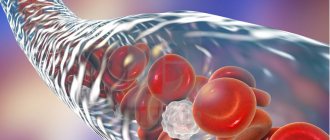
According to the World Health Organization, in most developed countries, deep vein thrombosis and pulmonary embolism have become one of the leading causes of mortality. Millions of people around the world die every year from acute blockage (embolism) of a blood vessel by a thrombus. The danger of thrombosis is that a clot can reach a size comparable to the diameter of a venous vessel and completely block the blood flow in it. Or, if it ruptures, the clot can travel with the blood into the vessels of the lungs and lead to pulmonary thromboembolism. Often with fatal outcome.
Related article Catch it if you can. How to detect and destroy a blood clot
“A blood clot has broken off,” they sometimes say in this case about the cause of death. Even fairly young people often die from detached blood clots. According to specialists from the Moscow State Medical and Dental University named after A. I. Evdokimov, more than 90% of deaths from pulmonary embolism occur in patients who were not diagnosed with embolism and who did not receive treatment.
What causes blood clots?
Thrombi, in the form of blood clots, form in blood vessels in response to damage to the vascular wall, slowing of blood flow and changes in blood composition. “Thrombosis does not occur out of nowhere; there must be some prerequisites. This is facilitated by the presence of varicose veins in the lower extremities. If it is, you should pay attention to compactions that may appear in the veins,” says phlebologist, surgeon Fedor Shpachenko .
According to the phlebologist, compactions may indicate that blood clots have already formed in the veins. “Often, these blood clots may not occur in the superficial veins that we see, but in deep veins, and it is impossible to visualize them without special research methods,” warns Shpachenko.
Who is at risk for blood clots and how to prevent sudden death
— Alexander Ivanovich, what are thromboembolic complications?
— Doctors talk about them when a thrombus occurs in any part of the cardiovascular system, that is, a blood clot in the cavities of the heart or great vessels, part of which can break off and migrate through the bloodstream. With thrombosis of the left atrium or ventricle, a detached thrombus (embolus) enters the aorta, and from there into the vessels of the heart, which can lead to the development of myocardial infarction. Blood clots trapped in the arteries of the head are the cause of ischemic stroke. Blood clots in the intestinal arteries are fraught with intestinal necrosis, and in the arteries of the extremities they threaten gangrene. If a blood clot primarily occurs in the veins of the legs (venous thrombosis), then the detached blood clot enters the pulmonary arteries. The resulting thromboembolism of the pulmonary arteries causes severe cardiopulmonary failure, which often leads to death.
- Why is this happening?
— Venous thrombosis occurs when a number of unfavorable circumstances coincide, which lead to a slowdown in blood flow through the vein of the legs, increased blood clotting and damage (often microscopic) to the venous wall. The speed of blood flow through the veins slows down sharply when people's mobility is limited due to bed rest, long air travel or driving in a car. The clotting potential of the blood increases in response to injury, bleeding, surgery, dehydration, the development of malignant tumors, uncontrolled use of female sex hormones for contraception or for the purpose of replacement, infection. Genetic predisposition is also important - the presence of so-called congenital thrombophilias in people. Venous thromboembolic complications often occur in patients with malignant neoplasms, in patients in trauma and orthopedic hospitals, burn departments; in patients who have suffered cerebrovascular accidents, gynecological operations (including abortion), etc. In fact, it is one of the most common hospital complications. But thromboembolic complications often occur in people at home.
— Who is at risk?
— People leading a sedentary lifestyle and forced to remain in bed; obese; cancer patients; who have undergone bone trauma and various surgical interventions. In addition, persons with dehydration who uncontrollably take female sex hormones and who have a genetic predisposition are at risk of venous thrombosis.
— Are patients capable of conducting such self-diagnosis or is this only a matter for the doctor?
“It is the doctor’s task to identify these complications and anticipate them, but the patient can help him by telling in detail his life history, previous diseases and symptoms that have recently appeared.
— What should you pay attention to, what symptoms should seem alarming?
— It is extremely difficult for the patient, and sometimes even for the doctor, to notice the first symptoms of thrombosis. This may be indicated by pain and swelling of the leg. Unfortunately, they appear only in cases where thrombosis has already had a significant extent. Therefore, these symptoms cannot be called early. In addition, symptoms appear quite late if the patient is forced to remain in bed. Sometimes the first manifestation of such asymptomatic thrombosis may be a life-threatening pulmonary embolism. That is why it is more important not to look for symptoms of already developed thrombosis, but to prevent its occurrence!
- How to prevent them?
— It is very important to lead an active, mobile lifestyle, not to overeat (obesity is one of the significant risk factors), and undergo regular medical examinations, which allows you to identify malignant neoplasms and other serious diseases in the early stages. Women who are planning to take hormonal drugs for contraception or to treat menopausal disorders should definitely discuss this with their gynecologist. Sometimes, to prevent thrombosis, it is enough to quickly activate the patient, make him walk immediately after surgery, and use compression stockings (special elastic socks or stockings). If necessary, doctors prescribe special medications - anticoagulants, the choice of which in modern conditions is quite wide. And finally, if your leg suddenly hurts and swells, or shortness of breath and chest pain occur for no apparent reason, you need to consult a doctor as soon as possible, who has every opportunity to make the correct diagnosis and prescribe the necessary treatment.
— According to the international study ENDOSE, in Russia only 26% of patients in surgical departments receive adequate prophylaxis, while in Germany, for example, this figure is 92%. What is the reason?
— For quite a considerable time in Russia, the leading causes of death of patients in surgical hospitals were hemorrhagic and infectious complications. With the introduction of new technologies and advances in the treatment of surgical infections, the frequency of these complications has decreased significantly, and venous thrombosis and pulmonary embolism began to take first place in their structure. This happened earlier in Western countries. In addition, clinical standards of treatment and prevention have long been in place there, which we began to introduce relatively recently. The unfavorable state of prevention of hospital thromboembolic complications prompted the Russian Society of Surgeons and the Association of Phlebologists of Russia to initiate the project “Territory of Safety from Venous Thromboembolic Complications.” The goal of the project was to introduce into the minds of doctors and into the practice of surgical hospitals the ideology of preventing these complications in various Russian regions. This is justified both from a medical, ethical, and financial point of view (the costs of prevention are many times lower than the costs of treating complications that have already arisen). Over time, the surgeons will be joined by therapists, neurologists, cardiologists, obstetricians-gynecologists, orthopedic traumatologists and representatives of other medical specialties. The implementation of the project made it possible to train doctors in the principles of risk assessment and effective prevention of these common complications; many of our patients were saved, saved from the disabling consequences of thrombosis and embolism, and their usual quality of life was preserved.
Who is at risk?
Those who are most likely to develop thrombosis are people who are obese and have varicose veins, women who take oral contraceptives, and those who take many long flights. But a high risk of blood clots occurs when all these factors are combined.
“Patients with obesity and varicose veins are at risk. As for medications, in particular oral contraceptives, now most of them are well balanced and we rarely see the development of thrombosis and thromboembolism in women taking these drugs. People with a sedentary lifestyle, impaired hemostasis, namely blood clotting disorders, also fall into this group. If the patient has all these provoking factors, then the risk of developing thrombosis increases. Age also makes it worse. Over the years, the vessels lose elasticity and become brittle, plus a number of concomitant diseases cause swelling of the lower extremities,” says Shpachenko.
If a blood clot comes off, what should you do?
If a person has a blood clot, then you cannot hesitate to call an ambulance. Moreover, even a doctor will not be able to make an accurate diagnosis without special equipment. Therefore, the victim must be urgently hospitalized.
There can be two treatment regimens for thrombosis: either the patient is prescribed medication correction or he is referred for surgery.
Drug therapy includes:
- Prescription of anticoagulants. These drugs help thin the blood (Heparin, Warfarin).
- Course treatment with statins.
- Prescription of fibrinolytics.
- Prescribing thrombolytics, which are necessary to dissolve the blood clot.
If the problem cannot be solved with the help of medications, or the person develops complications of thrombosis, he is indicated for an operation called thrombectomy. It is also possible to install special vena cava filters that will “catch” blood clots, preventing them from clogging vital vessels.
How to diagnose thrombosis at an early stage?
Thrombosis at an early stage can be detected with timely diagnosis of the veins of the lower extremities. To confirm or refute the diagnosis, phlebologists often recommend laboratory and ultrasound duplex scanning (USD) of the veins. This diagnostic method allows you to see the walls and lumen of the veins, the presence of a blood clot in them, its size, and even roughly judge how long ago the process is. You can also do angiography: a contrast study of blood vessels. And the predisposition to the appearance of blood clots can be identified using a coagulogram: a comprehensive analysis of blood clotting indicators.
How to prevent a blood clot from breaking off
People whose blood relatives suffered from thrombosis will have a high risk of developing a similar disease. Therefore, you should be regularly examined by a doctor to detect dangerous vascular growths. Modern medicine has all the necessary tools to detect a blood clot and prevent its rupture.
If a person’s blood has increased clotting, he will be prescribed medications (antiplatelet agents). Sometimes they need to be taken for life. It should be noted that only a doctor can recommend them, otherwise you can cause serious harm to your own health.
If the doctor diagnoses a blood clot that is highly likely to break off, the patient is urgently hospitalized and prepared for surgery.
People with thrombosis should strictly follow their doctor's instructions. They are not recommended to take a hot bath, visit saunas and steam baths, as all these procedures increase blood flow through the vessels. A ban is also imposed on visiting massage rooms and using warm compresses.
To prevent blood from stagnating in the veins, it is necessary to move as much as possible, engage in physical exercise, and walk a lot.
If the patient is at risk of blood clot rupture, then strict bed rest is indicated. Self-treatment of thrombosis or wait-and-see tactics in this case is unacceptable.
A menu containing foods that lower blood cholesterol should be a priority. This will prevent the formation of atherosclerotic deposits on the vessels, and therefore reduce the risk of thrombosis. For this purpose, you can include sea fish, seafood, broccoli, spinach, new potatoes, and dairy products in your diet.
How to determine deep vein thrombosis?
Thrombosis often occurs asymptomatically or with mild symptoms. The nature of patient complaints may vary depending on the location of the blood clot, the duration of the disease and the nature of the lesion. The main symptom of deep vein thrombosis is pain in the leg, namely in the calf muscle. Swelling may also be a concern. When a blood clot forms in the deep veins of the lower extremities, the skin may take on a reddish or blue tint.
Article on the topic
Dissolve the clot. What foods improve blood quality
“Signs of thrombosis can manifest themselves as swelling and pain in the lower extremities, and the location of this pain can be very diverse. Sometimes you can’t guess what the pain is due to: either osteochondrosis, or blood clots, or other diseases. Therefore, if your legs swell, or there are varicose veins in your legs, then you should pay attention to the possible development of blood clots,” says Shpachenko. An ultrasound duplex scan or angiography will help you understand the exact picture.
Symptoms of the disease
It is quite difficult to diagnose yourself. And if a blood clot comes off, it’s even more difficult.
A blood clot that breaks off in the heart, lungs, or brain usually results in death.
But experts call a number of symptoms that signal serious danger:
- if the pathogen has formed in the leg, then it begins to hurt, heat up, turn red and swell;
- if it reaches the brain, then speech and coordination are impaired, paralysis appears, the face becomes distorted - all signs of a stroke;
- if in the vein that carries blood from the brain, then vision deteriorates and the head hurts;
- if in the pulmonary arteries, then the person begins to choke and turn blue;
- if in the digestive organs, then vomiting and pain in the stomach appear, which radiates to the shoulder;
- if in the heart, then sharp pain, tachycardia, loss of consciousness;
- if in the portal vein, then abdominal pain appears and liver cirrhosis gradually develops.
Usually everything happens suddenly. Few people can understand in practice what it means that a blood clot breaks off and a person dies.
How is pulmonary embolism diagnosed?
As a result of pulmonary embolism, cardiac function, pulmonary blood flow and gas exchange are disrupted. This condition is accompanied by characteristic symptoms, primarily a rapid heartbeat. There may also be a stabbing pain in the chest that gets worse while breathing. Patients may experience severe shortness of breath, and the respiratory rate may increase to 30-40 per minute. In addition, cyanosis or pallor of the skin, decreased blood pressure, cough, and hemoptysis may be observed.
“In the case of pulmonary embolism, difficulty breathing and chest pain may occur. In people with a disease of the vascular-cardiac system, for example, atrial fibrillation, pulmonary embolism can occur quite often,” says Shpachenko.
If thromboembolism is suspected, urgent hospitalization is required. To confirm the diagnosis, the hospital will order electrocardiography, chest x-ray and echocardiography. A radionuclide scan of the lungs, probing of the right side of the heart, and computed tomography with contrast of the pulmonary arteries can also be performed.
Causes of blood clot separation
The thrombus can be parietal, or it can be floating. If a blood clot is located near a cholesterol plaque, it is less likely to come off than a floating blood clot. The latter “sits” on a thin leg, which has a weak attachment to the vascular wall. It is floating blood clots that most often lead to the development of pulmonary embolism and strokes.
Also, wandering blood clots may be present in the body, which pose a serious threat to life.
A blood clot can break off as a result of the following influences:
- The blood flow accelerates greatly.
- A thrombus has formed in a wide vessel.
- The stem of the thrombus is weak.
After breaking off, the thrombus begins traveling with the bloodstream along the vascular bed. At this time, it often breaks up into small fractions. Once in a vessel that does not exceed its size, the thrombus clogs it. This entails stopping blood flow and disrupting the nutrition of the limb or organ. This pathological condition is called occlusion.
Possible consequences
They depend on where the blood clot clogged the vessel:
- if in the brain, then a stroke occurs;
- if in the coronary arteries - myocardial infarction;
- if in the intestines, then - necrosis, peritonitis of this organ;
- if in the legs, then gangrene is possible.
Stagnant blood is a favorable environment for microorganisms. An infected embolus can cause sepsis.