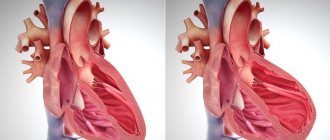
Myocardial dystrophy
Myocardial dystrophy with anemia
Disturbances in the myocardium develop when hemoglobin decreases to 90-80 g/l.
Against this background, hemic hypoxia develops, accompanied by energy deficiency in the myocardium. Anemic myocardial dystrophy can occur with iron deficiency and hemolytic anemia, with acute and chronic blood loss, and disseminated intravascular coagulation syndrome. Clinical manifestations of myocardial dystrophy in anemia include pallor of the skin, dizziness, shortness of breath, tachycardia, and increased pulsation of the carotid arteries. Percussion examination reveals expansion of the borders of the heart, indicating myocardial hypertrophy. Auscultation reveals loud heart sounds, systolic murmurs over the heart and blood vessels, and a “spinning top noise” on the cervical vessels. Heart failure develops with prolonged anemia and inadequate treatment.
Myocardial dystrophy with thyrotoxicosis
Under the influence of an excess amount of thyroid hormones in the heart muscle, the synthesis of adenosine triphosphoric acid (ATP) and creatine phosphate (CP) is reduced, which is accompanied by energy and then protein deficiency. At the same time, thyroid hormones stimulate the activity of the sympathetic nervous system, causing an increase in heart rate, minute blood volume, blood flow velocity, and bcc. Under such conditions, changes in intracardiac hemodynamics cannot be supported energetically, which ultimately leads to the development of myocardial dystrophy.
In the clinic of myocardial dystrophy in thyrotoxicosis, arrhythmias (sinus tachycardia, extrasystole, paroxysmal tachycardia, atrial fibrillation) predominate. Long-term thyrotoxicosis causes chronic circulatory failure, mainly of the right ventricular type, which is manifested by pain in the heart, edema, and hepatomegaly. Sometimes, with thyrotoxicosis, the symptoms of myocardial dystrophy dominate, and therefore patients turn, first of all, to a cardiologist, and only then go to an endocrinologist.
Myocardial dystrophy with hypothyroidism
The pathogenetic basis of myocardial dystrophy in hypothyroidism is a deficiency of thyroid hormones, leading to a decrease in metabolic activity in the myocardium. In this case, as a result of increased vascular permeability, fluid retention occurs in myocytes, which is accompanied by the development of dysmetabolic and electrolyte disorders (increased sodium content and decreased potassium).
Myocardial dystrophy in hypothyroidism is characterized by constant aching pain in the heart, arrhythmias (sinus bradycardia), blockades (atrial, atrioventricular, ventricular).
Alcoholic and toxic myocardial dystrophy
It is believed that alcoholic myocardial dystrophy is caused by daily intake of 80-100 ml of ethyl alcohol for 10 years. However, with a hereditary deficiency of a number of enzymes that break down ethanol, stress, and frequent viral infections, myocardial dystrophy can develop in a shorter time - within 2-3 years, even when consuming smaller amounts of alcohol. Alcoholic myocardial dystrophy occurs mainly in men 20-50 years old.
Toxic myocardial dystrophy occurs in individuals receiving long-term therapy with immunosuppressants (cytostatics, glucocorticosteroids), NSAIDs, some antibiotics, tranquilizers, as well as in cases of poisoning with chloroform, phosphorus, arsenic, carbon monoxide, etc. Such variants of myocardial dystrophy can occur in cardialgic (painful) conditions. , acute arrhythmic, combined and congestive forms.
The cardialgic form of myocardial dystrophy is characterized by pinching or aching pain in the chest, a transient sensation of heat or chilliness in the extremities, and sweating. Patients are concerned about general weakness, fatigue, decreased physical endurance, and headaches.
The arrhythmic form of myocardial dystrophy is accompanied by tachycardia, disturbances of rhythm and conduction of the heart (sinus tachy- or bradycardia, extrasystole, bundle branch blocks), sometimes - attacks of fibrillation and atrial flutter. In the combined form of myocardial dystrophy, arrhythmias and cardialgia are observed. Manifestations of congestive myocardial dystrophy are caused by heart failure and include shortness of breath on exertion, cough, attacks of cardiac asthma, swelling in the legs, hydropericardium, hydrothorax, hepatomegaly, ascites.
Tonsillogenic myocardial dystrophy
Myocardial lesions during tonsillitis occur in 30-60% of patients. Tonsillogenic myocardial dystrophy usually develops after a series of tonsillitis, occurring with high fever and intoxication. In the clinic of tonsillogenic myocardial dystrophy, complaints of intense pain in the heart area, severe weakness, irregular pulse, shortness of breath, focal or diffuse sweating, low-grade fever, and arthralgia prevail.
Myocardial dystrophy of physical overexertion
Develops in athletes who perform physical activity that exceeds their individual capabilities. In this case, myocardial damage can be caused by hidden chronic foci of infection in the body - sinusitis, tonsillitis, adnexitis, etc.; lack of proper rest between workouts, etc. Regarding the pathogenesis of myocardial dystrophy of physical exertion, a number of theories have been put forward: hypoxic, neurodystrophic, steroid-electrolyte.
This variant of myocardial dystrophy is mainly manifested by general symptoms: weakness, lethargy, fatigue, depressed mood, decreased interest in sports. Palpitations, tingling in the heart area, and interruptions may occur.
Menopausal myocardial dystrophy
Develops as a result of dishormonal processes in women aged 45–50 years. Menopausal myocardial dystrophy is manifested by pain in the heart area of a pressing, stabbing or aching nature, radiating to the left arm. Cardialgia intensifies due to “hot flashes” and is accompanied by a feeling of heat, rapid heartbeat, and increased sweating. Heart failure in menopausal myocardial dystrophy can develop with existing concomitant arterial hypertension.
Urolithiasis (UCD)
General principles of therapy
Both surgical treatment methods and conservative therapy are used.
Treatment tactics are determined by the urologist depending on the age and general condition of the patient, the location and size of the stone, the clinical course of urolithiasis, the presence of anatomical or physiological changes and the stage of renal failure. As a rule, surgical treatment is necessary to remove stones from urolithiasis. The exception is stones formed by uric acid derivatives. Such stones can often be dissolved by conservative treatment of urolithiasis with citrate mixtures for 2-3 months. Stones of other compositions cannot be dissolved.
The passage of stones from the urinary tract or surgical removal of stones from the bladder or kidney does not exclude the possibility of recurrence of urolithiasis, therefore it is necessary to implement preventive measures aimed at preventing relapses. Patients with urolithiasis are recommended for complex regulation of metabolic disorders, including care for maintaining water balance, diet therapy, herbal medicine, drug therapy, physical therapy, balneological and physiotherapeutic procedures, and sanatorium-resort treatment.
Diet therapy
The choice of diet depends on the composition of the stones found and removed. General principles of diet therapy for urolithiasis:
- A varied diet with a limited amount of food;
- Restriction in the diet of foods containing large amounts of stone-forming substances;
- Take a sufficient amount of fluid (daily diuresis of 1.5-2.5 liters should be ensured).
For urolithiasis with calcium oxalate stones, it is necessary to reduce the consumption of strong tea, coffee, milk, chocolate, cottage cheese, cheese, citrus fruits, legumes, nuts, strawberries, black currants, lettuce, spinach and sorrel. In case of ICD with urate stones, you should limit the intake of protein foods, alcohol, coffee, chocolate, spicy and fatty foods, and exclude meat foods and offal (liver sausages, pates) in the evening.
If you have phosphorus-calcium stones, avoid milk, spicy foods, spices, alkaline mineral waters, and limit the consumption of feta cheese, cheese, cottage cheese, green vegetables, berries, pumpkin, beans and potatoes. Sour cream, kefir, red currants, lingonberries, sauerkraut, vegetable fats, flour products, lard, pears, green apples, grapes, and meat products are recommended.
Stone formation in urolithiasis largely depends on the pH of the urine (normally 5.8-6.2). Eating certain types of food changes the concentration of hydrogen ions in the urine, which allows you to independently regulate the pH of the urine. Plant and dairy foods alkalize urine, and animal products acidify. You can control the acidity level of urine using special paper indicator strips, freely sold in pharmacies.
If there are no stones on ultrasound (the presence of small crystals - microlites is allowed), “water shocks” can be used to flush the kidney cavity. The patient takes 0.5-1 liter of liquid on an empty stomach (low-mineralized mineral water, tea with milk, dried fruit decoction, fresh beer). If there are no contraindications, the procedure is repeated every 7-10 days. In cases where there are contraindications, “water shocks” can be replaced by taking a potassium-sparing diuretic drug or a decoction of diuretic herbs.
Phytotherapy
During the treatment of urolithiasis, a number of herbal medicines are used. Medicinal herbs are used to accelerate the passage of sand and stone fragments after extracorporeal lithotripsy, and also as a prophylactic agent to improve the condition of the urinary system and normalize metabolic processes. Some herbal preparations help increase the concentration of protective colloids in the urine, which prevent the process of salt crystallization and help prevent relapse of urolithiasis.
Treatment of infectious complications
With concomitant pyelonephritis, antibacterial drugs are prescribed. It should be remembered that complete elimination of urinary infection in urolithiasis is possible only after eliminating the root cause of this infection - a stone in the kidney or urinary tract. There is a good effect when prescribing norfloxacin. When prescribing drugs to a patient with urolithiasis, it is necessary to take into account the functional state of the kidneys and the severity of renal failure.
Normalization of metabolic processes
Metabolic disorders are the most important factor causing relapses of urolithiasis. Benzbromarone and allopurinol are used to reduce uric acid levels. If the acidity of urine cannot be normalized by diet, the listed drugs are used in combination with citrate mixtures. When preventing oxalate stones, vitamins B1 and B6 are used to normalize oxalate metabolism, and magnesium oxide is used to prevent crystallization of calcium oxalate.
Antioxidants that stabilize the function of cell membranes - vitamins A and E - are widely used. If the level of calcium in the urine increases, hypothiazide is prescribed in combination with drugs containing potassium (potassium orotate). For disorders of phosphorus and calcium metabolism, long-term use of bisphosphonates is indicated. The dose and duration of taking all drugs is determined individually.
Treatment of urolithiasis in the presence of kidney stones
If there is a tendency to spontaneous passage of stones, patients with urolithiasis are prescribed medications from the group of terpenes (extract of the fruit of ammi dentifrice, etc.), which have a bacteriostatic, sedative and antispasmodic effect.
Relief of renal colic is carried out with antispasmodics (drotaverine, metamizole sodium) in combination with thermal procedures (heating pad, bath). If ineffective, antispasmodics are prescribed in combination with painkillers.
International Classification of Diseases for Oncology, 3rd edition (ICD-O-3)
Definitions and purposes of classification
ICD-O-3 is used in cancer patient registration systems (oncology registries) to encode data on the topography and morphology of tumors based on the histological report.
Classification structure
ICD-O has a multi-axial structure with a coding system for topography, morphology, behavior of the neoplasm and its biological properties.
In the topographic axis, for all existing types of neoplasms (except for categories related to secondary tumors and specific morphological types of neoplasms), the ICD-10 classification of malignant neoplasms is used, which allows for more detailed indication of the location of benign tumors. Unlike ICD-10, ICD-O includes the topography of foci of hematopoietic and reticuloendothelial tumors.
The morphological axis provides five-digit coding ranging from M-8000/0 to M-9989/3. The morphological code has 5 characters: the first four indicate the histological type, the fifth - the biological properties of the tumor [/0 - benign tumor; /1 - unclear whether the tumor is benign or malignant; /2 non-invasive cancer, /3 - cancer, primary focus; /6 - MN, metastasis; /9 - ZN. it is unclear whether it is a primary or metastatic lesion. Within the classification, there is also a separate one-digit code that allows determining the degree of histological differentiation.
Classification status:
Date of creation:
1976
Last modified date:
year 2000
Description of changes:
Updates have been made to the nomenclature and classification regarding the section of hematological neoplasms and tumors of the brain and spinal cord.
Reference documents
Indexes:
"A single combined index of topographic and morphological categories."
Available format:
- The index is available in CSV database format.
ICD-O training and educational materials:
With the support of the European Cancer Registry Network, the International Agency for Cancer Research, the European Commission and the US National Cancer Institute, the following training courses have been developed:
- https://www.encr.com.fr
Languages
Training is available in Chinese, Czech, English, Finnish, Flemish/Dutch, French, German, Japanese, Korean, Portuguese, Spanish, Romanian and Turkish.
Relation to other classifications
Revision version correspondences:
There are correspondence tables between revision versions of ICD-O and between revision versions of ICD-O and ICD-9/ICD-10, respectively.
Compliance with international and national classifications:
The topographic classification of ICD-O largely coincides with the ICD-10 classification applied to malignant tumors, from a conceptual and structural point of view. ICD-O was originally based on the American Cancer Society's Manual of Tumor Nomenclature Coding and Nomenclature (MOTNAC), first published in 1951.
Relation to other terminologies
There is an agreement between the World Health Organization and the College of American Pathologists that the section on morphology (ranging from M-8000 to M-9989) was borrowed from SNOMED (Systematized Nomenclature of Medical Clinical Terms). An update to the SNOMED medical nomenclature in 1993 resulted in inconsistencies for non-neoplastic pathologies. For this reason, ICD-O-3 no longer uses SNOMED codes to classify non-neoplastic pathologies.
Responsible persons
WHO Secretariat, European Cancer Reporting Network, mediated by the International Agency for Research on Cancer
150, cours Albert Thomas 69372 Lyon Cedex 08, France
Phone: (33) 4 72 73 80 56; Fax: (33) 4 72 73 86 96
Email ;
Contact Information:
Dr David Forman
International Agency for Research on Cancer 150, courses Albert Thomas 69372 Lyon Cedex 08, France Telephone: (33) 4 72 73 80 56; Fax: (33) 4 72 73 86 96 E-mail
Dr Robert Jakob
World Health Organization 20 Av. Appia 1211 Geneva 27, Switzerland E-mail