Most often, sudden cardiac death occurs outside a medical institution, with 80% of cases occurring in public and work places where there is no possibility of providing emergency resuscitation care [1, 2].
The probability of survival in patients with ventricular fibrillation, according to modern literature, decreases by 7–10% in each subsequent minute. Primary resuscitation measures (ABC) cannot convert fibrillation into hemodynamically effective heart contractions in such patients without electrical pulse therapy (EPT). Therefore, early defibrillation in such situations is a chance to restore an effective heart rhythm, i.e. save the patient's life.
In recent years, there has been increasing support among experts for the concept of early defibrillation using an automatic external defibrillator (AED). This concept implies the presence of AEDs in public places (airports, supermarkets, educational institutions, etc.), which will allow even an unqualified eyewitness to help a patient with sudden cardiac arrest before the arrival of an emergency medical team (EMS).
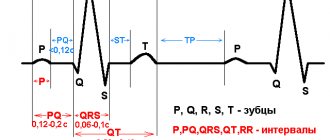
I would like to remind the reader that electropulse therapy is a procedure for stopping cardiac arrhythmias (arrhythmias) by exposing the myocardium to an electrical discharge. There are two types of EIT: defibrillation and synchronized electrical cardioversion (ECV). These two types of EIT differ significantly in the mechanism for applying an electric discharge.
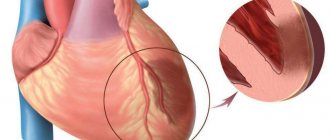
Defibrillation is the application of a pulse of direct electrical current with sufficient energy to depolarize the myocardium, which allows the first order pacemaker to resume control of the heart rhythm. Defibrillation is one of the integral components of resuscitation measures and should be carried out, if necessary, by nursing staff.
Electrocardioversion is the effect of a direct electric current pulse on the myocardium, synchronized with the least vulnerable phase of the electrical systole of the ventricles. Electrocardioversion can be planned - restoring the rhythm with stable hemodynamics, when preparing the patient for the procedure, and emergency - performed for various tachyarrhythmias with unstable hemodynamics.
Defibrillators-cardioverters
A defibrillator is a device that generates a single charge of direct electrical current that can be passed through the myocardium to eliminate ventricular fibrillation.
An automatic external defibrillator is a device that generates a single charge of direct electrical current and is used to conduct an electrical impulse through the chest wall to the heart. The AED is a computer that evaluates the patient's heart rhythm and decides whether EIT is necessary. Specificity in recognizing the rhythm subject to EIT approaches 100%. Currently, AEDs guide unskilled rescuers through the entire resuscitation process, from assessing the patient's viability to performing CPR. The AED operation protocol includes a sequence of visual and voice prompts that are aimed at helping the rescuer during resuscitation, and also has a function for recording the course of events, which allows you to subsequently retrospectively analyze the use of the device. The effectiveness of AEDs has been proven and recommended for use by the ERC (2010) [4].
An implantable defibrillator cardioverter ( IDC) is The IDK constantly monitors the patient’s heart rhythm and, when life-threatening arrhythmias are detected, stops them using differentiated electrical impulses. The choice of electrical impulse by the device depends on the type of rhythm disturbance. Heart rate analysis and therapy takes seconds for the IDC. The effectiveness of the device has been confirmed by SMASHVT studies [5] in the USA and Europe. IDC can significantly prolong the life of patients with episodes of hemodynamically ineffective rhythms. The need to replace the device every 5–8 years (Gem III VR, Maximo VR).
Cardioverter is a complex of a defibrillator and an electronic synchronizer device, which makes it possible to deliver a discharge at a certain phase of the electrical systole of the ventricles (usually 20–30 ms after the apex of the R wave). When eliminating tachyarrhythmia, there is a danger of applying an electrical pulse in the most vulnerable phase of cardiac activity (the period of repolarization of the ventricles of the heart on the ECG corresponds to the apex of the P wave), which can cause ventricular fibrillation (VF). To prevent VF in the treatment of tachyarrhythmia, a cardioverter is used.
Recommendations on the form and energy of the electrical shock for defibrillation are set out in the ERC (2005).
Types of physiotherapy with pulsed current
The physiotherapeutic procedure itself, associated with the influence of pulsed current, is an effect alternating with rest phases. The amplitude and rhythm of the current gradually increase, reach a high point, and then smoothly decrease to zero.
The current pulse is supplied through electrodes that are placed at certain points on the patient's body. The impact of the current is calculated so that the doctor can visually observe muscle contraction. In this case, the impact should not cause any discomfort. The current strength is usually 10-15 mA, the procedure lasts 15 or 30 minutes. As a rule, 15-20 such procedures are prescribed.
Pulsed currents are used in various types of physiotherapy. These include:
- Electrosleep;
- Diadynamic therapy;
- Interference;
- Amplipulse therapy;
- Electrical stimulation;
- Fluctuarization.
During electrical sleep, portions of low-intensity current pulses affect the brain receptors, normalizing the functions of the central nervous system. In this case, the pulse frequency varies from 1 to 150 Hz, and the duration is 0.2-0.3 ms. Bifurcated electrodes are applied to the patient's eyes and mastoid process.
To conduct diadynamic therapy, low-frequency pulses of 50-100 Hz are used. The impact can be separate or alternate between long and short periods. The epidermis resists this action, resulting in hyperemia, the walls of blood vessels dilate, and blood flow increases. The therapeutic effect of the procedure is associated with stimulation of the nervous system and muscle tissue.
Diadynamic therapy activates the circulatory system, metabolic processes are enhanced, and pain is noticeably reduced. This method is often used to treat pathologies of the musculoskeletal system and the peripheral nervous system.
Interference is the effect of low-frequency pulsed currents of 1-150 Hz of constant or variable frequency. The technique is used in the treatment of pathologies of the peripheral nervous system at subacute stages.
Amplipulse therapy is carried out with simulated sinusoidal currents of low frequency 10-150 Hz; mid-frequency currents of 2000-5000 Hz are also used. The current penetrates the skin, does not cause irritation, but has an exciting effect on muscle and nerve fibers. This type of physiotherapy is prescribed for problems with the musculoskeletal system, injuries, pathologies of the nervous system and other diseases.
Electrical stimulation is used to excite or significantly enhance the functioning of organs and systems. The most common options are stimulation of motor muscles, nervous system and cardiac activity. This type of impact helps maintain the vital activity and nutrition of muscle tissue, prevent its atrophy and strengthen it during rehabilitation or recovery after forced inactivity.
Fluctuarization is exposure to alternating currents of low frequency 10-2000 Hz, fully or partially rectified. They irritate and excite tissues, increasing the flow of lymph and blood.
Indications for electropulse therapy
At the prehospital stage, indications for EIT include cardiopulmonary resuscitation (CPR), unstable hemodynamics, increasing symptoms of acute left ventricular failure, syncope, severe anginal attack with various types of supraventricular and ventricular tachyarrhythmias (atrial flutter or fibrillation, paroxysmal supraventricular tachycardia, ventricular tachycardia) . In emergency situations, the main indication for EIT is the picture of unstable hemodynamics or CPR.
Effect of physiotherapy
Physiotherapeutic procedures have a normalizing effect on metabolism, redox processes, regulation of internal organs, lymph and blood circulation. In addition, they mobilize the body's defenses.
Physiotherapy is part of the comprehensive treatment of diseases. As a rule, its methods are used at the stage of remission, but can also be used in the acute stage. The main advantage of this direction is the absence of exposure to drugs and chemicals. Thus, the high effectiveness of physiotherapy is combined with the safety of its use.
Success of EIT
The effectiveness of EIT largely depends on the transthoracic impedance (transthoracic resistance). Typically, 10–20% of the discharge energy passes through the heart; an increase in transthoracic impedance leads to a decrease in the current reaching the myocardium, which impairs the effectiveness of EIT. Transthoracic resistance is influenced by chest size and hair cover; size and location of the electrodes, the force of their pressing to the chest; conductive material between the electrodes and the patient’s skin; number of shocks applied; previous surgical interventions on the chest by the patient and a number of other factors. Modern cardioverters have the option of automatic compensation of transthoracic impedance, which allows a discharge close to the optimal one to be passed through the heart.
You should lubricate the defibrillator electrodes with a special conductive gel or use special disposable electrodes, this will reduce the resistance between the electrodes and the patient's skin.
The electrodes must be pressed tightly against the patient’s body with a force of 10 kg, since even a small layer of air between them and the skin is a good insulator, and this will lead to burns.
The discharge must be applied during the exhalation phase; the lungs filled with air increase the resistance of the chest tissues.
EIT in “wet” patients is ineffective, since water on the chest dissipates the charge over the surface and the current discharge will spread in the superficial tissues and, therefore, will not reach the myocardium.
Indications for using pulsed current
In the treatment of various types of pathologies, doctors use pulsed current. The impact is carried out in a rhythm specified by a special device, which corresponds to the rhythm of the functioning of the internal system or a specific organ. The pulse frequency may also change.
Pulsed currents in physiotherapy are used to treat the following diseases and pathological manifestations:
- Lesions of the neuromuscular system;
- Diabetes;
- Painful sensations of various origins;
- Obesity;
- Hyperthyroidism;
- Pathologies in the endocrine system;
- Impaired intestinal motility;
- Diseases of the genitourinary system and pelvic organs;
- Skin problems of a cosmetic nature.
Indications for the use of pulsed current may include injuries and diseases of soft tissues: bruises, myositis, sprained muscles and ligaments. This technique is used for damage to the spine and joints, as well as peripheral nerves as a result of disease or injury. The effect of current helps to cope with rhinitis, otitis, sinusitis, remove stones from the ureter, and cure lymphatic edema of the lower extremities.
In dentistry, fluctuating currents are used to treat neuralgia of the glossopharyngeal, trigeminal and other nerves, alveolitis, periodontal disease, arthritis of the temporomandibular joint, inflammatory and purulent processes in the submandibular and maxillofacial areas, including after surgery.
Rational implementation of electropulse therapy
— Before performing EIT, all patients with preserved consciousness must be provided with complete pain relief. Inhalations are carried out with 100% humidified oxygen. As a premedication, 0.1 mg of fentanyl is prescribed, and for elderly or weakened patients, 10–20 mg of promedol.
— Medicinal sleep is carried out with the help of sibazon (Seduxen, Relanium), 5 mg of which is administered intravenously in a slow stream, and then 2 mg is added every 1–2 minutes to medicinal sleep. It is advisable to use intravenous anesthesia with propofol 2–2.5 mg/kg. In exceptional cases, in the absence of these drugs, the use of ketamine (0.5–1 mg/kg) is acceptable.
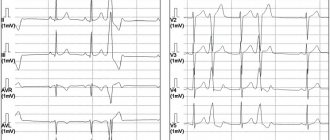
— Before and after EIT, an ECG is recorded in leads that are informative for rhythm analysis (II, V1, according to Lian).
— The required discharge energy to stop the rhythm disturbance is selected depending on the type of arrhythmia: for supraventricular tachycardia and atrial flutter - 50 J, for atrial fibrillation - 75 J, for ventricular tachycardia - 100 J, for the diagnosis of polymorphic ventricular tachycardia or ventricular fibrillation - 200 J .
— If EIT is ineffective, repeat after administration of an antiarrhythmic drug indicated for this arrhythmia.
— After EIT, the heart rhythm is assessed. If the arrhythmia continues, a second shock is given at a higher energy level; if ventricular fibrillation is detected, then defibrillation is performed; if sinus rhythm is recorded, then an ECG is recorded and the patient is hospitalized in a hospital.
Indications for hospitalization
All patients who experienced clinical death in the prehospital stage should be urgently hospitalized after hemodynamic stabilization. Hospitalization should be carried out with reliable venous access, with the obligatory possibility of performing EIT during transportation. Patients who have experienced clinical death are transferred “hand to hand” to the resuscitator on duty.
Safety precautions
Persons who have studied the safety rules when working with electronic medical devices are allowed to work with a defibrillator-cardioverter. Remember, a defibrillator is a device of increased, and sometimes fatal, danger! During EIT, it is important not only to help the patient, but also to protect yourself and others. The discharge of the released electrical energy can cause fatal rhythm disturbances in the rescuer or in the person who inadvertently touched the patient.
Necessary:
- remove all strangers (neighbors, relatives, etc.) from the premises;
- wipe the patient’s chest dry;
— remove oxygen from the defibrillation zone.
Prohibited:
— Hold both electrodes of the device in one hand!
— Charge the defibrillator if the electrodes are not placed on the patient’s chest!
— Direct or indirect contact with the patient during EIT!
How to use a defibrillator
1. Turn on the defibrillator.
2. Apply a sufficient amount of conductive gel to the electrodes. If there is not enough gel under the electrodes, burns will occur.
3. Select the required energy level.
4. Install electrodes: one - under the right clavicle marked Sternum, the second - above the area of absolute cardiac dullness marked Apex; with force (10 kg) press the electrodes to the patient’s chest.
5. Give the command “Get energy!”
6. Avoid touching the patient while the shock is being applied.
7. Give a loud command “Discharge!” Perform a discharge by simultaneously pressing both trigger buttons on the electrodes.
8. Check the result of the EIT. Register an ECG.
9. If necessary, resolve the issue of repeated discharge.
Complications of cardioversion include: ventricular fibrillation; aspiration of gastric contents; laryngospasm; hypoventilation; skin burns; electric shock to medical personnel.
Selecting a device for EIT
A wide range and price differences make choosing a device for EIT a difficult task. First of all, you need to decide who will use this device: a paramedic, an emergency rescue worker or a doctor. An AED is a necessary tool for performing high-quality CPR, which does not require extensive personnel training. The price is determined by the quality of electronic components and batteries. Professional cardioverter defibrillators are multifunctional devices that are equipped with an ECG monitor, a built-in thermal printer, an external pacemaker module, and a pulse oximeter for determining SpO2 saturation.
It is necessary to clarify the availability of children's electrodes. Remember that modern devices for EIT generate a biphasic pulse shape, and monophasic defibrillators have not been produced since 2005.
There are no contraindications to the use of emergency cardioversion in a critically ill patient.
Contraindications and effects
It is important to remember that there are certain contraindications for the use of physiotherapy methods using pulsed currents:
- Tumors of various etiologies;
- Individual intolerance to exposure;
- Pregnancy (second trimester);
- Hemarthrosis in the acute stage;
- Kidney and cholelithiasis;
- Spastic state of muscles;
- Dislocations, bone fractures;
- Bleeding.
Current pulses have an exciting, stimulating and irritating effect on the human body. Passing through the tissues of the body, the current causes increased functions of cell membranes and tissue tension. Cells are activated, their vital activity improves, the functioning of joints, blood vessels and nerve fibers is restored. This helps speed up the treatment of many diseases, as well as avoid all sorts of complications.
In general, as a result of exposure to pulsed currents, the following occurs:
- Reducing congestion in the pelvis;
- Metabolism improves, the body's defenses increase;
- The synthesis of organ secretion is activated;
- The permeability of cell membranes increases.
Physiotherapeutic procedures using pulsed current activate blood flow, so the drugs used penetrate the tissues faster, and the effectiveness of treatment increases.