Deep vein thrombosis, along with thrombophlebitis of the saphenous veins and thromboembolism of the pulmonary arteries, are combined into a single concept - venous thromboembolic complications (VTEC).
Venous thrombosis is an acute disease characterized by the formation of a blood clot in the lumen of a vein with a more or less pronounced inflammatory process and disruption of blood flow. The presence of an inflammatory component in the area of thrombosis determines another name for this disease - thrombophlebitis.
Most phlebologists, understanding the conventions of such a division of venous thrombosis, use the term “thrombophlebitis” to denote damage to the saphenous veins (in which symptoms of inflammation are pronounced), and the terms “thrombosis”, “deep vein thrombosis”, “phlebothrombosis” to denote damage to the deep veins .
Deep vein thrombosis (DVT) is a disease that negatively affects not only the venous and lymphatic return system, but also worsens the function of the cardiovascular system as a whole.
If you do not take active steps to eliminate this pathology, the further course of the pathological process becomes persistent, prone to self-development and irreversible.
The disease does not have strictly characteristic symptoms and has many risk factors and triggering factors, which requires the additional use of additional high-precision modern instrumental diagnostic tools to clarify its presence and type of course, the main of which in modern clinical conditions is the method of ultrasound angioscanning with color mapping.
- According to the International Consensus Statement, the incidence of deep vein thrombosis in the general population is approximately 160 cases per 100,000 population, with the incidence of fatal pulmonary embolism being 60 per 100,000 population.
- In Russia, venous thrombosis affects 240,000 people annually, and pulmonary embolism, including fatal ones, develops in 100,000 of them, which significantly exceeds the incidence rates of tuberculosis, viral hepatitis, and HIV infection.
- In the United States, approximately 200,000 people are hospitalized each year for deep vein thrombosis. In this case, 1/3 is accounted for by repeated thromboses. Among Italian residents of the most active working age (from 20 to 55 years), deep vein thrombosis is diagnosed within 1%.
- Venous thrombosis occurs in a wide variety of clinical situations and complicates the course of many diseases. The incidence of postoperative thrombosis, according to various authors, is 20-59%.
What it is?
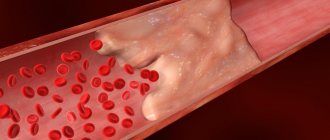
Thrombosis
is a pathological condition in which dense blood clots (thrombi) form in the vessels, slowing down or completely stopping the normal flow of blood. As a result, a lack of organ nutrition (ischemia) may occur, which in turn can lead to tissue death (necrosis, infarction) and death. There are two types of thrombosis: venous and arterial. From the names it is clear where the formation of blood clots occurs. In the first case - in the veins, in the second - in the arteries. The disease can occur in acute and chronic form. Arterial thrombosis is the most dangerous.
Main causes
There are three main factors for thrombus formation.
- Damage to the vessel wall
(as a result of injury, surgery and poor nutrition (cholesterol plaques form), infection, heavy lifting, childbirth, etc.). - Blood clotting disorder
(tendency to increased clotting). Changes in blood clotting may occur due to metabolic disorders or hormonal imbalances. - Stagnation of blood
. It occurs when a person remains motionless for a long time in one position (for example, in front of a computer, in an airplane seat, or chained to a bed).
The risk group also includes people with varicose veins, those who are overweight, bad habits, leading a passive lifestyle, as well as people over 60 years of age.
Symptoms of thrombosis
The following signs are characteristic of arterial thrombosis:
- Sharp pain that occurs in one place and spreads to adjacent areas in the form of a pulsating stream
- A feeling of numbness in the extremities depending on the location of the blood clot, causing them to lose sensation and become cold
- Shortness of breath, irregular heart rhythm, chest tightness (due to blockage of the pulmonary artery)
- Dizziness, speech disorder (due to blockage of cerebral arteries)
With venous thrombosis the following is observed:
- Increasing pain in the affected area
- Swelling and hardening of the veins at the location of the blood clot
- The skin color in this area takes on a blue tint.
- Swelling and bulging of superficial veins.
Acute arterial insufficiency
The main sources of peripheral arterial embolism are currently considered to be heart disease (95% of all cases). Moreover, more than half of them are due to atherosclerotic cardiopathy: myocardial infarction, post-infarction cardiosclerosis, cardiac aneurysms. Acquired heart disease accounts for 40-43% and congenital defects 1-2%. In atherosclerotic cardiopathy, the thrombus is usually localized in the left ventricle, and in case of heart defects in the left atrium or its appendage. Of the non-cardiac sources of embolism, the first place is occupied by aortic aneurysm (34%), followed by aneurysm of the subclavian artery, thrombosis of the veins of the systemic circulation (with cardiac septal defects), pneumonia, and lung tumors. In approximately 8% of patients with embolism, its source remains unknown. Most patients with embolism experience various heart rhythm disturbances, often in the form of atrial fibrillation, which contribute to intracardiac thrombus formation. In most cases, emboli are localized in the area of arterial bifurcation. Based on pathological and clinical studies, it was found that the visceral branches of the abdominal aorta are most often affected (up to 40% of all embolisms), then the arteries of the brain (from 35 to 60% according to different authors) and only after them the aorta and arteries of the lower extremities ( 25%). The frequency of embolism in various segments of the arteries of the lower extremities is as follows: aortic bifurcation 10%, iliac artery bifurcation 15%, femoral artery bifurcation 43%, popliteal artery 15%. In approximately 1/4 of patients, repeated embolisms are observed; multiple embolisms are not uncommon, when the embolus clogs one of the main arteries of the limb and a visceral artery. This type (called “combined”) embolism presents diagnostic difficulties (embolism in the abdominal vessels may be missed or diagnosed late). Finally, mention should be made of “level” emboli, in which the emboli are located at different levels in the main artery: for example, in the femoral and popliteal. Following arterial embolism, acute ischemia of the limb or organ supplied by this vascular system develops. Its severity will depend on a number of factors:
- severity of roundabout circulation,
- continued thrombosis,
- arterial spasm,
- state of central hemodynamics.
Lack of oxygen leads to disruption of tissue metabolism. The accumulation of under-oxidized metabolic products (lactate, pyruvate) leads to local acidosis. The permeability of cell membranes is disrupted, muscle cells die, as a result, electron exchange suffers, expressed in increased transport of K+ ions into the extracellular space and then its increased concentration in the blood plasma; accumulation of myoglobin, which is filtered by the kidneys and can accumulate in the tubules, blocking them. A drop in intravascular pressure to a stagnation level leads to platelet aggregation and the formation of blood clots in the microcirculation system. As a result, irreversible changes in tissues occur. Later, thrombosis develops in larger arteries. Different tissues vary in their tolerance to ischemia. So in the tissues of the extremities, irreversible changes with complete ischemia occur after 6-8 hours, in the intestines after 2 hours, in the kidneys 40-50 minutes, in the brain after a few minutes.
Clinical course and symptoms of peripheral artery embolism
The main symptom of arterial embolism is pain in the affected limb. It occurs suddenly and is very strong. Sometimes patients fall, unable to withstand this severe pain. Along with pain, patients often note a feeling of numbness in the limb. Upon examination, a change in the color of the skin of the limb is striking: from pronounced pallor to a “marble” color. In the late stage of ischemia, when thrombosis of the venous bed occurs, the color of the skin becomes cyanotic. With comparative palpation, the difference in skin temperature is noticeable, especially in the distal parts of the limb. There is also a disorder of all types of sensitivity (pain, tactile, deep). The border of sensitivity disorder does not coincide with the level of arterial occlusion, but is lower, which should not mislead the diagnostician. An equally characteristic symptom is a violation of active movements in the joints of the limb, which vary in degree from limitation to complete plegia. In the late stage of severe ischemia, passive movements may also be absent due to rigidity of muscles and joints. Joint contracture is an unfavorable sign indicating the non-viability of the limb. The absence of a pulse in the arteries located distal to the level of blockage is also one of the important symptoms of embolism. With severe swelling of the limb, it is sometimes difficult to determine the pulse. Slow filling of the saphenous veins, or the “groove” symptom, also indicates poor circulation. Sometimes there is increased pulsation in the arteries located proximal to the occlusion, determined by comparative palpation. In advanced cases, severe muscle soreness on palpation, rigidity and subfascial edema are observed. Various classifications have been proposed to assess the severity of limb ischemia. The classification proposed by V.S. Savelyev and co-authors in 1978 most fully meets practical purposes. Classification of acute arterial insufficiency (V. S. Savelyev)
- Stage I of ischemia is the stage of functional impairment (sensitivity and movements of the limb are preserved, acute pain in the limb, pallor and coldness of the skin, absence of pulse in the peripheral arteries).
- Stage I A - a feeling of coldness, numbness, paresthesia.
- Stage I B - pain in the distal parts of the limb occurs.
- Stage II of ischemia is the stage of organic changes. Its duration is 12-24 hours. There is no pain and tactile sensitivity, active and passive movements in the joints are limited, muscle contracture develops, and the skin is bluish.
- Stage II A - disorders of sensitivity and movement - paresis.
- Stage II B - disorders of sensitivity and movement - plegia.
- Stage II B - subfascial edema.
- Stage III of ischemia is necrotic. The duration of the stage is 24-48 hours. All types of sensitivity and movements are lost. As a result, gangrene of the limb develops.
- Stage III A - partial muscle contracture.
- Stage III B - total muscle contracture.
The diagnosis of great artery embolism is usually made on the basis of physical findings. Additional research methods include ultrasound, radioisotope and X-ray contrast angiography. In this case, the main purpose of their use is to establish the patency of arteries located distal to the occlusion. It should be noted that due to spasm of both main and collateral vessels, the information content of these methods is sharply reduced.
Arterial thrombosis
Differential diagnosis: may be required in patients with arterial thrombosis, which will be discussed in more detail in the section on thrombosis.
In case of incomplete ischemic syndrome (1st stage of ischemia), embolism must be differentiated from spinal diseases (intervertebral disc herniation, acute ischioradiculitis (lumbago), soft tissue diseases (myositis, tendonitis). With all of the listed diseases, the arteries of the foot remain and this is the main distinguishing feature. Differential diagnostic difficulties may arise between embolism with severe ischemia and blue phlegmosia (Gregoire's disease). Blue phlegmosis is distinguished by the following symptoms: thrombophlebitis without anamnesis (often does not occur), sharp, rapidly increasing swelling of the entire limb, sometimes spreading to the lower abdomen, sometimes hemorrhagic epidermal blisters, severe endotoxicosis. Treatment at the prehospital stage
District or emergency doctors should know that the success of preserving the limb and life of patients with embolism of the main arteries directly depends on the timing of delivery to the hospital and restoration of blood circulation. Conservative treatment on an outpatient basis with the hope of resorption of the embolus is unacceptable, but it should begin immediately after diagnosis. Avoid any local warming or cooling agents (compresses, ice, etc.). The limb remains at rest; during transportation, splinting with a soft lining is necessary. Pain relief is achieved by administering drugs or analgesics. An important point is the administration of anticoagulants (10 thousand units of heparin) to prevent continued thrombosis. If necessary, cardiotonic drugs are prescribed. The issue of prescribing vasodilators is controversial, since they act not only on collaterals, but also on the post-occlusion segment of the artery, slowing down the already slow blood flow in it. Under certain conditions, this can lead to deterioration of microcirculation and more rapid progression of ischemia.
The main method of treatment for embolism of the aorta and peripheral arteries should be surgical, aimed at restoring blood flow in all patients who do not have absolute contraindications to surgery.
The latter include: 1. agonal state of the patient, 2. gangrene of the limb. Relative contraindications are: 1. tension ischemia or grade 1 in elderly patients (70-80 years old) with severe concomitant diseases, 2. with embolism of the end parts of the upper or lower limb, 3. with embolism of the upper limb with relative circulatory compensation and severe general condition. Surgical treatment
The operation of choice is embolectomy.
The best results are obtained in the early stages (6-8 hours) after the development of embolism. This is explained by the duration of tissue tolerance to ischemia, which for the limbs is within these limits. At later stages, irreversible tissue changes may develop. However, the timing itself does not determine the indications for surgery. A reliable guideline is the severity of limb ischemia, which depends on several factors: 1. level of occlusion, 2. size of the continuous thrombus, 3. state of preformed collaterals, 4. central hemodynamics. Thus, embolectomy can be successfully performed even after several days, if the limb is still viable. Tactically, emergency surgery is required (within 12 hours from the moment the patient is admitted) for grade 2-3 ischemia. In case of embolism occurring with grade 1 ischemia, surgery can be delayed for 1 or several days. In most cases, the operation can be performed under local anesthesia, but with the obligatory presence of an anesthesiologist. During the operation, it maintains central hemodynamics, acid-base status, respiratory function, etc. Operational technique
It was significantly simplified after the introduction of Fogarty balloon catheters into practice (1962).
Embolectomy of the aorta and iliac arteries
With aortic embolism, both femoral arteries in Scarp's triangle are exposed. The deep and superficial femoral arteries are isolated in their initial section and placed on rubber holders. The patient is heparinized (5-10 thousand units of heparin). The arteries are clamped and opened with a transverse incision along the anterior wall of the femoral artery above the bifurcation. By temporarily loosening the clamps, retrograde blood flow from the femoral arteries is checked; if it is satisfactory, the arteries are clamped again. A Fogarty catheter is inserted through the lumen of the iliac artery into the aorta, the balloon is inflated, and the embolus with a continuous thrombus is released. Sometimes it is necessary to repeat this manipulation to obtain good central blood flow. The femoral artery is clamped and a similar procedure is performed on the opposite side. Then the arterial bed is washed with heparinized Ringer's solution and the arteriotomies are sutured alternately with interrupted sutures.
Femoral artery embolectomy
Access to the artery is the same. The embolus is localized, as a rule, at the bifurcation of the femoral artery, but prolonged thrombi can spread a considerable distance downwards and upwards. After arteriotomy, the embolus is removed by extrusion. Then, thrombectomy is performed from the proximal and distal arterial beds. Difficulties in restoring blood flow arise in cases of thrombosis of the tibial arteries, into which it is not always possible to insert a catheter. In such cases, techniques such as circular compression of the leg muscles and suction of thrombotic masses through a polyethylene catheter inserted into the lumen of the tibial artery are used. Sometimes it is necessary to resort to retrograde washing out of the thrombus from the tibial (anterior or posterior) arteries. To do this, the posterior tibial artery is exposed on the foot, behind the medial malleolus. The latter is taken on holders, a transverse arteriotomy is made over half a circle, a polyethylene catheter of a suitable diameter is inserted into the lumen of the vessel, through which a heparinized solution is injected under pressure, which, together with thrombotic masses, is removed through an arteriotomy in the femoral or popliteal artery. Once the bed is free of thrombi, the arteriotomy is sutured with interrupted sutures.
Embolectomy from the popliteal artery
Surgical access to the popliteal artery is made from a tibiomedial incision. To do this, the skin with subcutaneous fat and fascia are dissected along the tibia, moving 2 cm downwards from it. The length of the incision is 8-10 cm. The tendons of the semitendinosus and semimembranosus muscles are cut. The gastrocnemius muscle is separated bluntly, and the soleus muscle is partially dissected, opening the tibioperoneal canal, after which the neurovascular bundle is exposed. In front lies the tibial nerve, which is retracted on a holder. The artery is separated from the accompanying veins and taken on a holder. In this case, the initial sections of the tibial arteries (trifurcation), where the embolus is most often localized, should be visible. A transverse arteriotomy is performed above the level of the origin of the anterior tibial artery and the embolus is removed by extrusion. The tibial arteries are then freed from the continued thrombus using Fogarty catheters of the appropriate diameter. The distal bed is washed with a heparinized solution and the arteriotomy is sutured. In severe ischemia accompanied by subfascial edema, embolectomy is complemented by fasciotomy. It is performed on the inner and outer surface of the lower leg. To do this, a small (2-3 cm) skin incision is made in the upper part of the leg, the own fascia of the leg is opened, after which a branch of long blunt scissors is inserted under the fascia and it is dissected under the skin along the entire length of the scissors. 1-2 sutures are placed on the skin.
Embolectomy from the arteries of the upper limb
To do this, it is advisable to expose the brachial artery in the ulnar pit and highlight the bifurcation in order to control the arteries of the forearm. A transverse arteriotomy of the brachial artery is performed above the bifurcation. A Fogarty catheter is inserted into it in the central direction and the embolus with thrombotic masses is removed. In the postoperative period, conservative therapy continues, aimed at improving hemostasis and blood rheology. To do this, continue to administer heparin up to 30-40 thousand units per day (5 thousand units every 4 hours), under the control of thromboplastin time. After 78 days, indirect anticoagulants are additionally prescribed, and heparin is gradually discontinued. To improve microcirculation, rheopolyglucin, rheomacrodex or reogluman are administered in 400-800 ml doses. intravenous drip. Trental is added to it 5.0 x 2 times. To improve the platelet component of hemostasis, small doses of aspirin of 100 mg are prescribed. h/w 2 days on the 3rd day.
Post-ischemic syndrome
In some patients (according to some data up to 30%), especially with severe ischemia, after restoration of blood flow in the limb, local and general disorders develop, known as “tourniquet syndrome”. All of them have many common features with the long-term compartment syndrome described by Bouters in the 50s. Local manifestations of post-ischemic syndrome are associated with the development of limb edema, which can be segmental or total. Edema of the limb is caused by increased cellular permeability and thrombosis of the venous bed. After the blood flow to the extremities is turned on, a large amount of under-oxidized metabolic products (lactate, pyruvate, etc.) enters the general bloodstream, which leads to the development of metabolic acidosis. Violation of the acid-base state negatively affects central hemodynamics, leading to hypotension, a decrease in stroke volume, etc. Against this background, concomitant hypercapnia and hyperkalemia can lead to cardiac arrhythmias, up to asystole. Metabolic and cardiac disorders lead to respiratory failure. The entry into the general bloodstream of myoglobin, which is formed in large quantities as a result of the death of muscle cells, leads to a blockade of the renal tubular system. Hypotension also contributes to the development of acute renal failure. Treatment Treatment of endogenous intoxication should be comprehensive and include regional perfusion of the limb and hemosorption. To carry out regional perfusion, a tourniquet is applied to the lower limb until arterial blood flow is completely stopped. The femoral artery is cannulated through the arteriotomy in the distal direction, and the femoral vein is cannulated through the mouth of the severed great saphenous vein. A perfusate consisting of 600 ml is poured into the heart-lung machine. 0.85% NaCl, 10 ml. 2% papaverine, 200 ml. 0.25% novocaine, 60000 units. fibrinolysin, 120,000 IU of streptase and 10 thousand units. heparin. After 30-40 minutes of perfusion, the perfusate with the patient’s blood is removed from the AIK until the limb turns pale. Then the device is filled with donor blood, sodium bicarbonate, heparin, novocaine, and perfusion of the limb is repeated for 10 minutes to oxygenate the tissues. After which the tourniquets are removed, the arteriotomies are sutured and the blood flow is turned on. A hemosorption session is carried out with various sorbents (SKN) at a rate of 8-120 ml/min and a duration of 30 to 120 minutes. Infusion therapy, antihypoxants (tocopherol), antiplatelet agents, and hyperbaric oxygenation are administered.
Acute arterial thrombosis
Acute arterial thrombosis extremely rarely develops in healthy arteries. In more than 90% of cases, it occurs in patients with chronic obliterating diseases of the arteries of atherosclerotic (mainly) or endangitic origin. More rare causes of thrombosis are the other two components of Virchow's triad: a violation of the blood coagulation system and a slowdown in blood flow. To varying degrees, they are present in patients with chronic obliterating lesions of the arteries. Men get sick more often than women. The peak incidence occurs in the 5th-6th decade of life. The symptoms of the disease are the same as for arterial embolism and depend on the severity of ischemia and the speed of its development. In general, it is believed that the development of ischemia during thrombosis is slower and not as pronounced as during embolism. However, a differential diagnosis cannot be based on these signs. A supporting sign may be previous chronic vascular disease and the absence of embologenic sources (heart disease, aneurysm, etc.). Of the additional examination methods, it is necessary, first of all, to point out anegiography, which makes it possible to establish the localization and extent of the thrombosed segment, and most importantly, the condition of the arteries located distal to the thrombosis. Angiograms show characteristic signs of chronic obliterating lesions of the arteries: segmental stenoses, corroded (uneven) artery contours, formed collaterals. In embolism, on the contrary, the occlusion border has a characteristic concave surface and ends abruptly, the overlying vessels have smooth walls, and the collaterals are poorly defined. Treatment Tactics of treatment of acute arterial insufficiency Degree of ischemia Disease embolism acute thrombosis / embolism? acute thrombosis? 1 emergency or delayed up to 24 hours embolectomy (for examination and stabilization of the general condition), anticoagulant or thrombolytic therapy, examination (angiography, ultrasound, ultrasound). depending on the dynamics of the disease and examination data, carry out conservative therapy, thrombolysis, revascularization surgery* 2a emergency surgery, anticoagulant or thrombolytic therapy, examination (angiography, ultrasound, ultrasound), thrombolysis, ROT, revascularization surgery in the first 24 hours* 2b emergency surgical treatment 2c emergency revascularization + fasciotomy + delayed amputation 3a emergency revascularization, necrectomy, delayed amputation 3b primary amputation * - Negative dynamics in the first hours of conservative treatment for 1st and 2nd degree of ischemia serves as an indication for emergency surgery. In acute thrombosis, urgent surgery is indicated only in cases accompanied by severe ischemia that threatens the viability of the limb. But even in these cases, all efforts should be directed at preliminary clarification of local operability (Dopplerography, angiography). In those patients whose limb ischemia is not severe after thrombosis, it is better to restore blood circulation in a delayed period. During this period, conservative therapy and a comprehensive examination of the patient are carried out. Many authors put forward the following arguments in favor of delayed surgery: 1) clarification of local operability (condition of the arteries), 2) development of collateral circulation, 3) improvement of the condition of soft tissues, 4) planned surgery is always preferable to emergency surgery (trained team of surgeons, plastic material, etc. .). Conservative treatment 1) heparin therapy from the first hours of admission at the rate of 30,000-40,000 units. per day every 4 hours under the control of a coagulogram, 2) Reopoliglucin 400-800 ml. IV drip, 3) trental 5.0 ml. x 2 times IV, 4) aspirin 100 mg. per day after 2 days, 5) nicotinic acid preparations intravenously and in tablets (nikoshpan, xanthinol nicothionate, halidor, etc.). In some cases, fibrinolytic therapy is used. In this case, thrombus lysis is possible in the early stages by endovascular administration of thrombolytic drugs to the thrombolytic segment or intravenous administration of thrombolytics. Thrombolytic drugs include strepto or urokinase, fibrinolysin, etc. All of them have serious side effects, so the program for such treatment must be clearly defined, and patients must be observed in the intensive care unit. Before starting treatment, the main parameters of the blood coagulation system are determined. Their normal indicators are as follows:
- recalcification time from 80 to 180 sec
- prothrombin complex from 70 to 100%
- fibrinogen from 200 to 600 mg%
- euglobulin fibrinolysis: more than 3 hours
After puncture and cannulation of the saphenous vein, the patient is administered 50 to 100 mg. prednisolone, after which the doctor administers an initial dose of 250,000 IU of streptase in 20 ml. physical Solution for 15 minutes. Then after 4 hours an additional 750,000 IU of streptokinase in 250 ml. saline solution (65 ml per hour), then every 8 hours streptokinase is administered twice in the same dose, after which the drug is administered daily for longer than 6 days (for a course of 3.5 million IU). Over the course of 3 days, additional heparin is administered at a dose of 30,000 units. per day. Constant laboratory monitoring of thrombin time is carried out, which should be 23 times higher than the initial one. Contraindications: patients under 60 years of age, recent injury, gastrointestinal ulcer, tumors, hypertension, infection (especially streptococcal), hypersensitivity to streptokinase, hay fever. Surgical treatment: in case of thrombosis, it cannot be limited to thrombectomy. Reconstructive operations such as bypass surgery, thromboendarterectomy, etc. are required. In the post-operative period, conservative therapy is carried out, as indicated above. Prevention of embolism: If an embolic lesion remains, then recurrence of embolism is very likely. The main task is to identify the sources of embolism and eliminate them (for heart defects, correction of valvular insufficiency, for aortic aneurysms, subclavian artery resection of the aneurysm).
Thrombosis and embolism of mesenteric vessels
Thrombosis and embolism of mesenteric vessels is one of the most dangerous diseases in urgent surgery, giving a very high mortality rate (up to 80%). Thrombosis and embolism of mesenteric vessels are relatively rare - 1 patient per 1500-2000 patients admitted to the hospital for urgent reasons. Thrombosis of mesenteric vessels occurs 5 times more often than embolism, and thrombosis can be in the form of thrombosis of arteries or veins, as well as combined thrombosis of arteries and veins. This disease is quite difficult. It is important to keep in mind that among the diseases against which thromboembolism of mesenteric vessels occurs, atherosclerosis is in first place in frequency, cancer is in second place, and heart defects, myocardial infarction, thrombovascular lesions of the liver and portal system are in third place. Embolisms and thromboses of mesenteric vessels are not a sad privilege of the elderly; middle-aged people often get sick. The variety of different types of intestinal circulatory disorders also determines the variety of clinical forms of thromboembolism of mesenteric vessels, therefore the diagnosis of thromboembolism of mesenteric vessels is of particular importance. Patient complaints and medical history Abdominal pain, vomiting, diarrhea, belching. In the anamnesis of these patients, it is possible to establish previous heart and vascular diseases associated with atherosclerosis (76.6%), thrombosis of the great vessels of the lower extremities (12%), heart defects (11%), hypertension (8%). Nature and localization of pain Pain due to thrombosis of mesenteric vessels, in the words of French authors, is called “Start at two tempos”. With thrombosis and embolism of thin branches, after blockage of the vessel, acute pain appears, which subsides. When thrombosis grows or a new embolus enters another vessel, the pain recurs again, but more intense and more widespread. The pain in these patients is localized throughout the abdomen (50%), in the remaining patients the localization is most uncertain. A number of patients before the disease experienced short-term abdominal pain with bloating that went away without a trace (gastric angina), which was quickly relieved by taking nitroglycerin. It is important that similar short-term abdominal pains were repeated and after some time passed, only to recur again after a certain period of time. Depending on the location of the occlusion, the location of pain changes. Pain in the epigastric region occurs when vascular obstruction is localized in the superior mesenteric artery, in the right iliac region - when a. ileocolica, in the lower quadrant of the abdomen - with damage to the inferior mesenteric artery. Sometimes the pain is cramping in nature. Dyspeptic disorders Vomiting occurs almost constantly. At first, the vomit consists of food debris, then it becomes fecal-like in nature and less often (10%) is blood-stained. Initially, there may be diarrhea, and in 20% of patients, stool mixed with blood is detected relatively early. With the development of peritonitis, it is possible to identify the clinical picture of acute peritonitis. Most authors distinguish two forms, occurring with symptoms of diarrhea or obstruction, although other forms are known (simulating acute appendicitis, perforation of intestinal ulcers). The tongue is usually dry, cracked, and coated. Temperature and pulse Initially normal, as destructive changes in the intestines develop and peritonitis progresses, the temperature acquires the character of purulent peritonitis. The pulse is weak, frequent, rarely slow; the pulse rate is influenced by the nature of the underlying cardiovascular disease and inflammatory changes in the abdominal cavity. Changes in the blood As a rule, already in the initial stages of the disease, leukocytosis is high, up to 30,000 and above with a shift of the formula to the left; in some patients there is hypochloremia. In the coagulation system there is hypercoagulation. Changes in urine When the superior mesenteric artery is blocked - glucosuria. Subsequently, as inflammatory changes in the peritoneum progress, changes characteristic of intoxication appear in the urine. Objective data
The condition is serious. Hypostasis is pronounced, especially in the abdominal area. In the initial stage of the disease, the abdomen is usually sunken and painful on palpation, but there is no rigidity of the abdominal wall muscles. When palpating the abdomen, a swelling of dough-like consistency is determined due to an infiltrated or blood-soaked loop of intestine. In these cases, it seems that there is an intra-abdominal infiltrate. Percussion, according to this “infiltrate”, dullness is determined, and in other parts - tympanitis. Peristalsis is not determined. There may be bloating, especially with venous thrombosis. X-ray examination Survey photographs of the abdominal cavity or fluoroscopic data give a picture of obstruction (Kloiber cups). Embolism and thrombosis of mesenteric vessels in their course resemble intestinal obstruction, pancreatic necrosis, myocardial infarction. For the purpose of differential diagnosis, laparocentesis with a groping catheter can be used,” and emergency laparoscopy is indicated. You should do an ECG and examine your urine for diastasis. Treatment of patients with thromboembolism of mesenteric vessels If the patient's condition allows, urgent laparotomy under endotracheal anesthesia is indicated. The extent of intervention depends on the severity of the lesion. In case of limited necrosis or subtotal damage, which is typical for arterial occlusion, intestinal resection within healthy tissue is indicated; in case of total necrosis, a trial laparotomy is indicated. In case of venous thrombosis with massive damage to the intestines, the introduction of anticoagulants and fibrinolytic agents (heparin, fibrinolysin, streptase, etc.) directly into the mesenteric veins is indicated, by catheterization of one of the veins with preliminary (if possible) thrombectomy. As a last resort, a catheter can be inserted into the root of the mesentery where anticoagulant agents are administered. Parenteral (in peripheral veins) anticoagulant and fibrinolytic therapy is also prescribed. In the early stages of the disease, before the development of total phlebothrombosis, this has a positive effect. Anticoagulant therapy should also be carried out for segmental lesions, due to arterial or venous thromboembolism, after resection of non-viable intestines. A catheter is inserted into the mesentery and through it heparin, 10-15-20 thousand units. (2-4 ml) in a 0.25% solution of novocaine 100-150 ml x 2 times simultaneously with antibiotics. In this case, not only the effect of novocaine blockade of the mesenteric nerve plexus is achieved, but also a longer and more effective effect of heparin, which, due to its lymphotropy, enters the lymphatic system. Such tactics, as our experience shows, are most effective for venous thrombosis; they can also be used after intestinal resection for any location of thromboocclusion, because helps restore microcirculation in the mesenteric basin, in the surgical area. Simultaneous lymphotropic administration of antibiotics prevents the development or progression of peritoneal infection. Intravenously, along with heparin, antiplatelet drugs (trental, reopolyglucin, hemodez, etc.) are prescribed. Heparin therapy under the control of the blood coagulation system (blood coagulation according to Lee White and prothrombin index). In case of an overdose of heparin and bleeding occurs, its inhibitor, protamine sulfate, is administered. Tasks of a general practitioner: • Drug prevention in patients at risk. • If abdominal pain occurs, the patient should be sent to a surgical hospital. • Warn the patient's relatives about the possibility of such complications and the need to urgently call a doctor in these cases.
Diagnosis of the disease
When visiting a medical facility, the doctor makes a diagnosis and prescribes treatment. Basic diagnostic methods:
- Blood tests for clotting
- Magnetic resonance venography
- Duplex/triplex scanning of the arteries of the lower extremities
- Duplex/triplex scanning of the veins of the lower extremities
- Duplex/triplex scanning of extracranial brachiocephalic arteries
- Duplex/triplex scanning of intracranial brachiocephalic arteries
- Duplex/triplex scanning of arteries and veins of the upper extremities
- Ascending venography using contrast agent
- Radionuclide scanning of thrombus location
- Thromboelastography.
Specialists to contact:
- Phlebologist
- Vascular surgeon
- Cardiologist
- Neurologist, etc.
Clinical picture
Common complaints:
- persistent or persistent increasing headaches;
- impaired sensitivity and motor skills of the muscles of the face, arms and legs, right or left half of the body;
- persistent distortion of speech and its understanding;
- blurred vision;
- loss of body balance, dizziness;
- feverish condition;
- excessive sweating;
- blood pressure surges;
- uncontrolled acts of defecation and urination;
- loss of consciousness;
- convulsive contractions, muscle twitching;
- nausea, vomiting.
Thrombosis of the basilar artery
Complaints regarding thrombosis of the basilar artery supplying the brain stem:
- throbbing occipital pain;
- dizziness, patients are “stormy, rocking on the waves”;
- blurry visual perception;
- impaired sensitivity of the skin around the mouth;
- gaze paresis – the inability to move both eyes simultaneously in vertical or horizontal directions;
- impaired sensitivity of half of the face;
- fainting;
- noise in ears.
Thrombosis of the carotid artery (internal, external)
Complaints characteristic of deterioration of blood supply to the brain through the internal carotid arteries :
- serious weakening of visual perception, even blindness;
- inability to speak, speech confusion;
- deterioration of motor function of the upper extremities;
- tremor;
- fainting;
- paresis of one or both halves of the body.
Complaints characteristic of deterioration of blood supply to the cerebral cortex, tissues of the neck and face through the external carotid arteries :
- dry mucous membranes;
- neck pain;
- distortion of facial expressions, paralysis of facial muscles;
- fainting;
- slurred speech;
- constant pain in the head.
Treatment
Depending on the severity of the disease, conservative and surgical treatment is possible. During surgical intervention, the following is carried out: removal of blood clots, suturing of a vessel, ligation of veins, arteriovenous bypass or other necessary operation.
Conservative treatment includes:
- Drug therapy (anticoagulants, administration of drugs that dissolve blood clots, etc.)
- Diet therapy
- UHF therapy.
Prevention
Preventive actions:
- Using elastic bandages and compression garments
- To give up smoking
- Rational and proper nutrition
- Vitamin therapy
- Physical activity
- Timely treatment of concomitant diseases
- Monitor cholesterol and blood glucose levels
- Reducing body weight.
If symptoms of the disease appear, you can seek advice and examination in Moscow from specialists from the Central Clinical Hospital of the Russian Academy of Sciences. Registration is made by phone...
Forecast
The prognosis for treatment of thrombosis depends on the following factors:
- Where is the carotid artery located and what is its role in the human circulatory system?
- competently prescribed therapy and the patient’s adherence to the doctor’s recommendations, lack of self-medication and ignoring symptoms;
- how quickly medical care was provided after a blood clot formed;
- the presence of concomitant diseases, including those associated with blood vessels (especially cerebral);
- patient's age;
- the degree of severity and nature of changes in brain tissue caused by deterioration of blood supply due to thrombosis (if any).
The timeliness and correctness of medical care is very important.