Diagnosis of angina pectoris
An important task in the treatment of cardiovascular diseases is the differential diagnosis of angina pectoris. In most cases, angina pectoris is a symptom of coronary heart disease that develops as a result of cholesterol deposition on the inner walls of blood vessels, so the efforts of cardiologists should be aimed at diagnosing the latter.
If you feel discomfort and pain in the chest or left shoulder after heavy exercise or stress, immediately contact a cardiologist. Self-medication can worsen the course of the disease.
Remember, only a specialist using modern diagnostic tools can identify coronary heart disease, prescribe treatment and prevent a tragic outcome!
Differential diagnosis of angina and other cardiovascular diseases
Cardiologist of the Department of Cardiology No. 1 Verbitsky V.L.
In some patients with a typical clinical picture of angina pectoris and positive stress tests (according to objective criteria), coronary angiography does not find any changes in the coronary arteries; Such patients have no signs of spontaneous angina. In these cases, we can talk about coronary artery disease with unchanged coronary arteries. In the English-language literature, this type of pathology is called “X syndrome.” Special studies show that in these patients the ability of the coronary arteries to dilate is significantly reduced, which is detected when assessing coronary blood flow using argon or rubidium radionuclides under the conditions of a dipyridamole test. When performing a myocardial biopsy in these patients, electron microscopy reveals degenerative changes in cardiomyocytes. Thus, both the decrease in coronary reserve and biopsy data allow us to think of “syndrome X” as the initial manifestations of dilated cardiomyopathy. This diagnosis becomes even more reliable if patients have persistent or transient (appearing under load) blockade of the left branch of the His bundle.
With mitral valve prolapse syndrome, there is a pressing or burning pain in the third or fourth intercostal space to the left of the sternum. Much less often the pain is localized behind the sternum or xiphoid process. Mild pain can last for hours, intensifying after physical and emotional stress. When intensified, the pain can cover the entire heart area. In some patients, the pain is relieved by nitroglycerin. The pain is often combined with cardiac arrhythmias (extrasystole, atrial fibrillation, atrioventricular block). It is believed that mitral valve prolapse predisposes to spasm of the coronary arteries. This syndrome is more common in patients with an asthenic build with a flat chest - with a reduced anteroposterior size. In patients with mitral valve prolapse, abnormalities of the ST segment and T wave are often detected, especially when performing an exercise test. On FCG and during auxultation in patients, a mesosystolic murmur is detected at the apex, which is often preceded by a mesosystolic click. The diagnosis of mitral valve prolapse has improved significantly due to the widespread use of ultrasound methods of cardiac examination in the clinic. It allows you to detect prolapse of one or both mitral valve leaflets into the atrium. Valuable diagnostic data can be obtained by ventriculography. Establishing a diagnosis of mitral valve prolapse does not exclude the simultaneous presence of stenosing coronary atherosclerosis in the patient.
Valvular stenosis of the aortic mouth, like arterial hypertension, leads to overload and hypertrophy of the left ventricle, increasing the myocardial oxygen demand. The shortening of the period of diastolic filling of the left ventricle observed with a defect of this type contributes to a decrease in coronary blood flow. These patients often complain of pain in the heart area. In the early stages of the disease, they have the character of cardialgia, and with severe aortic stenosis, typical attacks of angina occur. If a systolic murmur is heard on the aorta in patients with angina, then it is necessary to carry out all available diagnostic studies aimed at identifying aortic stenosis. The diagnosis of aortic stenosis is made on the basis of the characteristic systolic murmur (diamond-shaped murmur on a phonocardiogram), physical, radiological and electrocardiographic signs of left ventricular hypertrophy. X-rays often reveal calcification of the aortic valve. Echocardiographic data are of great differential diagnostic importance. Detection of aortic stenosis does not exclude the simultaneous presence of atherosclerosis of the coronary arteries. Aortic stenosis in a patient with angina pectoris, combined with attacks of cardiac asthma, has a dire prognosis.
With mitral heart disease, patients often complain of pain in the heart area, in some cases indistinguishable from angina. The cause of this pain may be pulmonary hypertension, characteristic of mitral stenosis, pathogenetically associated with insufficient blood supply to the hypertrophied right ventricle. Sometimes pain sensations have a neurotic basis, but typical attacks of angina pectoris are highly likely to indicate a concomitant stenotic lesion of the coronary arteries of the heart, which is confirmed by coronary angiography data. When carrying out a differential diagnosis of angina pectoris, it is necessary to exclude aortalgia - pain accompanying inflammatory and degenerative diseases of the aorta. With syphilitic aortitis, which is rare in our time, aortic insufficiency occurs; the pathological process also affects the mouths of the coronary arteries of the heart, which can be accompanied by typical attacks of angina. With nonspecific aortoarteritis, typical angina is rarely observed; prolonged pain in the heart area without irradiation is characteristic.
With an aortic arch aneurysm, numerous accompanying symptoms caused by compression of neighboring organs (cough, dysphagia, hoarseness, visual disturbances, fainting, asymmetrical pulse, compression of the superior vena cava) help to make a correct diagnosis. With aortic dissection, the pain is of maximum intensity from the very beginning. The widest irradiation is characteristic: pain, starting behind the sternum, then radiates to the neck, back, abdominal area, along the spine and even to the legs. Spider fingers and other signs of Marfan syndrome may lead the doctor to believe that chest pain is related to aortic dissection, to which these patients are predisposed.
Pain in the heart area is the most common and one of the early symptoms of myocarditis . They are varied, unlike angina pectoris, they last for hours and days. In the acute period of the disease, the intensity of pain may vary, but the pain is almost constant. When diagnosing, it is necessary to take into account the connection with a recent infection, fever, leukocytosis, and enlargement of both ventricles of the heart. With a more or less prolonged course, cardiomegaly and heart failure become obligatory symptoms of myocarditis. Differential diagnostic difficulties more often arise with mild heart damage, when after a sore throat, flu or other infection, unpleasant sensations appear in the heart area, accompanied by changes in the final part of the ventricular ECG complex. Patients have a tendency to tachycardia and shortness of breath, and a systolic murmur is heard. More often, these symptoms are manifestations of infectious-allergic myocarditis; they gradually undergo a reverse development.
Pain in the heart area is a common occurrence in people suffering from alcoholism. In this case, a diagnosis of coronary artery disease is often made, and pain is regarded as angina pectoris. Difficulties in diagnosis are associated with the fact that patients hide alcohol abuse. The ECG often reveals nonspecific changes in the ST segment and T wave. A bicycle ergometer test may be positive. X-rays reveal an expansion of the borders of the heart. An echocardiogram reveals dilatation of the left ventricle. Dynamic observation of patients shows worsening myocardial damage and the appearance of severe arrhythmias provoked by large amounts of alcohol. Diagnosis of alcoholic cardiopathy is facilitated by simultaneous signs of liver damage. Many cardiovascular disorders in these patients are associated with autonomic disorders, which manifest themselves very early, even before the development of severe myocardial damage. Coronary angiography, as a rule, does not reveal stenotic lesions of the coronary arteries.
is often mistaken for ischemic heart disease in patients with neurocirculatory dystonia (we used one of many designations for the disease). Cardiac syndrome with neurocirculatory dystonia is long-lasting and persistent. The pain is mostly stabbing or aching, localized mainly in the apex of the heart or in the second to fourth intercostal space to the left of the sternum. The pain is relieved or reduced by taking valocordin, validol, sedatives, and using mustard plasters.
Vegetative-dystonic syndrome in neurocirculatory dystonia is manifested by lability of pulse and blood pressure, peripheral vascular disorders, and vegetative-vascular paroxysms of predominantly sympathetic-adrenal origin. Asthenic syndrome is characterized by both physical and intellectual exhaustion and a significant decrease in performance. Weakness (of a neurogenic nature) manifests itself primarily in the morning. During the day, the feeling of weakness and fatigue may increase, forcing patients to go to bed. Neurocirculatory dystonia is characterized by a syndrome of neurotic respiratory disorders: a feeling of lack of air, dissatisfaction with inhalation and yawning, the need to periodically take deep breaths. Sometimes the feeling of suffocation or a lump in the throat comes first. Periods of “paroxysmal shortness of breath of a neurotic” are less common. Eggs with neurocirculatory dystonia never feel completely healthy; they always exhibit some syndrome or a combination of several. The onset or exacerbation of the disease is usually associated with a stressful situation (mental and physical stress), less often with infectious exposure or hormonal changes (pregnancy, abortion, dysvariant disorders, menopause).
The long-term existence of cardiovascular disorders without clear organic heart pathology favors the diagnosis of neurocirculatory dystonia. ECG changes concern only the final part of the ventricular complex. With normal heart sizes and normal position of the electrical axis, biphasic or negative T waves are recorded, especially in the chest leads. To more accurately interpret ECG abnormalities, a number of functional and pharmacological tests have been proposed. Hyperventilation and orthostatic tests lead to the appearance or deepening of isoelectric or negative T waves in the chest leads. After stopping the test, the ECG approaches the initial level. Tests with propranolol and potassium chloride, with positive results, are characterized by the transition of a negative or biphasic T wave to a positive one. Positive test results are more often observed in neurocirculatory dystonia, indicating that changes in the final part of the ventricular complex are associated with functional disorders. However, the differential diagnostic value of these tests should not be overestimated. A positive test with propranolol rather indicates increased activity of the sympathetic-adrenal system, which also happens with coronary pathology. The bicycle ergometer test is negative in most patients. Patients often refuse to undergo it until diagnostic criteria are reached due to fear or fatigue. In these cases, other stress tests become more valuable. The dipyridamole test in these patients is usually negative. The isoproterenol test is occasionally false-positive in hypersympathicotonia. Transesophageal electrical stimulation of the atria has great diagnostic value.
In patients in this category, it is extremely important to conduct the entire complex of stress tests. If all tests are negative, then the diagnosis of IHD is confidently removed. If some of the samples are positive, then patients need to undergo coronary angiography. Excluding coronary pathology allows you to more clearly formulate the diagnosis and choose treatment.
When establishing a diagnosis of neurocirculatory dystonia, it is necessary to take into account possible variants of the course of the disease (from mild to severe). The lung is characterized by relative monosymptomatics, spontaneous disappearance of symptoms, and preservation of tube ability are possible. The ECG is usually slightly changed. Drug therapy is often not needed. Moderately severe disease is long-term, with an abundance of symptoms, decrease or temporary loss of disability; patients require drug therapy. A severe course is characterized by persistence and multiplicity of pathological symptoms without a tendency to disappear, and the ability to work is reduced.
The severity of the clinical manifestations of neurocirculatory dystonia is determined mainly by the severity of tachycardial and asthenic syndromes, as well as the presence of vegetative-vascular paroxysms, the addition of cardiophobia and other severe psycho-emotional disorders. Among the many complaints of a patient with neurocirculatory dystonia, it is necessary to highlight the meager, but quite identifiable symptoms of angina pectoris. It is necessary to take into account the possibility of a combination of ischemic heart disease and neurocirculatory dystrophy, which makes it possible to make both diagnoses simultaneously. Usually in such cases the doctor relies on coronary angiography data.
Interview and examination of the patient
An important role in the differential diagnosis of angina pectoris is played by questioning and examination of the patient. When compiling a medical history, the cardiologist studies all the symptoms that concern the patient, risk factors, for example, the presence of bad habits, obesity, etc., as well as possible genetic predisposition. During the examination, the doctor listens to heart sounds, looks for signs of damage to the main arteries, as well as signs of lipid metabolism disorders - one of the main causes of the formation of cholesterol plaques. Externally, they manifest themselves in the appearance of xanthoma and xanthelasma - skin neoplasms of a characteristic yellow color.
Causes of angina pectoris
One of the main reasons for the development of angina pectoris is atherosclerosis. There are a number of risk factors under the influence of which the disease not only begins, but also progresses.
Unavoidable factors for exertional angina are genetic predisposition, the person’s gender and age. Until approximately 50-55 years of age, men are more susceptible to angina pectoris. After menopause in women, that is, after 50 years, the percentage of patients of different sexes equalizes.
Avoidable risk factors:
- Smoking.
- Physical inactivity.
- Diabetes. The disease cannot be completely defeated, but following the doctor’s recommendations reduces its severity and, accordingly, reduces the likelihood of changes in the blood vessels.
- Arterial hypertension. Just like with diabetes, controlling the course of the disease reduces the risk of complications.
- Obesity.
- Psycho-emotional stress.
- High cholesterol levels.
Holter monitoring
Daily, or Holter, monitoring is a continuous process of monitoring the patient’s heart throughout the day using a special recorder, the data from which is sent to the stationary equipment of the attending physician. This type of ECG allows you to diagnose unstable angina and angina in the absence of symptoms, helps evaluate previously prescribed treatment, records changes in the cardiogram during exercise, stress, sleep, etc. It can be either outpatient or inpatient, it depends on the purpose of the study and the patient’s well-being.
Signs of exertional angina
The degree of angina pectoris determines the clinical picture of the disease. But the main manifestation for all stages of the disease is an attack of pain. Typical course of a pain attack:
- The pain begins during physical work, at a time of stress. It is typical for an attack to occur in cold or windy weather.
- The pain is most often concentrated behind the sternum with irradiation to the scapula, neck, and lower jaw. Patients describe the pain as squeezing, burning, cutting.
- The duration of pain is from 2 to 15 minutes. With a prolonged attack, the possibility of developing a heart attack cannot be ruled out.
- The intensity of the attack decreases after taking nitroglycerin and when physical work stops.
Symptoms of angina pectoris include weakness, shortness of breath, interruptions in heart function, a decrease or increase in blood pressure, and cold sweat. Some patients experience pale skin, increased urination, and dry mouth.
Attacks can recur from several times a day to two or three episodes a month. Unstable angina pectoris manifests itself more clearly, its symptoms intensify over time.
Load tests
Electrocardiography with physical activity (Stress ECG, Veloergometry) is a very useful method that helps diagnose angina pectoris. Also, do not forget about stress echocardiography, which allows you to clarify the diagnosis. Since angina pectoris manifests itself during physical activity, the method allows you to accurately determine the load threshold, the recovery period, and study the work of the heart after pain relief. Such diagnostics are carried out on a special bicycle ergometer and treadmill (treadmill). However, it is not suitable for everyone: stress tests are contraindicated in patients with acute angina.
Forms of angina pectoris
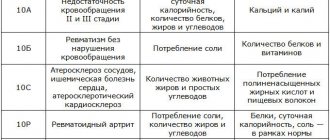
IHD exertional angina is divided into forms:
- First appeared. The diagnosis is made if no more than one month has passed since the attack. The course of the disease occurs in two variants - angina regresses (disappears) or becomes stable angina. The first signs of pathology may be harbingers of a heart attack.
- IHD stable angina pectoris. A persistent form of the disease with attacks lasting more than one month. It is characterized by the appearance of stereotypical symptoms in the patient under the load of one force.
- Progressive angina pectoris. Its development is indicated by an increase in severity and an increase in the duration and frequency of pain attacks when the body is exposed to normal stress.
Angina pectoris stage or otherwise functional classes (FC):
- 1 (first) FC. The usual load does not cause changes in well-being. Painful attacks occur against the background of excessive stress - after climbing several flights of stairs, while walking quickly.
- Second FC. The patient's physical activity is limited. An attack can be triggered by walking 500 meters or more, climbing 1-2 flights of stairs, walking in windy weather or frost, or psycho-emotional agitation.
- Third FC. The patient's physical activity is kept to a minimum. The attack appears after walking a distance of 100 meters, or when climbing one flight of stairs.
- Fourth FC. Physical activity is limited. A painful attack also occurs at rest.
Angina pectoris FC (functional classes) allows the doctor to correctly determine the amount of physical activity and select medications.
Pharmacological tests
Pharmacological tests are an alternative to stress tests and are recommended for patients who, for various reasons, cannot perform physical activity. The principle of their action is the introduction of special drugs, due to which the myocardial need for oxygen increases, thereby simulating activity. Depending on the drug, this need arises as a result of an increase in heart rate or redistribution of blood in favor of vessels not affected by atherosclerosis.
Treatment of angina pectoris
The patient's treatment plan is drawn up individually. First of all, standard therapy for coronary artery disease is prescribed using beta-blockers, antiplatelet agents, and drugs that reduce blood cholesterol.
During an attack, nitroglycerin helps relieve pain. For frequent episodes of exacerbation, prolonged (long-term) action nitrates are prescribed - Isosorbide mononitrate, Isosorbide dinitrate, nitroglycerin ointment or patch.
Complex therapy includes the elimination of all risk factors for the disease, diet therapy, and the choice of optimal physical activity.
Diagnosis of angina pectoris at the Center for Pathology of the Circulatory Organs
Today, instrumental diagnostics play a valuable role in monitoring the state of the cardiovascular system. Coronary heart disease cannot be completely cured and requires the patient to pay increased attention to his own body. Monitoring the condition using modern medical equipment allows you to correctly adjust therapy, thereby prolonging the patient’s life.
The Center for Pathology of the Circulatory Organs conducts a full range of studies of the cardiovascular system . Our experienced cardiologists work with the latest medical equipment, which allows us to detect the disease in the early stages, as well as diagnose asymptomatic forms of angina.
Specializing in non-surgical methods for diagnosing and treating heart disease, our doctors quickly, painlessly and, most importantly, completely safely carry out any procedure, make an accurate diagnosis and return you to a healthy and fulfilling life!
Do not put off health problems; the key to success in the treatment of coronary artery disease is its timely diagnosis!