Medical editor: Strokina O.A. - therapist, functional diagnostics doctor. September, 2021.
ICD-10 code: I35.0, I06.8, I35.8.
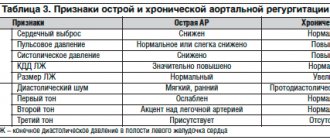
Aortic insufficiency is a malfunction of the aortic valve with the formation of reverse blood flow from the aorta into the cavity of the left ventricle. Symptoms directly depend on the amount of blood entering the ventricle. Diagnosis of pathology is possible only with the help of echocardiographic examination (ultrasound of the heart). Treatment also depends on the degree of deficiency and may involve both conservative and surgical techniques.
Aortic insufficiency is a heart defect that is characterized by the development of regurgitation (backflow of blood) on the aortic valve during the relaxation phase of the heart muscle. As a result, blood from the aorta flows back into the ventricle. There is an overflow of its volume, which in the future may threaten the expansion of the cavity of the left chambers of the heart with the development of heart failure.
During the contraction phase, the left ventricle ejects blood into the aorta, after which the ventricular relaxation phase begins. At this moment, the blood tends to return back. Her path is blocked by 3 leaflets of the aortic valve, which are “sacs”. As they fill with blood, the valves straighten, close with each other and completely close the aortic opening.
On the mitral and tricuspid valves, a small discharge of blood in the opposite direction is normally allowed, and the term “insufficiency” is not used here. In the case of the aortic valve, even minimal regurgitation is a pathology that needs to be monitored.
General information
Aortic valve insufficiency is one of the types of heart defects acquired during life, namely the aortic valve, accompanied by hemodynamic disturbances. The pathology causes a reverse flow of blood from the aortic cavity into the left ventricular chamber during relaxation of the heart muscle (in diastole). Most often, failure is provoked by acute rheumatic fever or infective endocarditis .
In some cases, the pathology may be due to congenital anomalies, which are most often combined with damage to other valves and Marfan syndrome .
How do adaptive mechanisms work?
As a result of incomplete closure of the semilunar valves, the returned blood forces the left ventricle to work harder and push out more blood. It expands and lengthens. After some time, muscle hypertrophy occurs. It is quite enough to compensate for the defect for many years.
In patients with rheumatism, repeated attacks lead to decompensation due to myocardial overload. Heart failure develops.
It is worth noting the peculiarity of the development of the decompensatory mechanism in syphilis: after inflammation, cicatricial deformation occurs at the base of the aorta. This is where the coronary vessels arise. Therefore, their mouth narrows and becomes deformed. Disturbance of the blood supply to the myocardium predominates.
Pathogenesis
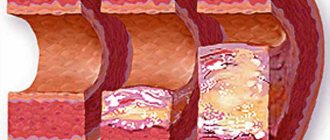
The mechanism of development of this type of heart defect is based on an inflammatory-sclerotic process that affects the leaflets of the aortic valve and causes them to shrink and incompletely close. As it spreads, the aorta may also undergo pathological changes, which leads to stretching of the mouth and retraction of the valves, and the boundaries of the left ventricle also significantly expand. In addition, the addition of septic lesions and the formation of defects is possible.
Pathogenesis in aortic insufficiency
With aortic insufficiency, hemodynamic disturbance occurs: diastole occurs when the semilunar valves are not closed, which entails a reverse flow of blood from the aortic space into the left ventricle throughout the entire period of relaxation of the heart muscle. This causes its stretching (compensatory tonogenic dilatation) and hypertrophy , and diastolic pressure decreases. If blood stagnation occurs in the pulmonary circulation, then the pressure in the pulmonary arteries increases and, as a result, the development of right ventricular hypertrophy and pulmonary hypertension . Hyperfunction and hypertrophy of the right ventricle leads to the gradual development of right ventricular failure, but death may occur earlier with significant hemodynamic disturbances and left ventricular failure.
The amount of blood thrown back depends, to a large extent, on the size of the resulting pharynx in the aortic valve. Systole is accompanied by a large ejection of blood into the aorta, which leads to expansion of its initial sections.
Aortic valve disease contributes to ischemia of the muscle tissue of the left ventricle, as it experiences a greater load and an increased need for oxygen in conditions of less than the required amount of circulating blood in the coronary vessels and coronary insufficiency.
Fluctuations in blood pressure are caused by an increase in systolic blood pressure due to a significant increase in stroke volume in the left ventricle, while diastolic blood pressure is reduced due to rapid regurgitation of the blood, and as a result, numerous characteristic “peripheral” symptoms occur.
tachycardia begins to occur , causing shortening of diastole and some limitation of the reverse flow of blood from the aorta.
Survey data
On an x-ray (including fluorography), the expansion of the aortic arch and enlarged left and right ventricles are clearly visible.
ECG - shows a shift to the left of the electrical axis, signs of myocardial hypertrophy, extrasystoles are possible.
Phonocardiographic signs allow you to objectively examine heart murmurs.
Ultrasound or echocardiography - indicates an enlargement of the left ventricle, most accurately characterizes the pathology of the valves (changes in structure, flutter of the valves, width of the residual opening).
Dopplerography is the most informative
The Doppler ultrasound method allows:
- see the return flow of blood;
- diagnose the degree of valve prolapse (internal deflection);
- establish the compensatory capabilities of the heart;
- determine indications for surgical treatment;
- assess the severity of stenosis by violation of the normal pressure gradient (from 3 to 8 mm Hg).
In the functional diagnosis of aortic stenosis using Dopplerography, it is customary to take into account the following gradient deviations (differences between pressure in the aorta and left ventricle):
- mild stenosis - less than 20 mm Hg. Art.;
- moderate - from 20 to 40;
- severe - over 40, usually 50 mmHg. Art.
The development of heart failure is accompanied by a decrease in the gradient to 20.
A type of echocardiography, the transesophageal version, is carried out by inserting a special sensor with an esophageal probe closer to the heart. It makes it possible to measure the area of the aortic annulus.
By catheterizing the chambers of the heart and blood vessels, the pressure in the cavities is measured (along the gradient) and the characteristics of the blood flow are studied. This method is used in specialized centers for diagnosis in people over 50 years of age, if it is impossible to decide otherwise on the method of surgical intervention.
Congenital defects are suggested to be operated on after 30 years of age, earlier - only with rapid decompensation
Classification
Isolated damage to the aortic valve is quite rare - in approximately 5-9% of all diagnosed heart defects. In most cases, the pathology develops against the background of the development of stenosis of the aortic mouth and damage to other heart valves.
Aortic insufficiency can be absolute and relative, characterized by severe atherosclerosis of the aorta and the presence of dilatation of the aortic mouth in the case of hypertension .
Depending on the length of the stream during regurgitation of blood flow and the amount of regurgitated blood, various degrees of the defect are distinguished.
Aortic valve insufficiency 1st degree
For the 1st degree of aortic insufficiency, the reverse blood flow reaches 5 mm - a jet under the aortic valve leaflets, while the amount of blood thrown back is approximately 15%.
Aortic insufficiency grade 2
In patients with grade 2 aortic insufficiency, regurgitated blood is diagnosed to reach the mitral valve at approximately a distance of 5-10 mm, and the amount of ejected blood increases to 30%.
Aortic valve insufficiency grades 3 and 4
The most severe forms of development of the pathology, because more than half of the volume of pumped blood returns to the ventricle in a flow that reaches directly to the apex of the heart chamber, while the distance can exceed 10 mm.
The role of valves in the formation of aortic stenosis
With repeated rheumatic attacks, the aortic valves shrink, and the free edges become so welded together that they narrow the outlet. The fibrous ring becomes sclerotic, further increasing the stenosis.
Symptoms depend on the degree of narrowing of the opening. A critical stenosis is considered to be a diameter of 10 mm2 or less. Depending on the area of the free aortic opening, it is customary to distinguish between the following forms:
- light - more than 1.5 cm2;
- moderate - from 1 to 1.5 cm2;
- severe - less than 1 cm2.
Patients complain about:
- pain similar to angina attacks is caused by insufficient blood flow into the coronary arteries;
- dizziness and fainting due to brain hypoxia.
Signs of heart failure appear in the event of decompensation.
During the examination, the doctor notes:
- pale skin;
- palpation is determined by a shift to the left and down the apex impulse, “trembling” at the base of the heart on exhalation, like a “cat’s purr”;
- hypotension;
- tendency to bradycardia;
- typical sounds on auscultation.
Causes
Relative (functional) aortic insufficiency occurs with hypertensive disease with pronounced dilatation of the aortic mouth or with the development of aortic trismus of various origins. However, most often the pathological changes are organic and are caused by deformations and defects of the aortic valve leaflets: wrinkling, perforation, etc.
The most common causes of aortic insufficiency are:
- systemic connective tissue diseases;
- rheumatic fever;
- endocarditis of infectious origin, causing perforation of infected leaflets;
- atherosclerosis against the background of dissecting aortic aneurysm also leads to damage to the valve leaflets;
- arterial hypertension;
- aortitis;
- valve damage resulting from tertiary syphilis ;
- Marfan syndrome , which initiates myxomatous degenerative damage to both the aortic valve leaflets and the aorta;
- chest injuries, especially when valve flaps are torn off.
Important! Rheumatic endocarditis causes heart disease in 70% of cases and is combined with stenosis and disturbances in the structure of the mitral valve, the development of its insufficiency and mitralization of aortic valve disease. Pathogenesis causes thickening, deformation and shrinkage of the semilunar valve structures, initiating disturbances in closure and hemodynamics in diastole.
Diagnosis confirmation methods
Diagnosis is usually not difficult. The age of the patient helps in determining the cause.
- Typically, children and young people are characterized by rheumatic lesions or the consequences of infective endocarditis.
- In middle age, manifestations of syphilis are more typical.
- In older people, atherosclerosis is the main disease.
ECG signs reveal significant hypertrophy of the left ventricle, in later stages - both ventricles and the left atrium.
Phonocardiography allows you to synchronously record noise; the diagram shows the point of maximum noise of the aorta
The x-ray shows expanded contours of the cardiac shadow, displacement of the apex outward and downward, and expansion of the ascending portion of the aortic arch.
Echocardiography and ultrasound make it possible to record the increase in the volume of the left ventricle, mitral valve flutter, and the magnitude of regurgitation.
The introduction of a catheter into the cavity of the heart allows you to accurately measure the amount of cardiac output and the volume of returned blood.
Laboratory tests play a role in determining the cause of aortic regurgitation.
Symptoms
With relatively powerful compensatory abilities of the body, formed aortic insufficiency for many years (10-15) may not cause subjective clinical manifestations. The exception is acute heart disease caused by destruction of the valve leaflets by infective endocarditis, which can develop in just a few hours, and sometimes even minutes.
First, patients begin to feel palpitations (caused by compensatory sinus tachycardia ) and strong pulsation in the neck, head and heart due to high cardiac output and high pulse pressure in the arterial system. At the same time, there is an increased tendency to faint, which occurs due to cerebral circulatory insufficiency during a diastolic drop in blood pressure in the arteries of the brain. At the stage of decompensation, complaints indicating left ventricular failure begin to appear. Patients may experience shortness of breath , especially at the beginning of physical exercise, and then at rest, as well as attacks of breathlessness and increased fatigue . Signs of further right ventricular failure include pain in the right hypochondrium, indigestion, swelling of the lower extremities and worsening diuresis .
Clinical manifestations of aortic insufficiency usually include the following symptoms:
- dizziness and tendency to sudden fainting;
- pain in the heart area , which are angina-like in nature, having physical exertion or emotional stress as the root cause, they are difficult to relieve with nitroglycerin and usually occur at rest and at night:
- visually visible pulsation of the carotid arteries, subclavian, radial and temporal veins, which is also called the “carotid dance”;
- Musset's symptom , manifested by shaking the head back and forth in time with the pulse;
- quite rare Landolfi symptom , manifested by pulsation of the pupils with systolic constriction and diastolic dilation;
- manifestations of Quincke's symptom - “pseudocapillary pulse” with variable redness and blanching of the nail bed at the base of the root in case of intense pressure on the apex or changes in the color intensity of spots on the forehead during skin friction, which is associated with pulsation of small-caliber arterioles that are not normally capable of pulsation ;
- symptoms similar to cardiac asthma and caused by stagnation of blood in the pulmonary circulation;
- stagnation in the systemic circulation causes swelling of the neck and swelling of the legs;
- high and racing pulse;
- pulsating sensations in the area of the right hypochondrium, located in the projection of the liver;
- pseudocapillary pulse or Quincke's sign .
Clinical manifestations
Symptoms of aortic insufficiency appear with the development of decompensation or when patients are forced to consult a doctor about chest pain and night suffocation. Before this, patients do not feel sick for 10-15 years, do physical work and play sports.
Typical complaints are more typical for atherosclerotic and syphilitic lesions. With infective endocarditis and rheumatism, patients notice dizziness, headache, increased shortness of breath, and palpitations.
- Pain behind the sternum occurs the same in nature as with angina (pressing, burning) with irradiation to the left shoulder, fingers, and scapula. But they are not associated with physical activity and last longer. Cannot be removed with nitroglycerin.
- Feeling of internal shocks of the body, mechanical impulses in the head, legs and arms.
- Shortness of breath indicates the onset of decompensation. At first it only bothers me during physical work, then it develops at rest, night attacks of suffocation begin, and the inability to take a lying position.
- Stagnation in the venous bed leads to swelling in the feet and legs, pain and heaviness in the right hypochondrium.
The echocardiogram picture is deciphered by a specialist
Tests and diagnostics
During physical examination, patients reveal a significant difference between systolic and diastolic pressure readings (with systolic being higher than normal and diastolic being lower). On palpation, the apical impulse is felt more dome-shaped, strong and shifted to the left and somewhat downward in conditions of an enlarged chamber of the left ventricle. Thanks to auscultation, a weakening of the first sound at the apex of the heart and a weakening of the second sound above the aorta can be heard.
In some cases, this heart defect is characterized by the detection of two sounds on the femoral artery - the Traube sound and the double Vinogradov-Durozier murmur .
Instrumental examination methods allow us to identify such signs of aortic insufficiency as:
- left ventricular hypertrophy and , left ventricular overload and relative coronary insufficiency, which are displayed on the ECG as a decrease in the ST segment and identification of a negative T wave in the first and second standard and left precordial leads, as well as possible blockade in the left bundle branch;
- thanks to echocardiography, fluttering is detected in the anterior leaflet of the mitral valve in diastole due to the impacts of the jet of reverse blood flow from the aorta;
- X-ray shows the aortic configuration of the heart - with an enlarged left ventricle or a specific “boot” shape;
- during Doppler studies, reverse blood flow into the heart chamber and diastolic reverse flows in the cavity of the abdominal aorta are detected;
- high-frequency diastolic murmurs, a decrease in amplitude towards the end of diastole and the amplitude of the second sound in patients are displayed on phonocardiography above the aorta.
How does the aortic valve work?
The tricuspid structure of the aortic valve is distinguished from the bicuspid mitral valve by the absence of papillary muscles and tendon chords. Therefore, it opens and closes only under the influence of the difference in pressure in the cavity of the left ventricle and the aorta.
During opening, elastin fibers from the ventricle press the valves against the walls of the aorta, opening the hole for blood flow. At the same time, the aortic root (the initial part) contracts and pulls them towards itself. If the pressure in the ventricular cavity exceeds the pressure in the aorta, then blood flows into the vessel.
The valves close with swirling currents in the area of the sinuses. They move the valve away from the walls of the aorta towards the center. Elastic flaps close tightly. The closing sound is heard with a stethoscope.
Diet for aortic valve insufficiency (aortic insufficiency)
Diet for cleansing blood vessels for diseases of the cardiovascular system
- Efficacy: therapeutic effect after 3 months
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Treatment of aortic insufficiency occurs under conditions of limited physical activity, which should be taken into account in nutrition. In addition, if you have heart problems, you should avoid:
- fried, smoked and fatty;
- too peppery and salty;
- refined sugar - in candies, ice cream, cakes, etc.
You also need to limit salt consumption - no more than 5 g and saturate your diet with healthy vegetables, dried fruits, herbs, berries, seafood and offal.
Treatment
Treatment of aortic regurgitation depends on the identified cause.
For rheumatism, antibiotics and courses of prophylaxis are needed to prevent repeated attacks.
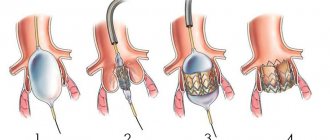
The diagram shows surgical strengthening of the aortic ring and complete closure of the valves
Infectious endocarditis is treated with high doses of anti-inflammatory drugs and corticosteroid hormones.
Coronary pain and hypertension are relieved with adrenergic blocking agents, long-acting nitro drugs, and diuretics.
Treatment of atherosclerosis requires the use of a strict diet and statins.
Acquired heart defects (AHD)
Heart valve defects
Valvular heart disease is characterized by damage or defect of one of the four heart valves: mitral, aortic, tricuspid or pulmonary.
The mitral and tricuspid valves control the flow of blood between the atria and ventricles (the upper and lower chambers of the heart). The pulmonary valve controls the flow of blood from the heart to the lungs, and the aortic valve regulates the blood flow between the heart and the aorta, and therefore the blood vessels to the rest of the body. With normal heart valve function, blood flows with the proper force in the right direction at the right time.
With a heart defect, the function of the valve is impaired; it can become too narrow (stenosis), which is why it does not open completely, or expand and cannot close completely (insufficiency). A narrowed valve prevents blood from flowing out of the chamber of the heart, while when it fails, the blood flows back into the chamber from which it previously came out. Impaired valve function leads to enlargement and thickening of the heart muscle, reducing its elasticity and efficiency.
The most common defects are the mitral and aortic valves.
The severity of heart disease varies. In mild cases there may be no symptoms, but in advanced cases the defect can lead to congestive heart failure and other complications. Treatment depends on the extent of the disease.
Causes of heart valve defects
There are many reasons. Some of them are present at birth (congenital), while others can be acquired later in life:
- aging of valves: heart valve tissue can degrade with age due to atherosclerosis, lose elasticity and become hard;
- rheumatism;
- bacterial endocarditis;
- high blood pressure;
- myocardial infarction;
- heart tumors
- systemic diseases (rheumatoid arthritis, systemic lupus erythematosus, syphilis);
- radiation therapy used to treat cancer.
Symptoms that may appear due to heart valve disease
Symptoms of heart disease can occur suddenly, depending on how quickly the disease progresses. When the disease progresses slowly, your heart may adjust and you may not notice the onset of any symptoms. It is important to understand that the severity of symptoms is not equivalent to severe heart valve disease and, conversely, symptoms may be completely absent in cases of severe heart valve disease.
Symptoms of heart disease include:
- Shortness of breath during exercise, fatigue
- Swelling of the extremities, rapid weight gain due to fluid accumulation
- Palpitations or irregular heartbeat
- Chest pain
- Dizziness or fainting
- Fever (if the valve is infected)
To identify and treat heart valve diseases, correct and timely diagnosis is important.
Diagnosis of defects
Valvular heart disease can be detected by listening to characteristic sounds known as heart murmurs.
To fully diagnose the defect, you need to undergo one or more of the following studies:
- An electrocardiogram (ECG) shows the heart's electrical activity, regularity of heartbeats, thickening (hypertrophy), and damage to the heart muscle from coronary artery disease.
- A chest x-ray shows enlargement of the heart chambers due to dysfunction of the heart valves.
- Echocardiogram (EchoCG) is the gold standard in modern diagnostics. In an echocardiogram, sound waves bouncing off the heart are recorded and converted into images. The scans can reveal abnormal size, shape, and movement of the heart and valve dysfunction.
- Coronary angiography, which involves inserting a catheter into the heart to assess the condition of the vessels supplying the heart.
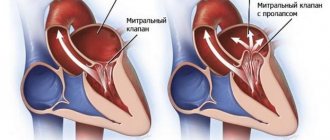
Mitral valve defects
There are three types of mitral valve dysfunction:
- Mitral valve prolapse is when both valve leaflets are enlarged and bulging, preventing them from closing evenly.
- Insufficiency is when the valve leaflets do not close tightly, causing blood to leak back into the left atrium of the heart. Deficiency can occur suddenly (acute) or, more often, gradually over time (chronic). Acute mitral valve regurgitation is often caused by damage to the heart, such as a heart attack or infective endocarditis.
There are many reasons why chronic mitral valve insufficiency can develop. Symptoms include fatigue, shortness of breath on exertion and while lying down, and irregular heartbeat.
- Stenosis—the mitral valve leaflets thicken, become rigid, and may even fuse together. Because of this, the valve opening narrows. Among adult patients, stenosis is more common in women, and the main cause is rheumatism. Symptoms include shortness of breath on exertion, swelling of the lower extremities, and cardiac arrhythmias. In some patients, clots (thrombi) form in the left atrium. These clots can travel through blood vessels and damage the brain, spleen, or kidneys.
Aortic valve defects
Aortic valve regurgitation occurs when the valve leaflets do not close and blood flows back into the left ventricle of the heart. A patient may have significant aortic regurgitation for many years without developing significant symptoms. Signs of the disease include palpitations, shortness of breath on exertion or while lying down (there may be sudden severe shortness of breath in the middle of the night), chest pain.
Aortic valve stenosis affects men more often than women. This is a condition where the valves thicken, become stiff and fuse together, narrowing the valve and preventing the normal flow of blood from the heart to the aorta and the rest of the body. Aortic valve stenosis usually does not cause symptoms until the valve opening has narrowed to about one-third of normal size. Symptoms include shortness of breath on exertion, chest pain, and fainting.
Tricuspid valve insufficiency
This is a heart defect characterized by incomplete closure of the tricuspid valve leaflets and the reverse flow of blood from the right ventricle into the right atrium.
Damage to the tricuspid valve, like other heart valves, can be caused by rheumatism, myxomatosis, infective endocarditis, or chest trauma.
Tricuspid valve insufficiency may also not be associated with damage to the valve itself, but may arise as a result of a long course of mitral and aortic defects, in the absence or improper treatment of them.
Treatment of heart valve defects
Treatment for heart valve disease will depend on the type and severity of the condition and may include medication or surgery.
If the heart defect is significant and medications do not help, surgery is performed to repair or replace the heart valve. Currently, heart valve surgery strives to perform valve-sparing operations. Thanks to improvements in reconstructive surgery techniques, it is possible to restore the valve even with infective endocarditis. In other cases, the valve is replaced with an artificial prosthesis.
Artificial heart valves
Artificial heart valves have improved significantly since their invention, and cardiac surgeons now have prostheses that can perform the function of their own valve as closely as possible.
Depending on the composition, artificial heart valves can be mechanical or biological. Mechanical valves are made entirely of synthetic materials, their advantages are strength, durability and wear resistance. The disadvantage is the need for lifelong use of anticoagulants (blood thinners) to prevent the formation of blood clots.
Artificial heart prostheses
Biological valves are made from animal heart tissue and treated with special solutions that increase wear resistance and prevent immune rejection after implantation. The advantages of biological prostheses are that there is no need for lifelong use of anticoagulants. Disadvantage: rapid wear, limited age of the patient. Biological prostheses are recommended for patients over 70 years of age; their service life is about 10-15 years.
Heart surgery
In most cases, the surgeon makes an incision in the middle of the sternum to reach the heart, uses a heart-lung machine to circulate blood throughout the body during surgery, stops and opens the heart to reach the diseased valve, then repairs or replaces the valve.
Heart valve surgery is also performed through a small incision on the right side of the chest using video support.
Patients with aortic stenosis can undergo aortic valve replacement with a biological prosthesis through the femoral artery or the apex of the heart - without cutting the sternum and stopping the heart. This operation is performed on older patients at high risk of standard open heart surgery. In this case, only biological prostheses are implanted.
After heart surgery
The World Health Organization (WHO) has defined health as not only the absence of disease and illness, but also the presence of physical, mental and social well-being. The goal of heart surgery is not only to prolong life, but also to improve functional mobility and quality of life.
Open heart surgery is a major procedure and requires time to fully recover. It depends on the age and general health of the person, as well as the complexity of the operation.
If you seek surgical help in a timely manner, it is possible to avoid postoperative complications and go through a short recovery path in almost 100% of cases.
During the first two weeks the patient feels tired and weak, the general condition gradually recovers over the next month. During this period, you need to limit heavy physical activity and give up sports. You need to leave the house at least 2 times a day for a short walk and try to increase your load a little every day. The sternum will heal completely within two months, after which it will be possible to return to normal household activities.
For many patients, returning home after heart surgery is a great relief, but for some it can be quite frightening. Follow the recommendations of your doctor, take prescribed medications on time, the duration and quality of your life depends on this.
Surgery
The choice of surgical technique depends on the presence of an aortic aneurysm. In the absence of an aneurysm, the aortic valves are replaced with artificial ones.
If there is an aneurysm, the operation is complicated by replacing the ascending section with a graft and suturing the coronary arteries.
Simultaneous replacement of the initial section of the aorta and valves in case of aneurysm