Transesophageal pacing
– a non-invasive procedure aimed at obtaining a recording of biological potentials from the outer surface of the heart, using special esophageal electrodes and recording equipment.
Carrying out special types of stimulation to study the electrophysiological properties of the conduction system, atrial and ventricular myocardium. Identification of arrhythmia substrates, their localization and electrophysiological characteristics. Monitoring drug and/or non-pharmacological therapy.
Non-invasive electrophysiological examination of the heart (TEPS)
The experience of using TEES in cardiology spans more than 30 years.
In our country, the first report on the use of TEES in patients with coronary heart disease appeared in the scientific medical literature more than 10 years ago.
Over this period of time, the attitude towards any research method has already become stable, and the capabilities of the method itself have been well studied.
It should be said that the attitude of cardiologists to the TEES method during this time changed depending on the development of cardiology itself and the technical capabilities of the stimulators used.
The increased interest in this method is currently due, on the one hand, to the rapid development of cardiology itself as a science, in particular its arrhythmology, as well as the emergence of modern stimulators with good technical characteristics that allow the study to be carried out with minimal discomfort for the patient.
The use of TEE helps solve three main problems: diagnosis, treatment
(therapeutic, selection of antiarrhythmic drugs) and
prognosis
in many clinical situations.
The essence of the method, advantages and disadvantages
The essence of an EFI examination of the heart is as follows:
- Typically, various heart rhythm disturbances or coronary heart disease can be determined based on a standard electrocardiogram.
- If arrhythmia or myocardial ischemia cannot be detected using a single ECG, the doctor prescribes 24-hour monitoring of blood pressure and Holter ECG. Under conditions of normal household activity, the indicated diseases can be registered in most cases during the day.
- If it is not possible to track them on the monitor, the patient performs exercise tests. As a rule, based on such tests (bicycle, treadmill, 6-minute walk test), an accurate diagnosis is established, since the heart is under conditions of increased stress, but increased naturally (walking, running).
- When the above methods do not reliably establish the diagnosis of arrhythmia or ischemia, and the patient still has cardiac complaints, he is prescribed EPI (electrophysiological study of the heart)
.
With EPI, the load on the heart also increases, but not as a result of physical activity, but as a result of electrical stimulation of the myocardium
.
Such stimulation is carried out using electrodes, which begin to supply electrical currents of physiological power to the heart muscle, but at a high frequency. As a result, the myocardium contracts faster, causing a provoked increase in heart rate. And at a high heart rate, either arrhythmia or ischemia occurs if a person already has pathological processes in the myocardium, which are prerequisites for the development of these diseases. In other words, EPI allows you to provoke the desired diseases and register them on an ECG for the purpose of further treatment of the patient.
But depending on how the electrodes are applied to the heart muscle, there are three types of techniques:
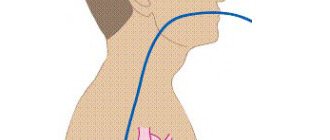
insertion of an electrode during transesophageal EPI
- Transesophageal EPI (TEPI)
.
The electrodes are supplied using a probe inserted into the lumen of the esophagus. It is a non-invasive technique, and its technique is similar to conventional fibrogastroscopy. Performed more often than the next two types of EFI. (We will not dwell on the technique of conducting PPE in this article in too much detail; there is a separate material about it). - Endocardial EPI (endoEPI)
. It is an invasive technique; electrodes are inserted into large vessels using a sterile probe and advanced under the control of X-ray equipment. Refers to high-tech types of medical care (HTMP). Despite the complexity of implementation, as well as the need to use high-quality personnel and expensive technical equipment, it is a very informative diagnostic method, and it identifies cardiac diseases better than TEE. - Epicardial EPI (epi-EPI)
. It is also an invasive technique when myocardial stimulation is performed during open-heart surgery with an incision into the chest (thoracotomy). In terms of information content, it is not inferior to endoEFI. Due to such a disadvantage as the need for thoracotomy, it is performed mainly during heart surgery for other diseases.
insertion of a catheter into the heart during invasive endoESI
Assessment of coronary circulation using the TEES method
This stimulation program is the basis from which the TEES method began as one of the stress tests (rhythm load) in cardiology.
The use of a stimulation program allows you to gradually and dosedly increase the frequency of ventricular contractions with constant assessment of changes in the final part of the ventricular complex on the monitor and when recording an ECG.
The use of TEES to assess coronary circulation allows the cardiologist to solve a number of important problems:
1. establish the very fact that the patient has coronary heart disease (CHD) and its forms, in particular, determine painless myocardial ischemia; 2. determine the degree of coronary insufficiency; 3. determine the optimal effective dose of the antianginal drug and the frequency of its administration; 4. to identify a group of patients with coronary heart disease with severe coronary insufficiency, for whom coronary angiography and possible surgical treatment of coronary artery disease are strongly recommended; 5. determine the prognosis and management tactics for patients with coronary artery disease after myocardial infarction; 6. identify a group of patients with coronary artery disease who have a high risk of sudden cardiac death for the purpose of preventive treatment; 7. carry out differential diagnosis of post-infarction cardiosclerosis in patients with Wolff-Parkinson-White syndrome; 8. identification of hidden forms of rhythm and conduction disorders; 9. when dynamically performing TES in the same patient with coronary artery disease, indirectly judge the rate of progression of coronary atherosclerosis and the effectiveness of the treatment.
In addition to general contraindications, performing TES according to the coronary circulation assessment program is not advisable in the following cases:
1. in the presence of persistent complete blockade of the left bundle branch; 2. when recording an obvious (manifesting) syndrome of premature excitation of the ventricles caused by the functioning of the Kent bundle on a resting ECG; 3. a patient with coronary artery disease with 3-4 functional class; 4. in a patient with new-onset angina during the first 4 weeks and in a patient with unstable angina; 5. during the first 3 weeks of uncomplicated myocardial infarction; 6. with pronounced hypertrophy of the left ventricular myocardium with secondary changes in the final part of the ventricular complex on the ECG. TEES is carried out as prescribed by the attending physician 2 hours after a meal against the background of withdrawal of coronary drugs in the case of a diagnostic study. In this case, the patient’s consent to perform TES, recording a resting ECG and echocardiogram (EchoCG) is required.
The stimulation program for the purpose of assessing coronary circulation is quite simple. After obtaining a stable pacemaker rhythm that exceeds the natural heart rate by 20 pulses/min, continuous stepwise stimulation is performed. The duration of each stage is 1 minute.
If there are no changes at the end of the step, the stimulation frequency is increased by 10-20 pulses/min. until a maximum frequency of 160 pulses/min is reached. After each stage of stimulation, the coronary circulation is assessed by changes in the ST segment on the ECG.
If, after reaching the maximum frequency (160 pulses/min.), no ischemic changes are observed on the ECG, then the stimulation time is extended to 2 minutes, after which a final assessment of the study is carried out. It is considered inappropriate to assess coronary circulation at a stimulation frequency of more than 160 pulses/min. at the same time, the number of false-positive results increases significantly, which is partly due to the so-called post-depolarization syndrome.
Post-depolarization syndrome is expressed in the occurrence of ST segment depression and T wave inversion on the ECG after the cessation of high ventricular frequency. The development of this syndrome after relief of paroxysm of ventricular tachycardia is well known.
In the absence of verified coronary artery disease in a patient, this syndrome indicates disturbances in the processes of ventricular repolarization not associated with deterioration of coronary circulation.
to the top of the page
When is EPI indicated?
Any type of EPI is carried out if the patient has certain complaints that the doctor cannot associate with disorders identified by the ECG or which arise in the patient with satisfactory examination results, or when certain diseases are suspected.
Thus, invasive cardiac EPI is performed when symptoms of the following nature occur:
- Paroxysmal interruptions in the work of the heart, especially short-term, but causing significant subjective discomfort,
- Interruptions in the heart, accompanied by severe general poor health, as well as shortness of breath and wheezing in the chest at rest, blue discoloration of the nasolabial triangle or the skin of other parts of the body (cyanosis), severe pallor of the skin, very high or low blood pressure, intense pain in the chest or in the chest on the left,
- Loss of consciousness and presyncope, with the exception of pathology of the central nervous system or other diseases (in the case of cardiac causes, loss of consciousness is called an attack or the equivalent of a Morgagni-Adams-Stokes attack, an attack of MES),
- Episodes of cardiac arrest (asystole) leading to clinical death with successful resuscitation of the patient.
Among the diseases that require invasive cardiac electrophysiology to clarify the diagnosis, the following can be noted:
- Paroxysmal types of arrhythmias - atrial fibrillation-flutter, supraventricular tachyarrhythmia, frequent ventricular extrasystole with transition to ventricular tachycardia,
- Sick sinus syndrome (SSNS), accompanied by alternating tachy- and bradycardia (tachy-brady syndrome), as well as bradycardia with the above-mentioned attacks of MES,
- Ventricular fibrillation with transition to asystole,
- Cardiac ischemia.
In the case where TEE does not help to reliably establish or exclude a diagnosis, that is, in diagnostically unclear cases, the patient undergoes endo- or epi-EPI.
In addition, endoEPI is carried out as part of an intraoperative examination when performing an intravascular RFA (radiofrequency ablation) operation, in which the pathological paths of the impulse that are the cause of one or another type of arrhythmia are destroyed by an intracardiac probe.
How is a transesophageal electrophysiological study performed?
TEE can be carried out in an outpatient or inpatient department of functional diagnostics. After measuring blood pressure and pulse rate, a baseline electrocardiogram is taken. Then the throat is treated with an anesthetic solution to alleviate discomfort when the probe is inserted.
TPE probe
A sterile tube with a tip that is equipped with an electrode for generating signals is passed through the nose or mouth. Sensors for a standard ECG are fixed on the chest. The depth of insertion of the device is 35 - 40 cm. If all stages were successful, then the supply of electrical impulses begins. During this time, there may be frequent heart contractions or a burning sensation in the chest.
The procedure itself lasts about half an hour. At this time, the doctor applies an electric current to the myocardium and takes readings of its activity with a cardiograph. During TPE, there is discomfort, but there is no severe pain.
In what cases is EPI contraindicated?
Any type of cardiac EPI has a number of contraindications. These include the following:
- The patient develops an acute heart attack or stroke,
- The occurrence of fever, acute infectious disease,
- Unstable angina (new or progressive),
- Suspicion of pulmonary embolism (PE),
- Acute surgical pathology,
- Severe decompensation of chronic diseases (diabetes mellitus, bronchial asthma),
- Development of acute heart failure (cardiac asthma, pulmonary edema), or severe decompensation of chronic heart failure,
- Decompensated heart defects,
- Stage III of chronic heart failure,
- Severe dilated cardiomyopathy with low ejection fraction (less than 20=30%).
How to prepare for the procedure?
All nuances of preparation for the study must be carefully explained by the doctor to the patient. Firstly, the patient (under the supervision and as directed by a doctor!) must stop taking any antiarrhythmic drugs, as they can distort the results of the study. Secondly, before the TPE procedure, a patient experiencing even slight discomfort from the stomach must undergo fibrogastroscopy in order to exclude acute gastroesophageal pathology.
Before the endoEPI procedure for attacks of loss of consciousness, a neurologist must exclude brain pathology that could cause fainting, and this may require a CT scan or MRI of the skull.
Due to the fact that endo- or epi-EPI requires hospitalization in a hospital, a patient undergoing a routine examination must provide the doctor with the results of tests for HIV, syphilis, hepatitis and blood clotting no later than two weeks ago (different institutions have their own deadlines) .
The study is carried out strictly on an empty stomach. The need for epi-EPI on an empty stomach is due to the fact that during general anesthesia, vomiting of eaten food or liquid and aspiration of vomit may occur.
After the necessary preparation, the patient is hospitalized in a hospital. He must have the results of the examination (ultrasound of the heart, 24-hour monitor), as well as an extract from the outpatient card or discharge summary from the institution where he received examination and treatment before. The extract must indicate the rationale for the need for EFI with a detailed clinical diagnosis.
Indications
- Attacks of palpitations that are not recorded during daily monitoring of the electrocardiogram;
- episodes of rare pulse followed by attacks of palpitations;
- constant low pulse;
- fainting and dizziness, especially in young people;
- WPW syndrome;
- study of various characteristics of supraventricular paroxysmal rhythm disturbances with an established diagnosis;
- assessment of the effectiveness of antiarrhythmic treatment, including surgery;
- in some cases - diagnosis of coronary heart disease.
Carrying out EPI of the heart
Due to the fact that the essence of electrical stimulation of the myocardium is the same for all three methods, and TPEPI is similar in technique to FEGDS, it makes sense to dwell in more detail on invasive EPI methods.
So, invasive endoEPI
is carried out in the department of x-ray and surgical diagnostic methods, while the patient is undergoing inpatient treatment in the cardiology, cardioarrhythmology or cardiac surgery department.
After a little preparation in the form of intravenous administration of sedatives, the patient is transported on a recumbent gurney to the X-ray surgery. The doctor conducting the examination, under conditions of complete sterility, accesses the femoral (less often the subclavian) vein under local anesthesia. A small incision is made in the vein in the most favorable place for the technique (called venesection).
Next, through the resulting incision, a thin plastic or metal conductor called an introducer is inserted into the patient's vein. A probe with electrodes at the end, which has X-ray contrast properties and is therefore visible on the screen, is passed along it. After the probe gradually moves through the vein to the right atrium, controlled on the screen, and the probe reaches the chamber of the heart (atrium or ventricle) necessary for examination, the myocardium is stimulated in a physiological mode.
The probe typically has three to five miniature electrodes that are connected to a device that can switch their operation from stimulation mode to recording mode, and vice versa. The resulting cardiograms are recorded using a computer device.
example of electrode placement for EndoEPI
The duration of the procedure is half an hour or more, without causing significant pain. The patient remains conscious throughout the operation. After removing the probe, a pressure aseptic bandage will be applied to the skin in the venesection area.
EpiEPI
carried out in the department of cardiac surgery. After putting the patient into a medicated sleep (general anesthesia), the chest is dissected with access to the pericardial cavity. The issue of using a heart-lung machine (ACB) is decided strictly individually. After exposing the inner layer of the outer layer of the heart (epicardium), electrodes are applied to it, and stimulation begins with simultaneous recording of the response received from the heart muscle. The study takes more than an hour. After all the necessary manipulations have been carried out, the wound is sutured layer by layer, and drainage remains in the pleural cavity and is removed on the 2-3rd day.
After any of the invasive EPI methods, the patient remains under observation in the intensive care unit for a period of one day or more, depending on the severity of the patient’s condition.
Preliminary procedures
The need to use EPI in the diagnosis of various cardiac disorders depends not only on their type, but also on the possible consequences. For many arrhythmias, an urgent visit to a cardiac surgery hospital is necessary, since conservative treatment in these cases is ineffective and even dangerous.
Before invasive diagnostic examination techniques, various non-invasive tests are required to obtain a more or less accurate picture. EPI is possible only after completing the following diagnostic plan:
| Diagnostic procedure | Purpose of the study |
| History, physical examination | Detection of cardiac pathology and its differentiation from neurological abnormalities. Determination of factors contributing to the occurrence of arrhythmias |
| Nervous system research | |
| EEG | Exclusion of abnormal phenomena in the central nervous system |
| CT/MRI | Detection of neoplasms and other abnormalities in the structure |
| ECG 12 leads | Determination of scar formations in the myocardium, conduction disorders inside the ventricles, hyperexcitation syndromes |
| Carotid Dopplerography | Detection of cerebrovascular insufficiency |
| Orthostatic test | Diagnosis of fainting conditions |
| Daily monitoring (Holter) | Determination of abnormalities that cannot be detected using a standard electrocardiographic study |
| Stress test | Detection of ischemia |
| EchoCG | Detection of intracardiac pathologies, organ size and contractility |
Are there any complications?
As with any invasive research method, complications of endo- and epi-EPI are possible, but they occur in extremely rare cases. The main types of adverse consequences are cardiac acute conditions provoked by artificially created tachycardia. These include:
- Angina attack
- Development of acute myocardial infarction,
- Thromboembolic complications caused by the entry of a blood clot that has broken away from the heart cavity, if the latter was not identified before the procedure using echocardiography (ultrasound of the heart).
Prevention of this kind of complications is a thorough examination of the patient before surgery, as well as competent determination of indications for examination.
In the postoperative period, there is an extremely low probability of developing inflammatory and thromboembolic complications, as well as the occurrence of life-threatening arrhythmias.
Preparation for the event
The procedure has specific features; preparation for it begins 7-10 days in advance :
- discontinue medications for the treatment of arrhythmia or reduce their dose in consultation with the cardiologist;
- during angina attacks, only Nitroglycerin is left for sublingual use;
- before TEE they undergo ECG, EchoCG, Holter monitoring and measure blood pressure several times a day;
- give up smoking and alcohol at least a week in advance;
- Dinner should be very light, and on the morning of the examination you should neither eat nor drink.
Decoding the results
Interpretation of the results is carried out by the doctor performing the study and the attending physician who referred the patient for the procedure.
Normally, the electrogram obtained during EPI reveals sinus tachycardia with a heart rate of 100 to 120 per minute or more. Such tachycardia is transient and is not dangerous for the patient.
example of EFI results
If the study protocol contains the phrase that no rhythm disturbances were achieved using all types of stimulation, it means that the patient does not have a suspected type of arrhythmia, and the EPS results are regarded as normal. Also, normally there should be no depression or elevation of the ST segment and negative T waves, indicating myocardial ischemia.
If such changes are detected, their location is indicated, as well as the type of electrical stimulation in which they occurred.
When an arrhythmia is detected, its type is indicated (atrial fibrillation, ventricular tachycardia, frequent ventricular extrasystole, etc.), and the stimulation parameters that caused the rhythm disturbance.
Any of the disorders recorded on the electrogram requires careful medical supervision due to the need to prescribe certain antiarrhythmic drugs or perform RFA.
Carrying out, based on the results of EFI, RFA – “cauterization” of the area of pathological electrical activity of the heart
What it is?
TEE is a functional diagnostic method used to determine the state of the cardiac conduction system. It allows you to determine whether this system is working normally, and also helps in diagnosing its violations. TEE identifies arrhythmias and helps clarify their characteristics necessary for proper treatment. Thus, TEE is a method for non-invasive diagnosis of heart rhythm disorders.
Approximate cost of EFI
Cardiac EPI can be performed in any large medical institution that has the appropriate personnel and technical equipment. Typically, EFI is carried out in regional or district centers, as well as in city hospitals in large cities (Moscow, St. Petersburg, Tyumen, Chelyabinsk, etc.).
Typically, EPI of the heart is carried out according to a quota from the Ministry of Health using funds from the federal budget. However, if the patient can pay for the procedure on his own, then there is no need to wait several weeks, since EFI can be performed for paid services.
Prices for cardiac electrophysiology testing vary widely. Thus, the cost of PPE is from 2000 to 4000 rubles, depending on the institution and equipment. The cost of endoEPI is much higher and amounts to 60-180 thousand rubles, depending on the payment for the probe and catheters, as well as the payment for the subsequent stay in the clinic.
Contraindications
- Patient refusal or severe neurotic reaction to electrode insertion;
- diseases of the esophagus (tumor, narrowing, esophagitis in the acute stage, esophageal polyps);
- acute diseases, including fever;
- difficulty in nasal breathing;
- atrial fibrillation at the time of the test (atrial fibrillation);
- atrioventricular block II and III degrees (diagnosed using electrocardiography);
- thrombus in the heart cavity (detected by ultrasound examination of the heart).