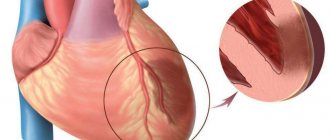
Thrombosis in pregnant women is a pathological condition characterized by the formation of blood clots in the lumen of blood vessels, which are called thrombi. They do not allow blood to circulate freely through the circulatory system, seriously impeding blood flow and causing a number of serious complications. Vein thrombosis in pregnant women is not uncommon. It appears against the backdrop of a number of changes occurring in a woman’s body during this period, and requires special attention both from the woman herself and from doctors.
Prevention of thrombosis in pregnant women and its treatment is one of the areas of work of the CELT Phlebology Department. Our clinic has been operating since 1993 and is multidisciplinary, so phlebologists work closely with gynecologists, achieving the best results. They have at their disposal a powerful diagnostic and treatment base, as well as modern gentle techniques that allow them to maintain the patient’s health and give birth to a healthy baby.
At CELT you can get advice from a phlebologist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Thrombosis in a pregnant woman: causes
During pregnancy, a number of serious changes occur in the female body. First of all, they are associated with hormonal changes, which affect the functioning of the blood coagulation system, causing the blood to become more viscous and thick. Another reason is the increase in the size of the uterus. It begins to exert a compressive effect on the inferior vena cava, causing disruption of the blood flow, leading to stagnation in the vessels of the legs. Another factor is increased body weight. The above leads to the development of thrombophlebitis. It can occur either as an independent disease or as a complication of thrombosis. Aggravating factors in this case are:
- The woman is over 35 years old;
- Congenital antithrombin deficiency;
- Long-term use of contraceptives;
- Serious injuries in the past;
- Presence of autoimmune diseases.
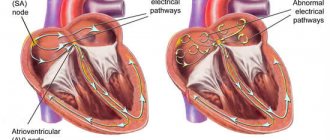
How does blood clotting occur?
The actual clot is formed by creating a fibrin network that strengthens and stabilizes it. This is due to the activation of the coagulation cascade - inactive blood coagulation factors circulating in the blood plasma begin to activate each other.
Under the influence of mechanical damage, platelets secrete thrombokinase, which triggers a number of processes leading to the formation of the corresponding factor that initiates blood clotting - calcium ions and plasma protein factors are important in this process.
Blood coagulation diagram
As a result of the blood clotting cascade, factor X together with factor Va forms a complex called prothrombinase, which converts prothrombin into thrombin. Thrombin, in turn, converts fibrinogen (a plasma protein that circulates in the blood) into fibrin (a water-insoluble protein), which forms a network of fibers that form the backbone of the clot.
Thrombosis in a pregnant woman: clinical manifestations
Thrombosis in pregnant women occurs with the following symptoms:
- Swelling of the affected leg;
- Redness and swelling of the skin around the affected veins;
- Local and general increase in temperature;
- Painful symptoms;
- Numbness of the affected leg;
- Fast fatiguability;
- Visibility of the vascular pattern of the affected limb.
The above is especially evident in the second half of pregnancy, when the uterus greatly increases in size. However, if there is deep vein thrombosis, symptoms appear even later.
Diagnosis of thrombosis in pregnant women
Before prescribing thrombosis treatment to a patient, CELT specialists conduct a comprehensive diagnosis aimed at making an accurate diagnosis. As a rule, the latter does not cause difficulties. Our phlebologist takes a medical history and prescribes the following tests for the pregnant woman:
- Complete blood count - to assess the functioning of the coagulation system;
- Ultrasound scanning of the fetus - to determine its condition and eliminate the risk of hypoxia;
- Dopplerography - to determine the condition of blood veins and detect disturbances in blood flow.
The concept of “thrombophilia” unites all hereditary and acquired disorders of hemostasis, in which there is a predisposition to the early manifestation and recurrence of thrombosis, thromboembolism, ischemia and infarction of organs [2]. For practical purposes, it is very important to distinguish congenital thrombophilia, since we are talking about thrombogenic factors that accompany patients throughout their lives. Congenital thrombophilia is a tendency to thrombosis due to congenital predisposing factors [13], regardless of the cause. For many years, antiphospholipid syndrome (APS) was classified as an acquired form of thrombophilia, but now there is evidence of the genetic nature of the origin of APS [5], which, however, does not prevent this condition from still being classified as thrombophilia. In patients with thrombophilia, thrombotic complications occur in situations where other people do not experience such complications: when oral contraceptives are prescribed, during pregnancy, during uncomplicated surgical operations, during long trips and in an uncomfortable position, etc.
Patients with thrombophilia are characterized by the occurrence of heart attacks and strokes at a young age - up to 50 years - without obvious predisposing factors, as well as thrombosis of unusual locations: retinal vessels, brain, veins of the upper half of the body, superficial epigastric, pudendal veins, ileofemoral thrombosis. Obstetric losses are characterized by early miscarriages, late miscarriages, repeated undeveloped pregnancies, the occurrence of severe forms of late gestosis with termination of pregnancy before 34 weeks, the development of fetal growth restriction syndrome, sudden fetal death syndrome, and premature abruption of a normally located placenta.
Clinical manifestations of thrombophilia are thrombotic complications or obstetric losses, as there are relevant publications in the medical literature [1, 3, 11]. This distinguishes thrombophilia from simple polymorphism of genes, the number of different combinations of which exceeds 1.5 million. Therefore, polymorphism of the genes fibrinogen, factor VIII (FVIII), factor XIII (FXIII), etc. should be considered simple polymorphism of genes, since to date they have not been proven connection with clinical pathology.
Congenital thrombophilias include the following conditions:
- deficiency of anticoagulant proteins: antithrombin III (AT III) below 70% (by activity), protein C (PS) below 65%, protein S (PS) below 55%;
- polymorphism of FV Leiden genes - homo- (A/A) or heterozygous carriage (A/G);
— polymorphism of the prothrombin gene FII G20210A — homo- (A/A) or heterozygous carriage (A/G);
- polymorphism of the methylenetetrahydrofolate reductase (MTHFR) gene C677T - homo- (T/T) or heterozygous carriage (C/T);
- polymorphism of the plasminogen activator inhibitor gene type I (plasminogen activator inhibitor - PAI-I) - homo- (4G/4G) or heterozygous carriage (4G/5G);
— antiphospholipid syndrome (APS), diagnosed according to modern diagnostic criteria in 2006 [10];
- hyperhomocysteinemia - homocysteine content in fasting blood plasma more than 15 mmol/l.
APS can be diagnosed if 1 clinical and 1 laboratory criteria are met. Clinical criteria:
1. Arterial or venous thrombosis without inflammation of the vascular wall.
2. Pathology of pregnancy:
a) one fetal death after 10 weeks of pregnancy or more;
b) eclampsia, gestosis or placental insufficiency in less than 34 weeks of pregnancy;
c) 3 spontaneous abortions or more in less than 10 weeks of pregnancy without anatomical, hormonal, or chromosomal disorders.
Laboratory criteria:
1. Twice positive test for lupus anticoagulant with an interval of 12 weeks;
2. Anticardiolipin antibodies in high titers (more than 40 units), determined by ELISA with an interval of 12 weeks;
3. Presence of antibodies to β-2-glycoprotein-I.
It should be remembered that APS should not be diagnosed in cases where the time interval between clinical and laboratory manifestations is less than 12 weeks and more than 5 years, and superficial venous thrombosis is not included in the criteria for diagnosing APS.
Indications for examination of patients
Examination is prescribed for patients in the event of idiopathic thrombosis, stroke, heart attack, miscarriage, severe gestosis, premature abruption of a normally located placenta, premature birth before 34 weeks of gestation, a history of fetal growth restriction syndrome, thrombosis while taking oral contraceptives or hormone replacement therapy (HRT). Based on the 3-year experience of the Moscow Regional Research Institute of Obstetrics and Gynecology (570 pregnant women with thrombophilia, mainly caused by a combination of heterozygous carriage of the MTHFR and PAI-I genes, were observed), we consider it advisable to screen for thrombophilia in the complicated course of this pregnancy, even in the absence of obstetric complications history, which allows justifying treatment with anticoagulants and preventing the progression of complications.
Normal conditions are considered to be ATIII activity of 70% and above, protein C - 65% and above, protein S - 55% and above; FV Leiden - G/G, prothrombin FII G20210A - G/G, MTHFR C677T - C/C, PAI-I - 5G/5G, homocysteine content in fasting blood plasma below 15 mmol/l.
It is also likely that thrombophilias should include polymorphism of the angiotensin converting enzyme gene (ACE I/D) and polymorphism of the endothelial receptor of protein C (ERPC), respectively associated with relapses of severe gestosis and repeated miscarriages in early pregnancy. .
Diagnosis of thrombophilias
For patients at risk - if there is a history of idiopathic or pregnancy-related thrombosis, or with the use of oral contraceptives, heart attacks, strokes, obstetric losses, severe gestosis, a history of abruption of a normally located placenta, failures when trying in vitro fertilization and embryo transfer - prescribed examination. It is advisable to obtain information as early as possible in order to make a decision on treatment: during prenatal examination, examination in the first trimester of pregnancy, if a complication occurs during this pregnancy.
Testing for thrombophilia includes:
— determination of the percentage of activity of anticoagulant proteins: AT III, PS, PS;
— study of gene polymorphism: FV Leiden, FIIG20210A, MTGFRS677T, PAI-I;
— determination of homocysteine content on an empty stomach;
- study of lupus anticoagulant, antibodies to cardiolipins and antibodies to β2-glycoprotein I.
Blood sampling for genetic studies and determination of homocysteine is carried out in a test tube with ethylenediamineacetic acid; for the determination of lupus anticoagulant, antibodies to cardiolipins and β2-glycoprotein-I in a citrate tube (for example, Monovet-S). When using heparin, test results may be distorted. If one thrombophilia factor is identified, the following diagnosis is made, for example: thrombophilia - heterozygous carriage of FIIG20210A A/G; if several thrombophilia factors are identified, a diagnosis of combined thrombophilia is made with a list of defective factors, for example: combined thrombophilia - heterozygous carriage of FV Leiden A/G, homozygous carriage of PAI-I 4G/4G, hyperhomocysteinemia.
Treatment of pregnant women with thrombophilias
Treatment with anticoagulants in patients with a deficiency of proteins—anticoagulants: antithrombin-III, protein C, protein S—reduced the risk of fetal loss [6].
Patients should be divided into two groups:
- having a history of obstetric losses;
- with a history of thrombotic complications and during current pregnancy.
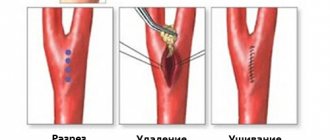
Treatment is possible with both unfractionated heparin (UFH) and low molecular weight heparins (LMWH): fragmin, fraxiparin, clexane. UFH, compared to LMWH, have a more pronounced anticoagulant effect, inactivating active molecules of blood coagulation factors: II, X, IX, XI, XII, reducing the number of microvesicles, increasing the content of tissue factor inhibitor, activating fibrinolytic activity, and inhibiting complement system factors [7]. Treatment with UFH is possible in the form of subcutaneous injections or inhalations through an ultrasonic inhaler. LMWH drugs have their own pharmacokinetics and are not interchangeable. Treatment is carried out in a prophylactic dosage - for UFH 10,000 or 15,000 units subcutaneously and, as a rule, does not require laboratory monitoring.
If there is a history of obstetric losses, treatment begins in the early stages of gestation to ensure adequate placentation from 4-5 weeks to 34 weeks of pregnancy, usually subcutaneous UFH 5000 units 2 times a day with an interval of 12 hours. To exclude heparin-induced thrombocytopenia at 4, 8 and On the 15th day of treatment with UFH, the platelet count should be determined in a clinical blood test. After 34 weeks of gestation, natural involutive changes occur in the placenta, and the use of heparin does not improve pregnancy outcome, theoretically increasing the risk of hemorrhagic complications. In the form of inhalations, heparin is used in a dosage of 500-700 units/kg every 12 hours. If the patient is large (more than 90 kg), heparin can be used in the same dose every 8 hours.
If there are thrombotic complications in a patient with thrombophilia during current pregnancy and a history of treatment after treatment by vascular surgeons, UFH therapy is administered at 5000 units every 12 or 8 hours without laboratory control. Due to the increase in the number of thrombotic complications in pregnant women in the third trimester and in the postpartum period, especially in the first 4 weeks, it is advisable to prescribe a regimen of 5000 units 3 times a day. The use of UFH in a daily dose of up to 20,000 units does not require laboratory control. Delivery, surgery and puncture of the epidural space are safe if the thrombin and activated partial thromboplastin time are normal and the patient’s platelet count is normal [12].
If clinical and laboratory examination does not make it possible to diagnose APS, but there is a constantly high titer of anticardiolipin antibodies, antibodies to anti β2-glycoprotein I, a positive lupus anticoagulant is constantly determined, treatment with UFH is indicated in a prophylactic dose - 5000 units subcutaneously with an interval of 12 hours.
When treating pregnant women with LMWH, achieving prophylactic treatment levels (0.3-0.5 units of anti-Factor Xa activity) is difficult due to the increase in glomerular filtration rate and volume of distribution as pregnancy progresses, so the recommended level of anti-Factor Xa activity can be achieved only with individual dose selection for the patient [4, 8]. Often, treatment with LMWH does not prevent the development of fetal malnutrition, and the use of UFH is preferable.
Treatment of patients with thrombotic complications requires a minimal interruption in the use of drugs during delivery. When carrying out programmed labor and planned cesarean section, the last heparin injection is carried out the night before, before 15:00 the next day, delivery is carried out and 3 hours after birth, heparin therapy is resumed at 5000 units every 12 hours throughout the entire postpartum period. Prescription of a full therapeutic dose of heparin is possible one day after birth and is monitored by the level of activated partial thromboplastin time for UFH and the level of anti-Xa factor for LMWH. Since during normal pregnancy and its complications the D-dimer content is increased, this indicator cannot be used either for diagnostic purposes or to monitor the effectiveness of LMWH treatment [9].
During prophylactic treatment of patients with thrombophilia with heparin, as a rule, there is no need to prescribe other drugs that actively affect the blood coagulation system. The use of other medications is not contraindicated.
This practice of managing pregnant women with thrombophilia allows achieving a favorable pregnancy outcome.
Our doctors
Drozdov Sergey Alexandrovich
Cardiovascular surgeon, phlebologist, Doctor of Medical Sciences
47 years of experience
Make an appointment
Malakhov Yuri Stanislavovich
Doctor - cardiovascular surgeon, phlebologist, Honored Doctor of the Russian Federation, Doctor of Medical Sciences, doctor of the highest category
Experience 36 years
Make an appointment