Each muscle of the human body is equipped with arteries that supply it with all the necessary substances and oxygen. Their origin comes from the main vessel - the aorta. If a healthy person increases the load on his body, then the heart’s need for oxygen increases, and, consequently, the volume of blood flow through the vessels also increases. If cholesterol deposits have formed on the coronary arteries, then atherosclerotic plaques appear on their walls, reducing vascular patency. Thus, the free access of oxygenated blood to certain areas of the heart muscle is limited. This condition is defined as oxygen starvation. 30 minutes are enough, during which oxygen does not enter the heart, for the death of myocardial cells to occur. Pain during oxygen deprivation that occurs in the heart is called angina. If it appears during physical activity, it is considered angina pectoris.
General information about angina
An attack of angina develops when there is insufficient oxygen supply to the heart muscle cells. This occurs when the coronary vessels narrow and the myocardial oxygen demand increases. The attack can be triggered by physical activity, emotional stress, or going out into the cold. The pain goes away within a few minutes at rest or after taking nitroglycerin.
Under conditions of oxygen starvation, cells cannot efficiently process glucose into energy. Metabolic byproducts accumulate and “acidify” the tissues, causing severe pain. If blood flow is not restored in time, the myocardium dies and a heart attack develops.
Strazhesko-Vasilenko classification (with the participation of G. F. Lang)
Was
adopted at the XII Congress of Therapists of the USSR. Classification of CHF is carried out in 3 stages:
- Stage I - initial. It is characterized by the fact that hemodynamic disorders are compensated and are detected only with significant physical activity (domestic) or stress tests - treadmill, Master's test, bicycle ergometry (during diagnosis).
Clinical manifestations: shortness of breath, palpitations, fatigue at rest disappear;
- Stage II - severe heart failure. When it occurs, hemodynamics are disrupted (stagnation of blood in the circulatory system), the ability to work is sharply impaired, tissues and organs do not receive the required amount of oxygen. Symptoms occur at rest. It is divided into 2 periods - IIA and IIB. The difference between them: at stage A there is failure of either the left or right parts of the heart, when at stage B there is total heart failure - biventricular;
Stage IIA - characterized by stagnation in the pulmonary or systemic circulation.
At this stage of heart failure, in the first case, left ventricular failure occurs. It has the following clinical manifestations: complaints of shortness of breath, cough with the release of “rusty” sputum, suffocation (usually at night) as a manifestation of the so-called cardiac asthma.
When examining, pay attention to pallor, cyanosis of the extremities, tip of the nose, lips (acrocyanosis). There is no swelling. The liver is not enlarged. On auscultation, you can hear dry rales; with severe congestion, signs of pulmonary edema (fine-bubble rales).
When cardiac function is impaired with the development of stagnation of the systemic circulation, patients complain of heaviness in the right hypochondrium, thirst, swelling, abdominal distension, and indigestion.
There is cyanosis of the face, swelling of the veins of the neck, external edema (later - cavitary edema: ascites, hydrothorax), enlarged liver, heart rhythm disturbances. Treatment at this stage may be especially effective.
- How long can you live with stage 1 chronic heart failure?
Stage IIB - represents total heart failure with severe manifestations of circulatory failure. Combines symptoms of blood stasis BCC and MCC. This stage is very rarely reversible.
Stage III - final stage, heart failure in the decompensation stage. Deep myocardial degeneration occurs, irreversibly damaging both the heart itself and the organs experiencing ischemia and oxygen starvation due to its dysfunction. It is terminal and never undergoes regression.
Classification of angina pectoris
Depending on the relationship between attacks and physical activity, angina pectoris is classified as exertional or resting. The latter can occur without the influence of provoking factors, so it is more difficult to control.
Angina pectoris can be divided into two types: stable and progressive. In the first case, the frequency and strength of attacks depends on the amount of physical activity; they are easily eliminated with the help of drug therapy. Progressive angina pectoris practically cannot be corrected with pharmaceutical drugs; the frequency of attacks increases over time.
The following functional classes of stable angina are distinguished:
- Pain appears only with intense or prolonged physical activity.
- The onset of an attack when walking more than 200 m or climbing more than one flight of stairs at a normal pace. With severe emotional stress.
- Pain when walking less than 200 meters or climbing one flight of stairs at a leisurely pace.
- Seizures occur with minor physical exertion or at rest.
There is Prinzmetal's angina or spontaneous (special, vasospastic) angina - caused by a sudden spasm of the coronary arteries. Attacks develop only at rest, at night or early in the morning.
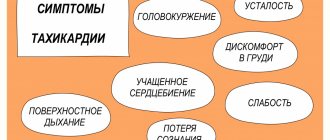
Symptoms
Regardless of the class of angina pectoris, it has common symptoms that range from slight discomfort in the chest to intense pain in the heart, which increases over time. A classic attack of angina has a clear beginning and end. It can stop if you complete physical activity and take an ester of glycerin and nitric acid (nitroglycerin). Pain can be localized in different places:
- behind the sternum;
- on the left side of the chest;
- give to the left arm, shoulder blade, jaw or neck.
The nature of the sensations can also be:
- pressing;
- contracting.
And by intensity: high and moderate. Accompanying factors of angina pectoris are a feeling of lack of air, shortness of breath, interruptions in heart rate, cold sweat and fear of death. Important! Interesting fact: angina pectoris does not always manifest itself as pain; sometimes it can be a cough, sudden unexplained weakness, or shortness of breath.
In cases where the pain is wave-like, too intense, and cannot be controlled by taking appropriate medications, you must call an ambulance. These symptoms may indicate the development of myocardial infarction.
Risk factors for developing angina
The following factors lead to narrowing of the coronary vessels and insufficient blood supply to the myocardium:
- atherosclerosis - deposition of cholesterol plaques in the walls of blood vessels;
- hypotension ー low blood pressure;
- coronary artery thrombosis;
- age-related changes in blood vessels.
In the vast majority of cases, angina is caused by atherosclerotic lesions of the coronary arteries. It develops due to disturbances in the metabolism of cholesterol and other lipids: excess animal fats in the diet, lack of plant foods. Therefore, proper nutrition is the basis for successful prevention of angina pectoris.
Nicotine also constricts blood vessels, so smokers develop angina more often.
The risk group for the development of angina pectoris includes:
- people over 55 years of age;
- men;
- smokers;
- people who abuse alcohol and drugs;
- people with pathologies of the cardiovascular system (heart defects, heart failure);
- with pathologies of the respiratory system (bronchial asthma, chronic obstructive diseases);
- overweight.
All these factors increase the risk of developing atherosclerosis, cardiac ischemia and angina. Most of them can be eliminated through lifestyle changes.
Angina pectoris 4 FC
4 FC of angina is the most difficult, because a painful attack in this case often occurs without obvious reasons (angina at rest). Any minor load can provoke an attack. In this functional class, the patient’s medical history may already include myocardial infarction or cardiovascular failure. Against the background of a recent heart attack, attacks are especially dangerous - with early post-infarction angina, they occur spontaneously and can lead to a second heart attack.
If a person has difficulty walking, shortness of breath, or pain in the sternum that does not go away within 15 minutes, it is necessary to urgently call the Ambulance Service, because in this case we may be talking about acute coronary syndrome and the patient requires treatment and observation in a hospital.
Diagnosis of angina pectoris
Angina pectoris has a fairly typical clinical picture, so it will not be difficult for a therapist and cardiologist with experience to recognize it. To find out the cause of the attacks and determine possible treatment tactics, specialists at the Paracelsus Medical Center recommend undergoing the following examination:
- general and biochemical blood test (cholesterol and other lipid levels);
- ECG at rest and during exercise;
- echocardiography (Echo-CG);
- coronary angiography ー examination of the heart vessels using a contrast agent;
- Holter monitoring - recording of electrical impulses of the heart for 24 hours (the patient adheres to his usual routine).
Angina pectoris 3 FC
Angina pectoris FC 3, in contrast to functional classes 1 and 2, involves significant restrictions on physical activity, since at this stage an attack can occur when moving at a normal pace or when climbing stairs just one flight. Sometimes an attack can be triggered by hypothermia or excessive eating or smoking. Very rarely in this functional class is angina at rest, which occurs during a supine position or severe anxiety.
In this case, treatment of angina pectoris is carried out as part of the treatment of coronary artery disease. It includes taking medications that lower cholesterol and thin the blood. In addition, the patient is prescribed medications that relieve pain and normalize blood pressure. However, if angina pectoris type 3 becomes unstable, pain syndromes become more frequent and last longer, then a decision is made about surgical intervention.
Forecast and prevention of angina pectoris
The basis for preventing angina pectoris is proper nutrition and exercise. The diet should consist of proteins, vegetable fats, and complex carbohydrates. The consumption of alcohol and trans fats (fast food) should be avoided. Give preference to white meat, fish and seafood.
Regular physical activity should be present in the life of every person, this could be swimming, team sports, fitness, running or just walking. Its intensity is determined by the person’s health status; if you have chronic diseases, you should consult your doctor about the types of physical activity acceptable to you.
If you follow all the doctor’s recommendations, angina pectoris can be controlled, but, unfortunately, most patients ignore lifestyle instructions, which can lead to a worsening of the condition.
Angina pectoris 1 FC
With 1 FC of exertional angina, the patient copes well with normal daily activity. Activities such as vigorous walking and climbing stairs do not cause an angina attack in the patient. It is quite rare for people with this functional class to go to the hospital, since the person may not even know about the presence of the disease. As a rule, symptoms of angina pectoris appear when performing fairly intense exercises, very fast and long runs, and loads that are unusual for an ordinary person. To diagnose angina pectoris FC1, it is necessary to use the bicycle ergometer test method.
Diagnosis and treatment of angina pectoris at the Paracelsus Medical Center
When should you see a doctor?
The characteristic posture of a patient with an attack of angina pectoris: he stops abruptly, leans forward, with his right fist pressed to his chest.
If such attacks occur, as well as pain and discomfort in the heart area, it is necessary to consult a general practitioner or cardiologist for a detailed examination and selection of drug therapy.
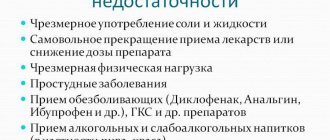
First of all, the patient is recommended to make lifestyle adjustments:
- quitting smoking, alcohol, drugs;
- normalization of nutrition (reducing the percentage of animal fats, sugar, flour products, increasing the proportion of plant foods, fish);
- optimal mode of physical activity;
- treatment of concomitant diseases.
Drug treatment
To eliminate attacks of pain, nitrates, calcium channel blockers, and anticoagulants are prescribed.
Attention!
Medicines should be taken only on the recommendation of a doctor. Dosages are selected individually, taking into account the characteristics of the patient.
Nitrates cannot be combined with drugs used to treat sexual dysfunction (Viagra, Tadafil, etc.).