Resuscitation is the restoration of body functions when they are significantly reduced with a high threat of death, as well as a return to life in case of sudden death. The goal of resuscitation is to prevent sudden death, stabilize vital functions, and, if possible, restore some of what is lost due to illness or injury.
Further treatment and recovery will take place in another, non-intensive care unit. The task of specialists in the intensive care unit (or ICU) is to prevent death from a person.
When is resuscitation required in oncology?
Resuscitation in oncology involves, if not returning a cancer patient to an absolutely normal life, then maintaining vital functions in a stable state.
In what cases is a patient taken to the intensive care unit? There are differences in the work of the oncology intensive care unit from the usual ones. In addition to typical cases of cardiopulmonary resuscitation after cardiac arrest or fatal rhythm disturbances, which also happens during a malignant process, a cancer patient is admitted to the intensive care unit:
- After extensive combined operations for common malignant processes, when the cancerous tumor and adjacent organs and tissues are removed as a single block.
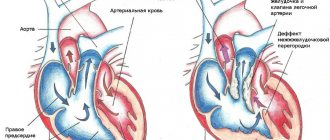
- After thoracic interventions, when a change in the anatomical relationship in the chest cavity after removal of part or all of the lung with lymph nodes or a tumor conglomerate of the mediastinum directly affects the functioning of the heart.
- After removing part or all of the stomach for cancer, because the malignant process causes a catastrophic metabolic disorder that at the end of the last century led to the death of one in four of those operated on, intervention in the abdominal cavity can lead to irritation of the vagus nerve, which partly determines the heart rhythm.
- With all interventions on the brain, due to the danger of swelling and compression of the medulla oblongata, where the regulatory centers of the cardiovascular and respiratory systems are located.
- In case of severe complications of stage 4 chemotherapy, for example, in case of critical thrombopenia with the risk of spontaneous bleeding, necrotic enteritis, and so on.
- For post-chemotherapy complications of grade 3 in patients with severe concomitant diseases, when their decompensation is possible.
- When using certain immunological anticancer drugs that cause severe allergic reactions, and during high-dose chemotherapy.
- To monitor the patient’s condition after some “non-standard” methods of administering chemotherapy.
- In case of decompensation of concomitant diseases, for example, hypoglycemic or hyperglycemic coma due to diabetes mellitus, ventricular fibrillation, and so on.
- In case of breathing problems as a result of extensive metastasis to the lungs, forced mechanical ventilation is required.
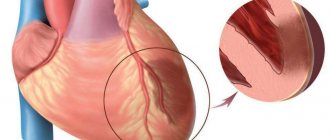
- After bleeding in any organ due to the disintegration of a malignant tumor.
It is impossible to list all the clinical situations when the functioning of organs and systems becomes so insufficient to support life that emergency and active intervention by professionals is required.
Degrees of coma
To simplify differentiation, doctors distinguish the following degrees of coma during strokes:
- 1st degree . It is determined by lethargy or loss of consciousness with preservation of reflexes. This is mild damage to brain cells during a stroke and slight depression of the functions of the nervous system. At the same time, skin reflexes are weakened and muscle tone is increased;
- 2nd degree . It is diagnosed by the patient falling into deep sleep, lack of response to external stimuli, skin reflexes and pain;
- 3rd degree . It is caused by extensive hemorrhage and is determined by the absence of many reflexes, consciousness, and the reaction of the pupils to light;
- 4th degree . It is not comparable to life, as it is characterized by the absence of spontaneous breathing, a sharp decrease in pressure and hypothermia. All reflexes are absent. A patient in this stage of coma has virtually no chance of returning to normal life.
What do they do with a patient in intensive care?
They do everything that can stop the fatal decline in body functions, mainly these are multi-liter and many-hour droppers with various medications. In some situations, a subclavian catheter is installed, which allows not only to administer large volumes of fluid, but also to determine central venous pressure and take blood for analysis at any time. In some cases, for all manipulations, it is sufficient to place a catheter in the peripheral - ulnar vein.
In some cases, it is necessary to maintain adequate breathing with a ventilator, then a special tube is inserted into the trachea, and the patient is put into medicated sleep.
After operations on the gastrointestinal tract, a probe is installed through the nose, through which wound exudate and digestive juices produced in excess are removed.
After surgical interventions on the organs of the urinary system, a catheter can be installed in the urethra for better tissue restoration.
Each intensive care patient is connected to a monitor that informs about the respiratory and heart rate, blood pressure and oxygen concentration in the blood at the current time. At certain intervals, blood is drawn for tests.
In addition to medical procedures and infusions, the patient is given hygienic measures - treatment of the skin and mucous membranes, the “toilet” of the wound is performed - dressing, and of course, timely emptying of the bladder and intestines is monitored.
The order of the Ministry of Health requires turning the patient over in bed every 2 hours to prevent ischemia of soft tissues as a result of their compression by body weight, which threatens the development of bedsores. Bedsores are dead tissue and not only a source of toxic decay products, but also a gateway to infection. Intensive care staff often do not have the time to regularly turn patients over, nor the strength to shift large immobilized bodies, so modern intensive care units must have special anti-decubitus beds or functional beds that facilitate patient care.
METHOD OF LAST HOPE
“ECMO is the method of last hope for COVID-19 (and not only for this disease. - Ed.), ” writes a cardiac surgeon, head of the operating department of the Center for Cardiovascular Surgery of the Main Military Clinical Hospital named after. N.N.Burdenko Alexey Fedorov. And he explains: the ECMO (extracorporeal membrane oxygenation) device combines an artificial heart and an artificial lung.
This is a relatively small device with a set of hollow tubes called cannulas. The device has two main “units”: a pump and an oxygenator. The first methodically pumps the blood, the second saturates it with oxygen, Fedorov describes. In fact, life is maintained through mechanisms outside the body: the patient’s blood is driven through the apparatus, enriched with oxygen and returned back. To do this, cannulas are inserted into the vessels (into the veins and arteries or only into the veins, depending on medical indications), and the device itself works while located nearby.
The procedure for connecting and managing a patient on ECMO is extremely complex and requires high skill and long-term experience. We need a large team of specialists. “In a regular hospital, it is unreasonable to connect the device. The risk of error and fatal outcome is too high,” notes Alexey Fedorov. According to his calculations, in all of Russia today there are approximately 100 ECMO devices, which are located in specially created centers. One of these centers is equipped in the 52nd City Clinical Hospital of Moscow, where Marina Abrosimova (singer MakSim) has been staying for more than a month and a half. At the same time, about 5% of people with Covid, that is, approximately every twentieth, end up on mechanical ventilation and ECMO. What happens to the body connected to special equipment in intensive care - we talked about this with an experienced resuscitator working in the red zone of one of the Covid hospitals, Candidate of Medical Sciences Georgiy Arbolishvili .
Singer MakSim.
Photo: Evgenia GUSEVA
Can relatives not be allowed into intensive care?
The public has achieved the official right to have relatives visit a patient in intensive care, but the Ministry of Health has not yet prepared standard all-Russian rules for admission to the department, so at present everything depends on the attitude of the administration of the medical institution to this issue.
Many employees of public hospitals speak out against visiting the intensive care unit, as if relatives “bring the infection” and interfere with work, this is partly true, especially since an unconscious patient does not need the presence of relatives. Relatives are afraid that without their vigilant supervision, the patient may do something wrong or even harm. This, of course, is not true: intensive care unit staff are extremely interested in the patient’s speedy recovery and transfer to another department.
In private clinics, relatives are allowed into the ICU, at the same time showing sympathy for the misfortune and demonstrating therapeutic activity in the fight for the life and health of the cancer patient.
Forecast for recovery
The prognosis is always extremely serious. First of all, due to the fact that patients are put into an artificial coma only in the presence of severe pathologies.
The further prognosis for rehabilitation and recovery depends on the main diagnosis, the duration of the medically induced coma, the patient’s age, the presence of concomitant pathologies and complications.
Important. The longer the patient is in an induced coma, the longer the further recovery period and the lower the likelihood of full recovery.
The most optimistic prognosis is observed in patients who were put into a short-term medical coma - up to several hours. There is also a good prognosis for complete rehabilitation in patients who have been in a medical coma for up to several days.
When can relatives not be allowed into intensive care?
Relatives are not allowed in if there is a threat to the health of an intensive care patient, that is, with signs of an infectious disease, including a runny nose. The ICU patient is weak and it is extremely difficult for his body to resist infection.
Children are not allowed and there are enough reasons for that. Firstly, a child with an infection does not realize that he is not healthy, especially since his activity decreases little even at high temperatures, so parents may not notice the onset of the disease. Secondly, he may touch tubes and medical devices with his hands, run or move awkwardly, disrupting the operation of equipment and disturbing personnel. Thirdly, children take death lightly, but the shock of what they see in the hospital will disrupt the child’s psychological comfort for a long time.
When performing medical manipulations and procedures, relatives are also not needed, it is unpleasant for them to see it, and the staff feels psychological pressure.
The presence of several relatives in the intensive care unit is excessive; one or two close people for a short time is quite enough to maintain the spirit of a cancer patient; do not forget that it is hard for him, he gets tired very quickly. Sitting all night long is not good for anyone, healthy people are exhausted, and the patient is simply not aware of round-the-clock vigil at the bedside.
Epidural anesthesia: pros and cons
Thanks to epidural anesthesia, when an anesthetic is injected into the space along the spinal canal, contractions become less painful and labor is noticeably calmer - while the woman is conscious. With a good dose calculation, sensitivity disappears almost only in the pelvic area, but sensations in the legs and the ability to move them remain. This anesthesia is also called walking epidural, although in fact you won’t be able to walk - your legs will be weak, and sensors or catheters on different parts of the body will not allow you to go far. The psychological aspect is also important: when you know in advance that it won’t hurt, it’s much easier to relax and not worry.
According to Oleg Karmanov, with epidural anesthesia already performed, it is faster and easier to proceed to an emergency caesarean section, if necessary: you will not have to waste time on pain relief. But you can’t always rely on epidural anesthesia; at a certain stage of labor it is already too late to perform it. The method has a number of contraindications, including intervertebral hernia and serious circulatory and coagulation disorders. Dangerous complications of epidural anesthesia are extremely rare.
How should a relative behave in intensive care?
- You must be in clean clothes, a medical gown, clean hands, shoe covers on your feet, and a mask on your face.
- Perfume odors are irritating, since in a serious condition the sense of smell changes; you should not perfume yourself on this day.
- Phone beeps must be turned off, or better yet, all gadgets must be turned off. Maintaining silence is mandatory; loud sounds disturb staff and cause stress in patients.
- Without the permission of the staff, you cannot perform any actions with the patient: turn over, sit up, put on your feet, take you to the toilet, change clothes, and so on.
- You cannot feed - the patient receives a specific and, as a rule, very strict diet or is generally on intravenous nutrition.
- You should not give medications, homemade decoctions, pharmacy tinctures, dietary supplements and nutritional supplements previously prescribed for chronic diseases. Biological supplements may not be compatible with the medications the patient is receiving. Everything must be agreed with the attending physician.
A sick person and a patient in the intensive care unit are two very different things; some cannot recognize their loved one, his appearance changes so much. Not only because of the tubes and wires, but the tissues swell, the eyes become sunken, and the unconscious state changes facial features. Many are shocked by what they see; one must be prepared for an unpleasant experience or not enter the intensive care unit.
In the Euroonko intensive care unit they always help patients and support the spirit of relatives. We know what needs to be done and when, you can be confident in us. We do not guarantee immortality, but we help to live without suffering.
Book a consultation 24 hours a day
+7+7+78
Bibliography
- Clinical recommendations. Anesthesiology and resuscitation / ed. Zabolotskikh I.B., Shifmana E.M. - M.: GEOTAR-Media, 2016.
- Moroz V.V., Bobrinskaya I.G., Vasiliev V.Yu. and others/Cardiopulmonary resuscitation// M.: FNKTs RR, MGMSU, NIIOR, 2017.
- Order of the Ministry of Health of the Russian Federation dated November 15, 2012 N 915n “On approval of the Procedure for providing medical care to the population in the field of oncology”
- Order of the Ministry of Health of the Russian Federation dated July 4, 2017 No. 379n “On amendments to the Procedure for providing medical care to the population in the field of oncology, approved by order of the Ministry of Health of the Russian Federation dated November 15, 2012 No. 915n”
Literature
- Boisson-Bertrand, Ravussin P. 4th meeting of the anesthesia-resuscitation section of the ORL Department. Lausanne//Ann. Fr. Anesth. Reanim. – 1991.- Vol. 10(1).- 1A-2A.
- Buck M., Blumer J. Opioids and other analgesics: Adverse effects in the intensive care unit // Crit. Care Clin. — 1991.- Vol. 7.- R. 615-637.
- Chollet-Rivier M, Chiolero RL. Anaesthesia for procedures in the intensive care unit. // Curr Opin Anaesthesiol. – 2001 – V. 14(4) – P. 447-51.
- Cohen D., Horiuchi K., Kemper M. et al. Modulating effects of propofol on metabolic and cardiopulmonary responses to stressful intensive care unit procedures // Crit Care Med.- 1996.- Vol. 24.- R.612-617.
- Cohen IL, Abraham E., Dasta JF, Gallagher TJ, Papadakos PJ, Pohlman AS Management of the agitated intensive care unit patient // Crit. Care Med. - 2002. - Vol. 30. – R. 97-123.
- Durbin CGJ Sedation of the agitated, critically ill patient without an artificial airway // Crit. Care Clin. - 1995. - Vol. 11. – R. 913-936.
- Ely E.W. Delirium in Intensive Care Unit: Textbook of Critical Care Fifth Edition MP Fink. E.Abraham, JLVincent, PM Kochanek - Flsevier, 2005.- 2358 p.
- Frye MA, Coudreaut MF, Hakeman SM et al. Continuous droperidol infusion for management of agitated delirium in an intensive care unit // Psychosomatics. - 1995. - Vol. 36. – R. 301-305.
- Harvey M. Managing agitation in critically ill patients // Am. J. Crit. Care - 1996. - Vol. 5. – R. 7-15.
- Kress IP, Lacy M., Pliskin N., Pohlman A. The long term psychological effect of daily sedative interruption in critically ill patients // Am. Respira. With rit. With are Med. - 2001. - Vol. 163. R .954
- Kress JP, Pohlman AS, Hall JB Sedation and Analgesia in the Intensive Care Unit // Am. J. Respira. Crit. Care Med. – 2002.- Vol. 166. – R. 1024-1028.
- Lewis K., Whipple J., Michael K., Quehbeman EJ. Effect of analgesic treatment on the physiological consequences of acute pain // Am. J. Hosp. Pharm. - 1994. –Vol. 51. – R. 1539-1554.
- Liu J., Singh H., White PF Electroencephalographic bispectral index correlates with intra-operative recall and depth of propofol-induced sedation // Anesth. Analg. — 1997. –Vol. 84. – R. 185-189.
- Mehta S. Sedation Strategies in the Critically II // Yearbook of Intensive Care and Emergency Medicine - Edited by JI.Vincent -Elsevier - 2005.- R. 78-
- Milbrandt E.W., Ely E.W. Agitation and delirium. Critical Care. Fifth edition. Finc MR, Abraham E, 2005, chapter 2.
- Park G, Lane M, Rogers S, Bassett P. A comparison of hypnotic and analgesic based sedation in a general intensive care unit. // Br J Anaesth. – 2007. – V.98(1). – P.76-82.
- Rhoney DH, Parker DJ Use of sedative and analgesic agents in neurotrauma patients: effects on cerebral physiology // Neurol. Res. - 2001. –Vol. 23. – R. 237-259.
- Terao Y., Miura K., Saito M., Sekino M., Fukusaki M., Sumikawa K. Quantitative analysis of the relationship between sedation and resting energy expenditure in postoperative patients // Crit. Care Med. — 2003. –Vol. 31(3). - R . 830-833.
- Vinik H. Intravenous anaesthetic drug interactions: practical applications. //Eur. J. Anaesthesiol. Suppl. – 1995. – V.12. –P.13-19.