Arterial hypertension (AH, arterial hypertension) is a pathological condition that leads to increased blood pressure, as a result of which the structure and function of the arteries and heart are disrupted.
Medical statistics claim that 30-40% of the world's inhabitants suffer from hypertension. Among people over 65 years of age, the disease is registered in 70%.
1
ABPM in the diagnosis of hypertension
2 Diagnosis of hypertension at MedicCity
3 Diagnosis of arterial hypertension
Hypertension significantly affects the quality of life: it causes attacks of headaches and dizziness, and affects performance. With long-term hypertension, irreversible changes occur in human organs and systems that threaten not only health, but also life itself.
Target organs for arterial hypertension:
- heart (left ventricular hypertrophy, heart failure, angina, myocardial infarction, etc.);
- brain (hypertensive encephalopathy, ischemic or hemorrhagic stroke, dementia);
- blood vessels (reduced arterial patency, aortic aneurysm);
- eyes (hemorrhages, retinal lesions, blindness);
- kidneys (renal failure).
1 ABPM for hypertension
2 ABPM for hypertension
3 ECHO-CG for hypertension
Blood pressure indicators for hypertension
The main manifestation of hypertension is a long-term and persistent increase in blood pressure (BP).
There are systolic (or upper) blood pressure, which shows the level of blood pressure at the moment the heart contracts, and diastolic (lower), which shows the level of blood pressure at the moment the heart relaxes.
Normal blood pressure levels are considered to be 120-134/80-84 mmHg, but data may vary due to emotional shocks, physical activity, changes in air temperature, etc. These fluctuations are normal; they reflect the body’s naturally programmed reaction to changes in living conditions. However, constantly elevated blood pressure in the absence of obvious reasons for this is a significant reason to take care of your health.
Arterial hypertension is indicated by a stable increase in blood pressure (systolic - above 140 mm Hg, diastolic - above 90 mm Hg when measured at a doctor’s appointment; 135/85 mm Hg and above - when measured independently) , confirmed by repeated measurements. To establish a diagnosis of arterial hypertension, two measurements with elevated blood pressure in the absence of physical and emotional stress are sufficient.
How is it diagnosed?
Interviewing the patient will help in making a preliminary diagnosis. Systolic-diastolic arterial hypertension can be detected through a general examination of the patient and questioning him about disturbing clinical manifestations. To confirm the diagnosis, blood pressure is monitored throughout the day. It is also important to do an ultrasound diagnosis of the heart and kidneys to exclude possible pathologies of these organs. It is recommended to conduct magnetic resonance and computed tomography of the brain and undergo a general and biochemical blood test.
Degrees of arterial hypertension
In modern cardiology, several classifications of arterial hypertension are used.
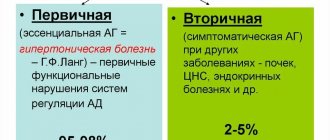
Classification by origin
Arterial hypertension can be an independent disease (hypertension). Or act as a sign of diseases of other organs, systems - endocrine glands (thyroid, adrenal glands), kidneys, heart, blood vessels. And also be the result of taking certain medications. In this case, we will talk about symptomatic (or secondary arterial hypertension).
The classification of hypertension according to blood pressure level, adopted by WHO, distinguishes three degrees of arterial hypertension:
1st degree (soft) - 140-159/90-99; 2nd degree (average) - 160-179/100-109; 3rd degree (severe) - 180/110 and above;
Isolated systolic hypertension is distinguished separately - SBP is above 180, DBP is below 90.
According to the degree of target organ damage, three stages of arterial hypertension are distinguished:
- at the first stage of arterial hypertension, an increase in blood pressure is not accompanied by changes in target organs;
- at the second stage, there is a persistent increase in blood pressure and organic changes in internal organs (however, without significant impairment of their functions). At this stage of the development of hypertension, signs of atherosclerotic damage to large vessels, narrowing of the retinal arteries, hypertrophy of the left ventricle of the heart may be detected; there is an increase in the level of creatinine in the blood and protein in the urine;
- at the third stage of arterial hypertension, a significant increase in blood pressure is associated with pathological changes in target organs and severe impairment of their functions (myocardial infarction, acute cerebrovascular accident, retinal hemorrhages, etc.).
1 Ultrasound of the heart for hypertension
2 ECG for hypertension
3 Diagnosis of hypertension at MedicCity
results
- The analysis included 9590 adults from the NHANES study (mean age 49 years, 52% women) and 8703 adults from the ARIC study (mean age 56 years, 57% women).
- The prevalence of isolated diastolic hypertension was 6.5% in NHANES according to 2017 ACC/AHA criteria and 1.3% according to JNC7 criteria. Absolute difference, 5.2% [95% CI, 4.7%-5.7%].
- According to the criteria, 0.6% of patients required antihypertensive therapy.
- Analysis of data from the ARIC study showed that isolated diastolic hypertension, according to the 2021 ACC/AHA criteria, was not significantly associated with the incidence of atherosclerotic cardiovascular disease (hazard ratio, 1.06 [95% CI, 0.89-1.26]) , heart failure (hazard ratio, 0.91 [95% CI, 0.76-1.09]) or chronic kidney disease (hazard ratio, 0.98 [95% CI, 0.65-1.11]).
Signs of arterial hypertension
Often, hypertension has no symptoms at all other than persistent high blood pressure. At the same time, not every person constantly monitors their blood pressure levels, so arterial hypertension is often detected very late.
Contact your cardiologist immediately if you regularly notice signs of hypertension such as:
- headaches in the occipital region;
- dizziness;
- “flies”, a veil before the eyes;
- noise in ears;
- rapid and increased heartbeat;
- unpleasant tightness or pain in the chest;
- swelling of the arms and legs, puffiness of the face.
Hypertensive crisis is an emergency condition caused by an excessively high level of blood pressure (for example, up to 200/110 mm Hg and above), it is characterized by: headache, tremor, increased heart rate, chills, nausea, vomiting, sudden fear of death, anxiety , facial redness, swelling, sweating, vision distortion.
1 Ophthalmoscopy in the diagnosis of hypertension
2 Ophthalmoscopy for hypertension
3 Taking tests to diagnose hypertension
Isolated systolic arterial hypertension in the elderly
O. Kislyak, A. Alieva, T. Kasatova,
Russian State Medical University
Arterial hypertension (AH) remains one of the most important medical problems, and its presence in different age groups largely determines cardiovascular morbidity and mortality. This is especially true for older people, who often have concomitant diseases, numerous target organ damage and are exposed to a variety of risk factors.
In recent years, interest in the health of older people and the quality of life of this category of patients has increased significantly. This is due, first of all, to the fact that in all economically developed countries the number of older people is growing much faster than the total population. Moreover, special attention is paid to cardiovascular pathology, which is the main cause of death in this age category of patients. That is why the geriatric aspects of arterial hypertension are being intensively studied, and many outdated ideas about approaches to the treatment of hypertension in elderly patients are being revised.
Isolated systolic arterial hypertension (ISAH) occupies an important place in the structure of hypertension in this group of patients. This term is used to describe all patients with systolic blood pressure equal to or greater than 140 mmHg and diastolic blood pressure <90 mmHg.
The prevalence of ISAH among older people is 15-20%, and its frequency increases with age, starting from 55 to 80 years. The development of ISAH is most common in women, overweight patients and patients with diabetes mellitus.
Unfortunately, today we can state that, despite the increased popularization of modern ideas about the diagnosis, prognosis and treatment of ISAH, they have not yet become the property of all doctors, which cannot but affect the results of blood pressure control in elderly patients.
Data obtained during the Russian scientific and practical program “Improving the detection, assessment and treatment of arterial hypertension in people over 55 years of age” (ARGUS) showed that only 61.2% of doctors were informed about the age-related dynamics of SBP, and 36% were informed about the dynamics of DBP. , about the diagnosis of ISAH - 53.2. To be fair, it should be noted that quite recently the attitude towards ISAH among practicing doctors was even calmer. The severity of hypertension has traditionally been associated with an increase in diastolic blood pressure, and this is what determined the medical approach to elderly patients. Thus, elderly people with DBP < 90 mm Hg. were not considered to have a poor prognosis and, in many cases, did not receive treatment. However, it has been shown that an increase in SBP with age is usually accompanied by a decrease in DBP, which is associated with a decrease in the elasticity of large arteries and a decrease in the reactivity of the vascular wall in response to the ejection of blood from the heart. In such patients, the incidence of cardiovascular complications increases significantly. This has been convincingly shown in a number of studies (Framingham, Copenhagen, MRFIT).
Today we have a clear understanding that the risk of cerebral stroke, ischemic heart disease and myocardial infarction is more closely related to systolic blood pressure than to diastolic blood pressure. With regard to ischemic heart disease, it increases by 3.7 times with an increase in SBP and by 2.8 times with an increase in DBP, and the risk of cerebral stroke increases with an increase in SBP and DBP by 8.2 and 4.4 times, respectively. The Honolulu study, which followed for 20 years, found that the incidence of stroke was higher in patients with SBP >160 and DBP <90 mmHg than in patients with SBP >160 and DBP >90 mmHg.
Not only the value of SBP is very important, but also pulse blood pressure, which increases in the elderly when ISAH occurs. Pulse blood pressure was found to be an independent predictor of cardiovascular mortality in a population of women 40–69 years of age with hypertension and men with or without hypertension.
There were other circumstances that hampered the implementation of active treatment therapy in elderly patients with ISAH. This was primarily driven by concerns that drug therapy might further reduce DBP and thereby reduce coronary blood flow—the “J effect” discovered by Cruickshank et al. However, it was then proven that a decrease in blood pressure even below 80 mm Hg. does not worsen the prognosis and does not increase the incidence of cardiovascular complications, including heart failure.
It has also been suggested that prevention of severe and fatal complications of hypertension (the ultimate goal of treatment in patients with hypertension) cannot be achieved in elderly people with sclerotic changes in the large arteries. This view was subsequently refuted, and it was demonstrated that treatment resulted in a greater reduction in cardiovascular mortality in patients than in younger patients.
Thus, recent data on ISAH in the elderly allow us to conclude that it requires much more attention than it received in previous years.
The basic principles of treatment of ISAH in old age include complex therapy using non-drug and drug methods to prevent the development of severe cardiovascular complications. The goal of treatment is to reduce SBP to <140 mmHg.
Non-drug treatment consists primarily of limiting salt intake. The pathogenetic basis is the fact that a significant number of patients with ISAH in old age are characterized by increased sensitivity to sodium chloride (this is especially typical for postmenopausal women - high salt sensitivity is observed in 30-50% of cases). Simply limiting salt intake in many cases can significantly reduce blood pressure in this category of patients.
Other non-drug treatment methods are: smoking cessation, a cholesterol-lowering diet and a dosed increase in physical activity, which promotes weight loss and has a beneficial effect on SBP levels.
However, non-pharmacological methods alone cannot guarantee adequate control of blood pressure in elderly patients. It is recommended to begin drug therapy in this category of patients immediately after the diagnosis of ISAH is established.
Modern ideas about the pharmacotherapy of ISAH are based on the results of a number of large studies, primarily the STOP-Hypertension, SHEP, Syst-Eur, Syst-China, etc. studies.
Preference is given to diuretic drugs, which are first-line drugs for this pathology. In cases where treatment with diuretics is impossible, it is recommended to use calcium antagonists of the dihydropyridine series (their prescription for elderly patients is justified in the presence of coronary artery disease and cardiac arrhythmias).
Beta-blockers are currently not recommended as first-line drugs for the treatment of ISAH in elderly patients and are usually prescribed to patients who have had a myocardial infarction, but not as monotherapy. ACE inhibitors can be used as second-line drugs, the effectiveness of which in reducing SBP in elderly patients has been shown in some studies (CARE). They may be added to diuretic or calcium antagonist therapy. The advisability of using ACE inhibitors in elderly patients with ISAH is also due to the fact that some of them, for example perindopril, increase the elasticity of the arteries, and, as mentioned earlier, ISAH in the elderly is characterized by a decrease in arterial compliance and high rigidity of the vascular wall. As for AT II receptor blockers, the lack of data on the effect on endpoints in hypertension and the limited experience of their clinical use do not yet allow us to judge their role in the treatment of ISAH in elderly patients. Research in this direction is underway.
In many cases, when treating elderly patients with ISAH, combination therapy should be used, because optimal reduction in SBP to 140 mm Hg. not always possible with monotherapy. Recently, the attention of cardiologists has been attracted by a new method of combination therapy using a fixed low-dose combination, an example of which is the combination of perindopril (2 mg) and indapamide (0.625 mg).
It is recommended to start therapy with low doses of thiazide and thiazide-like diuretics (hydrochlorothiazide, chlorthalidone, indapamide in regular and retard forms).
Positive effects and high efficiency have been proven in ISAH in relation to hydrochlorothiazide and chlorthalidone. The effectiveness and possibility of preventing cardiovascular complications (cerebral and coronary) when treated with these drugs has been proven. It was possible to establish that hydrochlorothiazide and chlorthalidone can be successfully used in elderly patients and in the presence of diabetes mellitus. These drugs are not only not inferior to the so-called new antihypertensive drugs, but also have significant advantages in terms of cost/effectiveness.
The latest international and Russian recommendations contain a number of requirements that the antihypertensive drug used must meet. These include: effectiveness, the possibility of prescribing a minimum dose and, to improve the patient’s adherence to treatment, a single dose per day. Not all thiazide diuretics meet these requirements. In addition, you must always remember the side effects that occur with long-term diuretic therapy (hypokalemia, hyperuricemia, orthostatic hypotension, lipid metabolism disorders, etc.).
Therefore, doctors are showing increasing and justified interest in the retard form of indapamide - a thiazide-like diuretic with a slow release, prescribed in a daily dose of 1.5 mg (indapamide SR 1.5 mg). This drug has a dual mechanism of action. On the one hand, it provides a slight increase in diuresis, eliminating excess sodium content in the vascular wall, on the other hand, it causes a primary vasodilating effect due to the regulation of calcium entry into smooth muscle cells and the influence on the synthesis of prostaglandins. The results of treatment with this diuretic confirmed its clear hypotensive effect. In terms of its antihypertensive effect, it is not inferior to enalapril at a dose of 20 mg and amlodipine at a dose of 5 mg. The antihypertensive activity of indapamide 1.5 mg sustained release lasts for 24 hours, and sensitivity to the drug persists for a long period (more than 1 year), while a year after the start of treatment with chlorthalidone, blood pressure is controlled in only 30% of patients.
Indapamide 1.5 mg has a unique form, which made it possible to change the pharmacokinetics of the drug. With its use, a constant concentration of the active substance in the blood is maintained throughout the day, which ensures blood pressure control without sudden fluctuations, and the high bioavailability of the drug allows you to prescribe a minimum dose of indapamide, which leads to a reduction in side effects. It does not affect the lipid spectrum and carbohydrate metabolism. Currently, it can be considered the safest diuretic for the treatment of patients with hypertension and diabetes mellitus.
Treatment with this drug, compared with other thiazide diuretics and immediate-release indapamide 2.5 mg, significantly (50%) reduces the incidence of hypokalemia. According to many authors, only 1% of patients taking indapamide 1.5 mg develop hypokalemia, and the average decrease in potassium levels is only 0.3 mmol/l.
Of particular note is the effect of indapamide 1.5 mg sustained release on left ventricular myocardial hypertrophy, which is reasonably considered an important independent risk factor for cardiovascular disease and is often found in patients with ISAH. The LIVE study showed that treatment with this drug reversed left ventricular hypertrophy.
Our experience with the use of indapamide 1.5 mg sustained release in elderly patients with ISAH shows the high efficacy and safety of this drug.
We assessed its effectiveness in a group of patients with stable ISAH, in whom the SBP load time index during the day, according to 24-hour BP monitoring (ABPM), was at least 50%. Another feature of the study was that the patients belonged to the group of so-called borderline hypertension (SBP within 140-149 mm Hg, DBP <90 mm Hg). Indapamide 1.5 mg sustained release was used as monotherapy for 8 weeks.
The dynamics of ABPM in patients receiving monotherapy with indapamide retard were characterized by a clear hypotensive effect of the drug. A decrease in SBP per day, day and night by 12.1 was determined; 8.8 and 8.9%, respectively, which is somewhat less than reported in other studies, but apparently due to the characteristics of the group (borderline hypertension). A significant decrease in the SBP load index was found during the day by 51.4, during the daytime by 47.5 and especially at night by 58.8%.
It is important to note the more pronounced effect of indapamide retard on the night phase of the circadian blood pressure rhythm. In our opinion, this effect is one of those positive properties of the drug that determine the usefulness of its use in elderly patients, in particular with ISAH, because nocturnal hypertension is a risk factor for the development of left ventricular hypertrophy.
In addition to 24-hour blood pressure monitoring data, we simultaneously studied 24-hour heart rate variability using the Delmar system.
It is known that reduced heart rate variability is considered by many researchers as a predictor of cardiovascular morbidity and mortality. We found that in elderly patients with borderline ISAH with stable hypertension, a decrease in heart rate variability was observed in 70% of patients before treatment. After 8 weeks of therapy with indapamide retard, it was found that in patients with normal heart rate variability, the increase in all main indicators was 2-4%. In patients who initially had a decrease in heart rate variability, they increased. Only one patient with initially reduced heart rate variability did not experience a significant increase during therapy. At the same time, the hypotensive effect of indapamide retard in the same patient was adequate. The question of the effect of antihypertensive drugs on heart rate variability requires further study.
Our data indicate that indapamide 1.5 mg sustained release can be successfully used as monotherapy in patients with borderline ISAH with high SBP load index scores and reduced heart rate variability.
In conclusion, I would like to note the exceptional importance of timely diagnosis and treatment of ISAH in elderly patients, the need to use thiazide diuretics as first-line drugs for the treatment of this condition, as well as the significant advantages of using indapamide 1.5 mg sustained release in this category of patients with ISAH.
The article was published in the journal “Pharmaceutical Bulletin”
Reasons for the development of arterial hypertension
The exact cause of the development of hypertension has not yet been established, however, a clear relationship has been identified between hypertension and the following factors:
- Exposure to stress;
- hereditary predisposition;
- age;
- gender (AH is more common in men);
- abuse of table salt;
- smoking and alcohol;
- endocrine disorders;
- excess body weight;
- physical inactivity;
- kidney diseases;
- increased adrenaline levels;
Complications of arterial hypertension
Under conditions of constantly elevated blood pressure, the walls of blood vessels thicken and lose their ability to relax, which prevents normal blood supply and saturation of tissues and organs with oxygen and nutrients. Various serious complications arise, including the following:
- Hypertensive crisis;
- myocardial infarction;
- stroke;
- angina pectoris;
- heart failure;
- cardiac ischemia;
- chronic renal failure;
- retinopathy;
- atherosclerosis, etc.
Complications and treatment of hypertension
Constantly elevated diastolic pressure leads to very serious, life-threatening complications, such as:
- A certain type of stroke called subarachnoid hemorrhage.
- Congestive heart failure.
- Kidney failure.
- Abdominal aortic aneurysm.
There is compelling evidence that high diastolic blood pressure is correlated with dementia.
Studies have shown that successful treatment of high diastolic blood pressure significantly reduces the risk of developing Alzheimer's disease.
The danger of increased lower pressure consists of the following deviations:
- the occurrence of a stroke;
- improper functioning of the heart;
- impaired renal function;
- aneurysm of vessels located in the abdominal cavity;
- infrequently, but the development of dementia (Alzheimer's disease) can still be triggered.
Increased diastolic pressure must be dealt with. For this, the patient will need a full examination and hospitalization. After receiving the results, a diagnosis is made and a treatment method is selected. In some cases, surgery may be recommended. This occurs when pathology of the aortic valve is detected.
- Products that will help remove salts from the body.
- Medicines that reduce heart rate.
- Drugs that can block calcium channels.
- Drugs for the treatment of heart and kidney failure.
The doctor prescribes treatment for each patient individually. Prescriptions cannot be used for a person with a similar problem. With long-term treatment and the right approach, a positive effect can be achieved: tension in the blood vessels will be relieved, and the functioning of diastole (heart muscle) will be restored. Then the heart will work in a normal rhythm and all other organs will not experience a lack of blood and oxygen.