has a negative effect.
- Angina pectoris FC 3 is already a serious limitation of normal physical and emotional activity. Obvious signs appear during normal walking at a distance of 150-200 m on level ground, or climbing one floor. Also, angina pectoris FC 3 develops due to anxiety.
- Stable angina pectoris FC 4 occurs after minimal exertion. The patient is unable to perform simple physical activities. This class closely borders on resting angina, i.e. one that is not associated with loads.
This classification allows the doctor to act more accurately when prescribing medications and treatments.
Diagnostics
In order to make a differential diagnosis, i.e. To distinguish ischemic pain from non-ischemic pain based on symptoms, I use specially developed criteria, including 3 main signs:
- classic attacks of angina pectoris,
- their appearance during physical work,
- weakening and disappearance after taking Nitroglycerin tablet/spray or stopping the load.
The presence of all three criteria is typical for typical angina, and two for atypical angina. If the patient has only one criterion, then the diagnosis is doubtful.
I also conduct a general examination of the patient, during which symptoms of heart failure can be identified:
- swelling of the legs,
- thickening of the fingertips,
- bluish lip color,
- swollen veins in the neck,
- enlarged and painful liver.
I especially often notice such signs in the elderly. In patients with heart defects, various sounds can be heard on auscultation. It is mandatory to measure blood pressure, since the vast majority of people with angina have hypertension.
To confirm or refute the diagnosis, I prescribe an additional examination, which includes:
- Blood analysis. Almost all people with coronary heart disease have elevated cholesterol levels. Therefore, I always prescribe a lipid profile (cholesterol fraction) determination. Also, following the protocol, you need to check the glucose concentration and do a general blood and urine test.
- Electrocardiography (ECG) is the main diagnostic method for suspected angina. The main symptom of the disease is a decrease (depression) in the ST segment. Sometimes a negative T wave is recorded. However, often these changes cannot be detected at rest, i.e. when there is no pain. Therefore, I prescribe additional ECG studies for my patients.
- Electrocardiography with stress. Of all such tests, I prefer bicycle ergometry (riding an exercise bike) and treadmill test (walking or running on a treadmill). If, after a certain time, symptoms of angina appear and the ECG shows typical signs (ST segment depression greater than 1 mm and a negative T wave), the test is considered positive. It is worth noting that such studies are not suitable for everyone. For example, I do not perform them on patients over 85 years of age and people with severe heart failure (III-IV functional class).
- Daily ECG monitoring. In cases where physical tests are not possible or the results obtained are questionable, it is advisable to conduct a Holter study. It is also a very good way to detect silent myocardial ischemia. Most often, I prescribe Holter ECG to patients with diabetes.
- Echocardiography (Echo-CG, ultrasound of the heart). The method allows you to check the ability of an organ to pump blood, assess the condition of the valves, the degree of wall thickening, and the presence of intracardiac blood clots.
- Transesophageal electrical stimulation of the heart (TEC) - the procedure is as follows. A flexible probe with an electrode is inserted through the patient's nose and installed in the esophagus in the projection closest to the heart. Then weak signals are sent, causing an attack of angina. At the same time, an ECG film is removed to record specific changes. I also perform this method on patients for whom physical tests are contraindicated.
- Myocardial scintigraphy - with this method I study the intensity of blood supply to the myocardium. For this, a radioactive drug is used (I mainly use thallium-201 and technetium-99-m), which is administered intravenously to the patient. Then he begins to perform moderate physical activity, after which an image is displayed on a special device. The degree of intensity of the glow is used to judge the blood circulation of different parts of the heart. I resort to myocardial scintigraphy if the patient has serious arrhythmias (bundle branch blocks, repeated ventricular extrasystoles), in which it is impossible to see specific changes on the cardiogram. This method is of little information for women, since breast tissue accumulates a significant part of the pharmaceutical drug.
- Coronary angiography is the gold standard for diagnosing coronary heart disease, allowing a reliable diagnosis. It can also be used to determine whether surgery is necessary.
Angina at rest: signs and symptoms
It is characterized by the manifestation of characteristic symptoms in a calm state - at night and especially in the morning after waking up. Typically, angina at rest is diagnosed using 24-hour monitoring. Most often, attacks are caused by increased blood pressure and psycho-emotional stress. Unfortunately, any troubles at work or family quarrel can provoke an attack. And sometimes it is enough to change the position of the body.
This type includes vasospastic angina, the cause of which is a sudden spasm of the coronary vessels. And also post-infarction - manifesting itself 10-14 days after the heart attack.
What is the difference between unstable and stable?
Stable and unstable forms of angina can alternate in the same patient. Differential diagnosis (difference) between them lies in the nature and duration of pain, the provoking factor and the reaction to Nitroglycerin.
In patients with stable angina pectoris, anginal (“angina” is the Latin name of the disease) attacks occur when performing the same physical work and are relieved after taking Nitroglycerin or stopping the exercise. Patients get used to this: they know what actions can cause an attack, and take the medicine in advance.
With unstable angina, episodes of pain:
- occur more frequently;
- last longer;
- provoked by minimal load or develop during rest;
- do not always stop after taking Nitroglycerin.
These symptoms should cause alarm in the patient, as they indicate plaque instability and the threat of a heart attack.
Unstable angina: signs and symptoms
Unlike stable angina, this type of disease changes its behavior, so it is important to constantly be under medical supervision in the first two months after the first attack. Obvious symptoms of unstable angina: changing frequency, duration, intensity of attacks. They can also start at night.
In turn, unstable angina is divided into:
- into classes depending on the nature and severity (initial, subacute and acute stages);
- into groups according to the conditions of occurrence (primary, secondary, post-infarction);
- into groups during therapy (the disease develops during procedures, medication, intensive treatment).
Therapeutic measures
Conservative treatment involves prescribing several groups of drugs to the patient. Antianginal drugs relieve symptoms of angina pectoris. In acute attacks accompanied by intense pain, intravenous infusion of painkillers is performed.
Thrombolytics reduce the likelihood of blood clots. A similar goal is pursued when prescribing direct anticoagulants to a patient.
Lipid-lowering drugs remain an integral component in the drug treatment of unstable angina. They help normalize cholesterol levels in the patient’s blood. Constant use of such drugs reduces the likelihood of complications and recurrent attacks.
If conservative treatment is ineffective, the patient is prescribed surgery. The type of surgical intervention is determined by a cardiologist based on coronary angiography data. Imaging will allow us to understand the extent of damage to the coronary arteries. The most common methods of surgical treatment of angina remain coronary bypass surgery and coronary angioplasty.
Symptoms of angina in women and men
Pain
Most patients report the following symptoms of an angina attack. First of all, cutting, pressing pain in the chest. Many people complain that their heart “burns” or their throat “tightens.” At the same time, you instinctively want to press your hand or fist to your chest. Often the pain migrates to the left shoulder, neck, arm, and shoulder blade. It may grow or disappear suddenly. Symptoms clearly and distinctly appear during exercise, when the patient is diagnosed with IHD angina pectoris FC 2.
Pain can occur after physical exertion, stress, high blood pressure, or overeating. At night - due to stuffiness or low air temperature. Often the attack is accompanied by arrhythmia.
External symptoms and signs of angina pectoris
It is quite simple to identify an attack by its external manifestations. Pay attention to the following signs of angina: the person turns pale, sweat appears on the forehead, his face expresses suffering; fingers lose sensitivity, hands become cold; the patient breathes intermittently and rarely; the onset of an attack is accompanied by a rapid pulse.
Load tests
Electrocardiography with physical activity (Stress ECG, Veloergometry) is a very useful method that helps diagnose angina pectoris. Also, do not forget about stress echocardiography, which allows you to clarify the diagnosis. Since angina pectoris manifests itself during physical activity, the method allows you to accurately determine the load threshold, the recovery period, and study the work of the heart after pain relief. Such diagnostics are carried out on a special bicycle ergometer and treadmill (treadmill). However, it is not suitable for everyone: stress tests are contraindicated in patients with acute angina.
What can the disease be confused with?
As for diseases not related to the cardiovascular system, based on the symptoms and signs, angina pectoris can be mistaken for:
- osteochondrosis of the cervical or thoracic spine;
- vegetative-vascular dystonia;
- gastrointestinal diseases (diaphragmatic hiatal hernia);
- pleurisy, pulmonary embolism;
- pinched nerves.
Usually this disease is confused with the onset of myocardial infarction. The signs are really very similar. The main difference is that an attack of angina is relieved by taking nitroglycerin. In case of a heart attack, the medicine does not work or relieves pain only slightly and temporarily.
Holter monitoring
Daily, or Holter, monitoring is a continuous process of monitoring the patient’s heart throughout the day using a special recorder, the data from which is sent to the stationary equipment of the attending physician. This type of ECG allows you to diagnose unstable angina and angina in the absence of symptoms, helps evaluate previously prescribed treatment, records changes in the cardiogram during exercise, stress, sleep, etc. It can be either outpatient or inpatient, it depends on the purpose of the study and the patient’s well-being.
Where can I get diagnosed and treated?
Rest assured that your heart is not in danger! If the first symptoms and signs of angina appear, consult a qualified healthcare provider. Cardiologists at the CBCP Center for Circulatory Pathology are ready to help you. The clinic will offer professional consultation and modern types of diagnostics, through which the doctor will receive objective, detailed and accurate information about the disease.
If you discover serious violations, do not despair! The level of medicine at CBCP makes it possible to effectively treat complex cardiovascular diseases using medicinal and non-surgical methods.
Interview and examination of the patient
An important role in the differential diagnosis of angina pectoris is played by questioning and examination of the patient. When compiling a medical history, the cardiologist studies all the symptoms that concern the patient, risk factors, for example, the presence of bad habits, obesity, etc., as well as possible genetic predisposition. During the examination, the doctor listens to heart sounds, looks for signs of damage to the main arteries, as well as signs of lipid metabolism disorders - one of the main causes of the formation of cholesterol plaques. Externally, they manifest themselves in the appearance of xanthoma and xanthelasma - skin neoplasms of a characteristic yellow color.
Treatment
The goals of treatment are to improve the prognosis (prevent heart attack) and eliminate symptoms of the disease. Non-medicinal (sports, diet), medicinal (tablets and drip infusions) and surgical treatment methods are used.
At the EXPERT Clinic, patients have the opportunity to receive a full consultation with a cardiologist on lifestyle changes and modification of risk factors. If necessary, treatment in a day hospital under the supervision of experienced medical personnel is possible.
FAQ
How to avoid angina pectoris?
To avoid angina pectoris, it is necessary to prevent the development of atherosclerosis if possible, because in the vast majority of cases it is the cause of angina. As is known, many factors directly influence the formation of atherosclerotic plaques. Gender, age, heredity are predisposing factors that cannot be changed, but other factors can be controlled and even prevented:
- high blood pressure
- smoking
- high cholesterol
- overweight
- diabetes
- low physical activity
- stress
Changing these factors is in your hands!
Is it possible to completely recover from angina?
Angina pectoris, as a rule, occurs as a result of damage to the coronary arteries supplying blood to the myocardium by atherosclerosis, and this is a chronic incurable process. However, with a properly selected treatment regimen, it is possible to ensure that long-term remission occurs and angina attacks will not bother you. Also, at present, if necessary, it is possible to install a stent into the narrowed lumen of the vessel to restore blood circulation, or MCS/CABG surgery is a surgical intervention that restores the blood flow of the heart below the site of the narrowing of the vessel. In this surgical procedure, another path for blood flow is created around the narrowing site to the part of the heart that is not supplied with blood.
Where does it hurt during an angina attack?
Characteristic of angina is paroxysmal pain behind the sternum, in the center of the chest. The pain is of a compressive, pressing nature, more often associated with physical or psycho-emotional stress and goes away when it stops. The pain may radiate to the left arm, shoulder blade, lower jaw and collarbone. If nitrates are used, the effect on angina is not delayed, it develops immediately, within 1-2 minutes.
Are there ways to cope with an angina attack without medications?
Since many people experience angina attacks during physical activity, sometimes simply stopping the activity (walking, etc.) and resting can lead to the cessation of pain. However, people suffering from angina pectoris should always have nitroglycerin or nitrospray with them in order to relieve an attack of pain within one to two minutes. You should not delay the time before taking nitroglycerin, since pain is a manifestation of myocardial ischemia (insufficient blood supply), and if it persists, then foci of necrosis may occur in the myocardium (myocardial cells may die). If angina attacks become more frequent, you should urgently consult a cardiologist.
What medications will help with an attack of angina?
An attack of angina must be stopped as soon as possible from the moment of its occurrence, because prolonged ischemia will lead to the development of necrosis, i.e. myocardial infarction. If an attack occurs for the first time in your life, call an ambulance. You can take a nitroglycerin tablet on your own or use a nitro spray under the tongue. The effect will occur within 1-2 minutes and does not last long, 10-15 minutes. It is better to take the drug while sitting or lying down, as a short-term decrease in blood pressure, dizziness, headache, tinnitus may occur - these symptoms are safe and are a consequence of the action of nitroglycerin. If pain returns, you can take nitroglycerin again, because it does not accumulate in the body; multiple doses of the drug are possible during the day (up to 6 tablets per day). If your blood pressure is high, you need to lower it to normal levels.
All patients who have suffered an attack of angina pectoris need to have an ECG performed and a decision by a cardiologist on hospitalization.
Why is it necessary to quit smoking? How does smoking worsen angina?
If you smoke and have angina, the best thing you can do to help your heart is to quit smoking!
Studies have shown that the mortality rate in those patients with angina who quit smoking decreased by 2 times compared to those who continued to smoke. Why? Angina is based on a lack of oxygen in the heart muscle, and smoking increases the level of carbon dioxide in the blood, and it displaces oxygen in the blood. This leads to oxygen starvation of the heart muscle. Smoking also increases blood viscosity. Smoking increases the frequency and aggravation of angina attacks and greatly increases the risk of myocardial infarction. Quitting smoking eliminates the adverse effects of nicotine on the coronary arteries, and angina attacks disappear or become less frequent.
Important: replacing cigarettes with cigars and pipe tobacco, switching to cigarettes with less tar and nicotine do not reduce cardiovascular risk!
Contrary to popular belief, abruptly quitting smoking is not harmful; overcoming this bad habit has an undeniable positive effect, regardless of smoking experience.
You need to be prepared for the fact that sometimes depression and irritability occur when quitting smoking, in which case you can seek help from a psychotherapist.
I suffer from angina pectoris, but I dream of losing excess weight. What physical activities are acceptable for people with such problems?
For people suffering from angina, 30–45 minutes of physical activity per day is recommended. The best choice is walking (preferably at a brisk pace) or Nordic walking with ski poles, cycling, swimming. It is important that the exercises do not cause pain, palpitations, or shortness of breath. When practicing swimming or water aerobics, you should remember that cold water can provoke angina attacks, so the water temperature in the pool should be comfortable for you. It is better to do water aerobics under the supervision of a trainer and according to a program specially adapted for people with cardiac problems. In this case, the loads should increase very gradually. However, to lose weight, you need not only physical activity, but also proper nutrition; a nutritionist will help you choose the right menu during your consultation.
Can you have angina if there is no pain?
Unfortunately yes. For example, with diabetes mellitus, diabetic polyneuropathy develops, and the patient may not feel pain, this is the so-called silent ischemia. This condition is dangerous because the patient does not take action in time, and myocardial infarction will develop. In some cases, shortness of breath during exercise can be considered equivalent to pain, so you can suspect the presence of angina pectoris and come for examination to a cardiologist.
Treatment history
Case No. 1
Kirill, 57 years old. Experienced smoker, hypertensive (“working” pressure 150/95 mmHg). Five years ago, according to the patient, he had problems with his heart and blood pressure, was examined, took prescribed medications for six months, then stopped taking them on his own. During the visit to the clinic, attacks of chest pain appeared during physical activity, which went away when the exercise stopped. At the doctor’s appointment, blood pressure is 170/100 mmHg, rapid pulse is 90 beats per minute. The patient was examined - an increase in the level of “bad” cholesterol was detected, ECG and ultrasound of the heart without signs of ischemia, and ischemia was recorded on the 24-hour ECG monitor at the time of significant physical activity, i.e. there is angina pectoris. The patient was given a treatment regimen for angina pectoris, which resulted in normalization of blood pressure and cholesterol levels within 3 months, and a significant increase in exercise tolerance. With the help of a psychotherapist, the patient decided to quit smoking and took up Nordic walking with a gradual increase in loads under the supervision of a cardiologist. Over the past year, angina attacks have not bothered me. It is recommended to continue taking medications and undergo regular preventive examinations.
Thanks to cooperation with doctors and the desire to feel better, the patient was able to change his lifestyle, prevent complications of the disease and prolong his life for many years.