In the group of congenital heart defects, tetralogy of Fallot ranks firmly in tenth place. The prevalence among “blue” defects is half. In medical reports and reference literature, the abbreviation CHD is often used, which is synonymous with the term “congenital heart disease.”
In the International Classification of Diseases ICD-10, it is included in the group of congenital anomalies under code Q21.3. An unusual combination of disturbances in the formation of the heart and main vessels was described in 1888 by A. Fallot as a separate syndrome. His name remains in the history of medicine.
What anomalies does the syndrome consist of, anatomical features
Tetralogy of Fallot includes a combination of four anomalies:
- defect in the interventricular septum;
- right-sided position of the aorta (as if “sitting astride” on both ventricles);
- stenosis or complete fusion of the pulmonary artery, it lengthens and narrows due to rotation of the aortic arch;
- pronounced right ventricular hypertrophy of the myocardium.
Among the combinations of defects with pulmonary artery stenosis and septal defects, there are 2 more forms, also described by Fallot.
The triad consists of:
- holes in the interatrial septum;
- pulmonary stenosis;
- right ventricular hypertrophy.
Pentad - adds to the first option the damaged integrity of the interatrial septum.
In most cases, the aorta receives a large volume of blood from the right side of the heart without sufficient oxygen concentration. Hypoxia is formed according to the circulatory type. Cyanosis is detected in a newborn child or in the first years of a baby’s life.
As a result, the infundibulum of the right ventricle narrows, and a cavity is formed above it, similar to an additional third ventricle. The increased load on the right ventricle contributes to its hypertrophy to the thickness of the left.
The only compensatory mechanism in this situation can be considered the appearance of a significant collateral (auxiliary) network of veins and arteries supplying blood to the lungs. The open botal duct temporarily maintains and improves hemodynamics.
Tetralogy of Fallot is typically associated with other developmental anomalies:
- non-closure of the ductus botallus;
- accessory superior vena cava;
- additional coronary arteries;
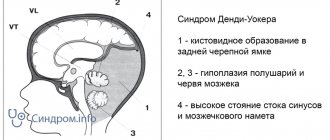
- Dandy Walker syndrome (hydrocephalus and underdevelopment of the cerebellum);
- in ¼ of patients the embryonic right aortic arch remains (Corvisart's disease);
- congenital dwarfism and mental retardation in children (Cornelia de Lange syndrome);
- defects of internal organs.
Algorithm of actions when an attack occurs
- You need to help the child squat down, or take a “knee-elbow” position. This position helps reduce venous blood flow from the lower body to the heart, and therefore reduces the load on the heart muscle.
- Oxygen supply through an oxygen mask at a rate of 6-7 l/min.
- Intravenous administration of beta blockers (for example, Propranolol at 0.01 mg/kg body weight) eliminates tachycardia.
- The administration of opioid analgesics (“Morphine”) helps to reduce the sensitivity of the respiratory center to hypoxia and reduce the frequency of respiratory movements.
- If the attack does not stop within 30 minutes, emergency surgery may be required.
Important! During an attack, drugs that increase heart contractions (cardiotonics, cardiac glycosides) should not be used! The action of these drugs leads to an increase in the contractility of the right ventricle, which entails additional blood discharge through the defect in the septum. This means that venous blood, which contains practically no oxygen, enters the systemic circulation, which leads to an increase in hypoxia. This is how a “vicious circle” arises.
Causes
The causes of the anomaly are considered to be effects on the fetus in the early stages of pregnancy (from the second to the eighth week):
- infectious diseases of the expectant mother (rubella, measles, influenza, scarlet fever);
- taking alcohol or drugs;
- treatment with hormonal drugs, sedatives and sleeping pills;
- toxic effect of nicotine;
- intoxication with industrial toxic substances in hazardous industries;
- a hereditary predisposition is possible.
The use of pesticides in the garden without respiratory protection affects not only the health of the woman, but also her offspring
The important thing is that at a short period of time a woman may not notice pregnancy and independently provoke fetal pathology.
Types of tetralogy of Fallot
It is customary to distinguish 4 types of tetralogy of Fallot according to the characteristics of anatomical changes.
- Embryological - narrowing is caused by anterior displacement of the septum to the left and low localization. Maximum stenosis coincides with the level of the anatomical demarcation muscle ring. In this case, the structures of the pulmonary valve are practically unchanged, moderate hypoplasia is possible.
- Hypertrophic - pronounced hypertrophy of the exit zone from the right ventricle and the dividing muscle ring is added to the mechanism of the previous type.
- Tubular - obstruction is caused by incorrect division in the embryonic period of the common arterial trunk, due to which the pulmonary cone (the future of the pulmonary artery) turns out to be underdeveloped, narrowed and short. At the same time, it is possible to change the valve apparatus.
- Multicomponent - all of the listed factors are partially involved in the formation.
Features of hemodynamics
The severity of the defect is determined by the degree of narrowing of the diameter of the pulmonary artery. To diagnose and determine treatment tactics, it is important to distinguish three types of anomalies:
- with complete fusion (atresia) of the arterial lumen: the most severe disorder, with a large interventricular foramen, the mixed blood of both ventricles is directed predominantly to the aorta, oxygen deficiency is pronounced, in the case of complete atresia, blood enters the lungs through the open ductus arteriosus or through collateral vessels;
- acyanotic form: with moderate stenosis, the obstacle to the blood flow from the right ventricle can be overcome by a lower pressure than in the aorta, then the blood discharge will take a favorable path from the artery to the vein, the defect variant is called “white”, since cyanosis of the skin does not form;
- cyanotic form with stenosis of varying degrees: caused by the progression of obstruction, discharge of blood from right to left; this causes a transition from the "white" form to the "blue" form.
Medical and social examination
Medical and social examination and disability in Fallot's disease MSA and disability in Fallot's triad MSA and disability in tetralogy of Fallot MSA and disability in the pentade of FallotFALLOT DISEASE (triad, tetrad, pentad) is one of the most common congenital heart defects, occurring with cyanosis and hypoxemic attacks.
ICD X headings: Q 21.3 - Q 21.8.
Epidemiology: the frequency of congenital heart defects in children is 0.8-1% of the number of newborns.
Etiology and pathogenesis. Fallot's defects are accompanied by an obstruction to the outflow of blood from the right ventricle and occur with depletion of the pulmonary circulation. There are triad, tetrad and pentad of Fallot. Fallot's triad includes pulmonary valve stenosis, ASD, hypertrophy of the right ventricular wall; tetralogy, the most common Fallot's defect, - infundibular stenosis, VSD, "ridden aorta", hypertrophy of the wall of the right ventricle; The pentad includes infundibular stenosis, ASD, “squatting aorta,” and hypertrophy of the right ventricular wall. Hemodynamic disturbances in these defects are due to the fact that an insufficient amount of blood enters the pulmonary circulation due to stenosis of the pulmonary trunk, which can be infundibular, valvular, trunk or, more often, combined, and into the systemic circulation through a VSD or ASD and displaced Venous blood is discharged to the right aorta. Spasm of the infundibular section of the right ventricle leads to the fact that most of the venous blood enters the aorta and increased hypoxia of the central nervous system, which causes the development of hypoxemic attacks in the child.
The clinical picture manifests itself in the first days of life: shortness of breath, cyanosis and systolic murmur in the second to fourth intercostal space to the left of the sternum. The epicenter of the noise depends on the location of pulmonary stenosis and VSD. With less pronounced stenosis and transposition of the aorta to the right, cyanosis appears later, in the first year of life. These defects are characterized by the sudden onset of hypoxemic attacks: the child suddenly becomes agitated, breathing quickens, cyanosis increases, and fainting (loss of consciousness) occurs within several minutes and sometimes hours. At the moment of the onset of the attack, the child takes a typical position - squats down. With the development of IDA in a child, the frequency and severity of hypoxemic attacks increase. Attacks decrease with age and after 2 years, as a rule, stop with a simultaneous increase in cyanosis. Children are lagging behind in physical development, they experience shortness of breath when feeding and moving, deformities of the fingers and toes in the form of drumsticks are detected, and chest deformities do not occur. The heart size remains normal or slightly increases to the left, and a systolic murmur is heard along the left sternal border. And the tone above the pulmonary trunk is weakened or absent, the maximum is reduced and a low pulse arterial pressure is recorded.
Complications: progressive oxygen deficiency with the development of bleeding of the mucous membranes and intracavitary bleeding as a result of disturbances in the hemomicrocirculation system; hemiparesis and paralysis due to a hypoxemic attack; chronic heart failure with the addition of collaptoid states.
Laboratory and instrumental methods confirming the diagnosis: 1) ECG (displacement of the electrical axis of the heart to the right, hypertrophy of the right atrium and right ventricle); 2) X-ray examination of the chest organs (the vascular pattern of the lungs is depleted, the heart is small in size, in the shape of a boot with a pronounced waist and a raised top); 3) EchoCG, Doppler EchoCG.
Treatment is symptomatic: emergency care for hypoxemic attacks (oxygen and aerotherapy, sedatives, cordiamin, beta-blockers, treatment of IDA), sanitation of foci of chronic infection, administration of cardiac glycosides, etc. Emergency surgery is indicated during the period of primary adaptation in severe hypoxemic attacks with progressive hypoxemia and hypoxia; radical planned surgery is performed on children over 3 years of age during the period of relative compensation of the defect. The rehabilitation period after surgery is at least 12 months.
The prognosis is serious.
Disability criteria are determined by an unfavorable prognosis and severe course of Fallot's defects; determination of disability is advisable from the moment of diagnosis, possibly in absentia; after surgical treatment, it is advisable to determine disability for at least 1 year, followed by re-examination after the examination.
Rehabilitation: medical rehabilitation during periods of exacerbations, psychological, pedagogical and professional rehabilitation during periods of relative compensation of the condition. Source
Symptoms
The clinical picture appears:
- significant cyanosis - located around the lips, in the upper half of the body, intensifies when the child cries, feeds, strains;
- shortness of breath - has a paroxysmal nature associated with physical activity, the child takes the most comfortable “squatting” position, due to a temporary reflex additional spasm of the pulmonary artery and the cessation of blood oxygen saturation by 2 times;
- fingers in the shape of “drum sticks”;
- physical underdevelopment and weakness of children; running, outdoor games cause increased fatigue, dizziness;
- convulsions - associated with hypoxia of brain structures, blood thickening, and a tendency to thrombosis of cerebral vessels.
The form of the disease depends on the age of the child, and it determines the adequacy of compensation; in a newborn, cyanosis is visible on the face, hands and feet
There are:
- early manifestations in the form of cyanosis immediately after birth or in the first 12 months of life;
- The classic course is considered to be the manifestation of cyanosis at two to three years of age;
- severe form - paroxysmal clinical picture with shortness of breath and cyanosis;
- late - cyanosis appears only by 6 or 10 years;
- acyanotic form.
An attack of shortness of breath can occur at rest: the child becomes restless, cyanosis and shortness of breath intensify, the heart rate increases, loss of consciousness with convulsions and subsequent focal manifestations in the form of incomplete paralysis of the limbs is possible.
Symptoms of the disease
Due to the fact that the disease manifests itself quite early, in the article we will focus on childhood, starting from birth. The main manifestations of tetralogy of Fallot are caused by an increase in CHF, although in such babies the development of acute heart failure (arrhythmia, shortness of breath, anxiety, breast refusal) cannot be excluded. The appearance of the child largely depends on the severity of the narrowing of the pulmonary trunk, as well as on the extent of the defect in the septum. The greater these disturbances, the faster the clinical picture develops. The appearance of the child largely depends on the severity of the narrowing of the pulmonary trunk, as well as on the extent of the defect in the septum. The greater these disturbances, the faster the clinical picture develops.
On average, the first manifestations begin at 4 weeks of a child’s life. Main symptoms:
- A bluish coloration of the skin of a child first appears when crying or sucking, then cyanosis can persist even at rest. At first, only the nasolabial triangle, fingertips, and ears appear blue (acrocyanosis), then, as hypoxia progresses, total cyanosis may develop.
- The child lags behind in physical development (later begins to hold his head, sit up, crawl).
- Thickening of the terminal phalanges of the fingers in the form of “drum sticks”.
- Nails become flattened and round.
- The chest is flattened, and in rare cases, a “heart hump” forms.
- Decreased muscle mass.
- Irregular growth of teeth (wide gaps between teeth), caries develops quickly.
- Spinal deformity (scoliosis).
- Flat feet develops.
- A characteristic feature is the appearance of cyanotic attacks, during which the child experiences:
- breathing becomes more frequent (up to 80 breaths per minute) and deeper;
- the skin becomes bluish-purple;
- pupils dilate sharply;
- shortness of breath appears;
- characterized by weakness, up to loss of consciousness as a result of the development of hypoxic coma;
- Muscle cramps may occur.
typical areas of cyanosis
Older children tend to squat during attacks, as this position makes their condition a little easier. On average, such an attack lasts from 20 seconds to 5 minutes. However, after it, children complain of severe weakness. In severe cases, such an attack can lead to a stroke or even death.
Diagnostics
The diagnosis is made by observing the child and the presence of objective signs. Information from relatives about development and activity, attacks with loss of consciousness and cyanosis are taken into account.
When examined in children, attention is drawn to the cyanotic nature of the lips and the altered shape of the terminal phalanges of the fingers. Rarely does a “heart hump” form.
On percussion, the borders of the heart are not changed or expanded in both directions. During auscultation, a rough systolic murmur is heard to the left of the sternum in the fourth intercostal space due to the passage of blood flow through the hole in the interventricular septum. It is better to listen to the patient in the supine position.
On the radiograph, the contours of the cardiac shadow resemble a “shoe” directed to the left
Due to the absence of the pulmonary artery arch, retraction occurs in the place where the vessels are usually located. A depleted lung appears more transparent. Enlargement of the heart to a large size does not occur.
A general blood test determines the adaptive response to hypoxia in the form of an increase in the number of red blood cells and an increase in hemoglobin.
Ultrasound diagnostics using a conventional ultrasound machine or Doppler ultrasound allows you to accurately determine changes in the chambers of the heart, abnormal development of blood vessels, the direction and magnitude of blood flow.
The ECG shows signs of right-sided cardiac hypertrophy, possible right bundle branch block, and the electrical axis is significantly deviated to the right.
Probing of the cavities of the heart with measurement of pressure in the chambers and vessels is carried out in specialized clinics when deciding on surgical treatment.
Less commonly, coronary angiography and magnetic resonance imaging may be required.
In differential diagnosis, it is necessary to exclude a number of diseases:
- transposition of the pulmonary artery causes a significant enlargement of the heart as the child grows;
- fusion at the level of the tricuspid valve promotes hypertrophy not of the right, but of the left ventricle;
- Eisenmenger's tetralogy - a defect accompanied not by fusion, but by dilation of the pulmonary artery; its pulsation and characteristic pattern of pulmonary fields are determined on an x-ray;
- stenosis of the pulmonary artery lumen is not accompanied by a “shoe” picture.
Doppler ultrasound helps to distinguish atypical forms.
Treatment
Drug therapy for a patient with tetralogy of Fallot is carried out only for the purpose of preparing for surgery or in the postoperative period. The only goal is to support the myocardium, preventing possible thrombosis after attacks and impaired coronary and cerebral circulation.
The patient is shown:
- inhalation of an oxygen-air mixture through nasal catheters or in an oxygen tent; newborns are kept in special intensive care units to reduce hypoxia;
- A solution of Reopoliglyukin, Eufillin is administered intravenously (in the absence of tachycardia);
- due to tissue acidosis, sodium bicarbonate solution is required.
It is impossible to treat a patient without surgical assistance
Operations can be:
- emergency measure of temporary assistance;
- shunt type for relieving blood flow along a new channel;
- a radical choice with correction of the ventricular septal defect and the location of the aorta.
As an emergency, the creation of an artificial connection (anastomosis) between the aorta and pulmonary artery using a prosthesis is used.
It is used as the first stage of surgical intervention for newborns and young children. It is believed that such actions allow you to prepare the child and avoid complications during further treatment, reducing the risk to 5–7%.
It is necessary to decide on the final planned correction of the defect before the age of three years. Temporary anastomoses can be performed between the subclavian and pulmonary arteries.
Radical surgery includes plastic surgery of the right ventricular exit cone, elimination of a hole in the interventricular septum, and valvotomy (dissection of an overgrown pulmonary valve). It is performed on an open heart and requires the use of a heart-lung machine.
The first days after surgery already show improvement in hemodynamics
Possible complications and prognosis
The most common complications after surgery are:
- Preservation of narrowing of the pulmonary trunk (with insufficient dissection of the valve).
- When the fibers that conduct excitation in the heart muscle are injured, various arrhythmias may develop.
On average, postoperative mortality is up to 8-10%. But without surgical treatment, the life expectancy of children does not exceed 12-13 years. In 30% of cases, the death of a child occurs in infancy from heart failure, stroke, or increasing hypoxia.
However, with surgical treatment performed on children under 5 years of age, the vast majority of children (90%) upon re-examination at the age of 14 years do not reveal any signs of developmental lag from their peers.
Moreover, 80% of operated children lead a normal lifestyle, practically no different from their peers, except for restrictions on excessive physical activity. It has been proven that the earlier a radical operation is performed to eliminate this defect, the faster the child recovers and catches up with his peers in development.
Is registration of a disability group indicated for illness?
All patients before undergoing radical heart surgery, as well as 2 years after the operation, are required to register for disability, after which re-examination is carried out.
When determining the disability group, the following indicators are of great importance:
- Are there any circulatory problems after surgery?
- Does pulmonary artery stenosis persist?
- The effectiveness of surgical treatment and whether there are complications after surgery.