Early ventricular repolarization syndrome - what is it? General information
Specific cardiac syndrome is found not only in patients with heart pathology, but also in absolutely healthy people. Early repolarization of the ventricles is called premature repolarization syndrome. Very often, WPW syndrome confused with premature repolarization, despite the fact that these are completely different pathologies.
Pathological changes on the ECG were considered normal for a long time, until a clear relationship with heart rhythm disturbances was revealed. The disease is asymptomatic, which greatly complicates timely diagnosis.
The syndrome of early (premature, accelerated) repolarization of the ventricles of the heart is characterized by specific changes in the electrocardiogram in the absence of obvious causes. ICD-10 code: I45.6
Treatment of early ventricular repolarization syndrome
Repolarization syndrome does not require specific treatment. The only thing that is offered to the patient is observation by a cardiologist.
However, a person with SRS should avoid alcohol consumption and intense physical activity to avoid triggering an attack of tachycardia.
In some cases, radiofrequency ablation of an additional beam is performed in an invasive way (a catheter is brought to the site of the beam and destroys it).
Sometimes energotropic therapy (B vitamins, carnitine, phosphorus and magnesium preparations, Mexidol, Kudesan), antiarrhythmic drugs (amiodarone) are used.
Important! The patient should retain all previous ECGs, which is required to exclude the diagnosis of myocardial infarction if heart pain occurs.
Pathogenesis
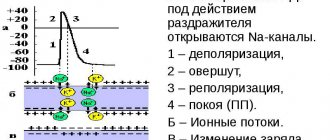
Contraction of the chambers of the heart occurs as a result of changes in the electrical charge in myocardial cells - cardiomyocytes . As a result, sodium, calcium and potassium ions move into the intercellular space and back. The process is carried out in alternating main phases:
- depolarization – contraction;
- repolarization is relaxation before a new contraction.
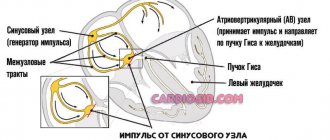
Early repolarization of the ventricles is formed as a result of improper conduction of the impulse through the conduction system of the heart from the atria to the ventricles. To transmit the electrical impulse, abnormal conduction pathways . The development of the phenomenon is due to an imbalance between repolarization and depolarization in the basal regions and apex of the heart. Characterized by a significant reduction in the period of myocardial relaxation. On the ECG, along with the SRRS, a disturbance of repolarization processes in the myocardium is often recorded, in particular, a violation of the repolarization of the lower wall of the left ventricle.
Depolarization and repolarization
The section "Basic principles of electrocardiography and disorders" discusses the general concept of "electrical excitation" , which means the propagation of electrical impulses through the atria and ventricles. The exact name for electrical excitation, or activation of the heart, is depolarization . The return of cardiomyocytes to a state of relaxation after excitation (depolarization) is repolarization . These terms emphasize that at rest, the myocardial cells of the atria and ventricles are polarized (their surface is electrically charged). Figure 2-1, A shows the state of polarization of a normal muscle cell of the atria or ventricles
Rice. 2-1. Processes of depolarization and repolarization A - the muscle cell of the heart is polarized at rest, i.e. the outer surface of the cell is positively charged, and the inner surface is negatively charged; B - when a cell (S) is excited, it depolarizes (the excited area is electronegative with respect to neighboring areas); B – a completely depolarized cell is charged positively inside and negatively outside; D – repolarization occurs when a cell returns from a state of excitation to a state of rest. The direction of depolarization and repolarization is indicated by arrows. Depolarization (excitation) of the atria on the ECG corresponds to the P wave, and depolarization of the ventricles corresponds to the QRS complex. Ventricular repolarization corresponds to the ST-T complex.
The outside of the cell at rest is positively , and the inside is negatively charged [about -90 mV (millivolts)]. Membrane polarization is caused by the difference in ion concentrations inside and outside the cell.
When the muscle cell of the heart is excited, it depolarizes. As a result, the outer side of the cell in the region of excitation becomes negative, and the inner side becomes positive. There is a difference in electrical voltage on the outer surface of the membrane between the depolarized area in the state of excitation and the unexcited polarized area, see Fig. 2-1, B. Then a small electric current arises, which spreads along the cell until it is completely depolarized, see fig. 2-1, V.
The direction of depolarization is shown by an arrow, see Fig. 2-1, B. Depolarization and repolarization of individual muscle cells (fibers) occurs in one direction. However, throughout the myocardium, depolarization proceeds from the inner layer (endocardial) to the outermost layer (epicardial), and repolarization occurs in the opposite direction. The mechanism for this difference is not completely clear .
| Note: Depolarization of the ventricular myocardium occurs from the endocardium to the epicardium, and repolarization occurs from the epicardium to the endocardium. This is due to the fact that the duration of TMPD in the subepicardial parts of the ventricles is 0.03-0.04 s less than in the subendocardial parts, and the repolarization process will begin earlier precisely under the epicardium. | |
The depolarizing electric current is recorded on the electrocardiogram in the form of the P wave (excitation and depolarization of the atria) and the QRS complex (excitation and depolarization of the ventricles).
After some time, the depolarized cell, completely engulfed in excitation, begins to return to a resting state. This process is called repolarization . A small area on the outside of the cell again acquires a positive charge, see fig. 2-1, D, then the process spreads along the cell until it is completely repolarized. Ventricular repolarization on the electrocardiogram corresponds to the ST segment, waves and (atrial repolarization is usually hidden by ventricular potentials).
An electrocardiogram shows the electrical activity of all cells in the atria and ventricles, rather than individual cells. In the heart, depolarization and repolarization are usually synchronized, so on the electrocardiogram these electrical flows can be recorded in the form of certain waves ( P , T , U , QRS complex , ST segment ).
| Any electrocardiogram - both normal and pathologically altered - reflects two main processes: depolarization - the propagation of an impulse throughout the myocardium - and repolarization - the return of the excited myocardium to a resting state. | |
Classification
In children and adults, early ventricular repolarization syndrome can have 2 development options:
- without damage to the cardiovascular system;
- with defeat.
According to the nature of the flow, they are distinguished:
- transitory form;
- permanent form.
Depending on the location of the ECG signs of SRGC, they are divided into 3 types.
- I characteristic signs are observed in a healthy person. ECG signs are recorded only in chest leads V1, V2. The likelihood of complications developing is extremely low.
- II ECG signs are recorded in the inferolateral and lower sections, leads V4-V6. The risk of complications is increased.
- III ECG changes are recorded in all leads. The risk of complications is the highest.
Diagnostics
Since this syndrome is an electrocardiographic phenomenon, it can only be established with a certain examination:
- ECG;
- Ultrasound of the heart (echocardiography): stress echocardiography (for impaired ventricular contractility)
- resting echocardiography;
In addition, tests are carried out on a bicycle ergometer or treadmill: after physical activity, the heart rate increases, and the ECG signs of SIRS disappear.
A potassium test is used: after taking potassium chloride, panangin or rhythmocor at least 2 grams, the severity of ECG signs of repolarization syndrome increases.
A test with isoproterenol and atropine is not used due to severe side effects.
It is important to distinguish between SRR and myocardial infarction, pericarditis, Brugada syndrome. For this purpose, differential diagnosis is carried out.
Causes
The true reasons have not been fully studied. There are only hypotheses for the occurrence of early repolarization:
- Genetic predisposition. Mutation of genes that are responsible for balancing the processes of the entry of certain ions into the cell and their release out.
- Disruption of the processes of contraction and relaxation of individual areas of the myocardium, which is characteristic of type I Brugada syndrome .
- Changes in cardiomyocyte action potentials. The process is associated with the mechanism for the release of potassium ions from cells. This also includes increased susceptibility to a heart attack during ischemia .
According to statistics, accelerated repolarization syndrome is typical for 3-10% of healthy people of all ages. Most often, changes are recorded in young people aged 30 years, in people leading a healthy lifestyle and in athletes.
Nonspecific factors influencing the development of early ventricular repolarization syndrome:
- congenital form of hyperlipidemia , which provokes the development of atherosclerotic changes ;
- long-term use of certain medications, or overdose (for example, beta-agonists);
- connective tissue dysplasia , which is characterized by additional chordae in the ventricular cavity;
- high blood cholesterol
- electrolyte imbalance;
- neuroendocrine changes;
- hypertrophic cardiomyopathy;
- heart defects : congenital, acquired;
- disturbances in the functioning of the autonomic nervous system;
- hypothermia of the body;
- excessive physical activity.
Syndrome of premature excitation of ventricles.
Heart rhythm disturbances are considered an important cardiac problem, since they often complicate the course and worsen the prognosis of many diseases and are one of the most common causes of sudden death.
Of particular interest to both clinicians and electrophysiologists is premature ventricular excitation syndrome (PVS), which in some cases, in the absence of clinical manifestations, can be an electrocardiographic finding, and in others it can be accompanied by life-threatening tachyarrhythmias.
Despite the successes achieved in the study of PPV, the issues of its diagnosis, patient management and treatment remain relevant today.
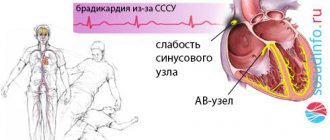
Definition. Classification
PPV (preexcitation syndrome, preexcitation syndrome) is an accelerated conduction of the excitation impulse from the atria to the ventricles along additional abnormal conduction pathways. As a result, part of the myocardium or all of the ventricular myocardium begins to be excited earlier than with the usual spread of excitation through the atrioventricular node, the His bundle and its branches.
According to the recommendations of the WHO expert group (1980), premature excitation of the ventricles, not accompanied by clinical symptoms, is called the “pre-excitation phenomenon,” and in the case when there are not only electrocardiographic signs of pre-excitation, but also tachyari paroxysms develop.
The anatomical substrate of PVS are bundles of specialized muscle fibers outside the conduction system of the heart, capable of conducting electrical impulses to different parts of the myocardium, causing their premature excitation and contraction.
Accessory atrioventricular connections are classified according to their location relative to the annulus fibrosus of the mitral or tricuspid valves, type of conduction (decremental type - increasing slowing of conduction along the accessory pathway in response to an increase in the frequency of stimulation - or non-decremental), and also according to their ability to antegrade, retrograde or combined implementation. Typically, accessory pathways have rapid, nondecremental conduction similar to that of normal tissue of the His–Purkinje conduction system and atrial and ventricular myocardium.
Currently, several types of abnormal pathways (tracts) are known:
- atrioventricular (Kenta), connecting the myocardium of the atria and ventricles, bypassing the atrioventricular node;
- atrionodal (James), located between the sinoatrial node and the lower part of the atrioventricular node;
- nodoventricular (Maheima), connecting the atrioventricular node (or the beginning of the His bundle) with the right side of the interventricular septum or the branches of the right bundle branch;
- atriofascicular (Breschenmash), connecting the right atrium with the common trunk of the His bundle.
There are also other additional conduction pathways, including “hidden” ones, capable of conducting an electrical impulse retrogradely from the ventricles to the atria. A small (5–10%) proportion of patients have multiple abnormal conduction pathways.
In clinical practice there are:
- Wolff–Parkinson–White syndrome (WPW syndrome), caused by the presence of bundles of Kent;
- Clerk-Levy-Christesco syndrome (CLC syndrome, shortened P-Q (R) interval syndrome), caused by the presence of the James bundle.
Electrocardiographic manifestations of PPV depend on the degree of preexcitation and the persistence of conduction along additional pathways. In this regard, the following variants of the syndrome are distinguished:
- manifest PPV (the ECG constantly shows signs of pre-excitation);
- intermittent (transient) PPV (on the ECG, signs of pre-excitation are transient);
- latent PPV (the ECG is normal under normal conditions, signs of pre-excitation appear only during a paroxysm of tachycardia or during provocation - physical activity, electrophysiological study (EPI), vagal or drug tests);
- hidden (changes are not detected on a standard ECG due to the conduction of excitation along additional pathways only in a retrograde manner).
Prevalence
According to various sources, the prevalence of PPV in the general population is approximately 0.15%. At the same time, paroxysms of tachyarrhythmias occur in every second patient (in 80–85% of cases – orthodromic tachycardia, 20–30% – atrial fibrillation (AF), 5–10% – atrial flutter and antidromic tachycardia). Hidden PPV is detected in 30–35% of patients.
PPV is a congenital anomaly, but can clinically manifest at any age, spontaneously or after any disease. Typically, this syndrome manifests itself at a young age. In most cases, patients do not have any other heart pathology. However, combinations of PPV with Ebstein's anomaly, cardiomyopathies, and mitral valve prolapse are described. There is an assumption that there is a relationship between PVS and connective tissue dysplasia.
In families of patients suffering from this syndrome, an autosomal dominant type of inheritance of additional pathways was identified in relatives of the 1st, 2nd, and 3rd degrees of kinship with various clinical and electrocardiographic manifestations.
The incidence of sudden death in patients with PPV is 0.15–0.6% per year. In almost half of the cases, cardiac arrest in persons with PPV is its first manifestation.
Studies of patients with PPV who have suffered cardiac arrest have retrospectively identified a number of criteria that can be used to identify individuals at increased risk of sudden death. These include the presence of the following signs:
- shortened RR interval – less than 250 ms during spontaneous or induced AF;
- history of symptomatic (hemodynamically significant) tachycardia;
- multiple additional paths;
- Ebstein's anomalies.
Story
An ECG with a shortened PQ interval and at the same time a widened QRS complex was first described by A. Cohn and F. Fraser in 1913. Isolated similar cases were subsequently described by some other authors, but for many years the cause of this ECG pattern was considered to be blockade of the branches of the His bundle.
In 1930, L. Wolff, J. Parkinson and P. White presented a report in which electrocardiographic changes of this type were considered as the cause of paroxysmal cardiac arrhythmias. This work provided the basis for conducting comprehensive studies aimed at elucidating the pathogenesis of these changes on the ECG, which were subsequently named Wolff-Parkinson-White syndrome.
Two years later, M. Holzman and D. Scherf suggested that the basis of WPW syndrome is the spread of the excitation impulse along additional atrioventricular pathways. In 1942, F. Wood provided the first histological confirmation of the presence of a muscular connection between the right atrium and the right ventricle, identified during autopsy of a 16-year-old patient with a history of episodes of paroxysmal tachycardia.
Despite these data, an active search for alternative mechanisms for the development of the syndrome continued until the 1970s, when EPI and surgical treatments confirmed the theory of accessory pathways.
Pathogenesis
The conduction of impulses from the atria to the ventricles during PPV occurs simultaneously along the normal conduction system of the heart and along the accessory pathway. In the conduction system at the level of the atrioventricular node, there is always some slowdown in the conduction of impulses, which is not typical for the anomalous tract. As a result, depolarization of a certain area of the ventricular myocardium begins prematurely even before the impulse propagates through the normal conduction system.
The degree of preexcitation depends on the ratio of conduction velocities in the normal conduction system of the heart, primarily in the atrioventricular node, and in the accessory conduction pathway. An increase in the conduction velocity along the accessory pathway or a slowdown in the conduction velocity through the atrioventricular node leads to an increase in the degree of ventricular preexcitation. In some cases, ventricular depolarization may be entirely due to the conduction of impulses along the accessory pathway. At the same time, when the conduction of impulses through the atrioventricular node accelerates or the conduction through the accessory pathway slows down, the degree of abnormal ventricular depolarization decreases.
The main clinical significance of additional conduction pathways is that they are often included in the loop of circular motion of the excitation wave (re-entry) and thus contribute to the occurrence of supraventricular paroxysmal tachyarrhythmias.
With PPV, orthodromic reciprocal supraventricular tachycardia most often occurs, in which the impulse is conducted antegrade through the atrioventricular node, and retrograde through the accessory pathway. Paroxysm of orthodromic supraventricular tachycardia is characterized by frequent (140–250 per 1 min), devoid of signs of preexcitation, normal (narrow) QRS complexes. In some cases, inverted P waves are observed after the QRS complex, indicating retrograde activation of the atria.
With antidromic supraventricular tachycardia, the impulse circulates in the opposite direction: antegrade - along the abnormal conduction pathway, retrograde - along the atrioventricular node. Paroxysm of antidromic supraventricular tachycardia in patients with PPV is manifested on the ECG by a frequent regular rhythm (150–200 per 1 min) with ventricular complexes of the type of maximally pronounced preexcitation (QRS = 0.11 s), after which inverted P waves are sometimes detected.
In 20–30% of patients with PPV, paroxysms of AF occur, in which, as a result of antegrade conduction of a large number of atrial impulses along the accessory pathway, the ventricular contraction frequency (VFR) can exceed 300 per minute.
Clinic
In many cases, PPV is asymptomatic and is detected only by electrocardiography. 50–60% of patients complain of palpitations, shortness of breath, chest pain or discomfort, fear and fainting. Paroxysms of AF become particularly dangerous in the case of PPV, since they are accompanied by a large heart rate, hemodynamic disturbances, and can often transform into ventricular fibrillation. In such cases, patients not only experience syncope, but also have a high risk of sudden death.
Independent risk factors for the development of AF in patients with PPV are age, male gender, and a history of syncope.
Diagnostics
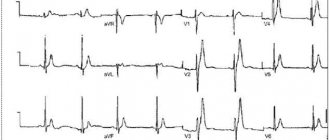
The main method for diagnosing PPV is ECG.
In case of WPW syndrome against the background of sinus rhythm, a shortening of the PQ interval (<0.12 s) and a D-wave (flat slope in the first 30–50 ms) are detected on the ascending part of the R wave or the descending part of the Q wave, the QRS complex is usually widened (i0, 11 s). Deviation of the ST segment and T wave in the direction opposite to the D-wave and the main direction of the QRS complex is also characteristic.
Electrocardiographic signs of CLC syndrome are shortening of the PQ (R) interval, the duration of which does not exceed 0.11 s, the absence of an additional excitation wave - D-wave - in the QRS complex, the presence of unchanged (narrow) and undeformed QRS complexes (except in cases of concomitant blockade of the legs or branches of the His bundle).
With PPV, caused by the functioning of the Maheim beam, a normal PQ interval is determined in the presence of a D wave.
The simultaneous functioning of the James and Maheim beams leads to the appearance on the ECG of signs characteristic of WPW syndrome (shortening of the PQ (R) interval and the presence of a D-wave).
In connection with the spread in recent years of surgical methods for the treatment of patients with PPV (destruction of an abnormal bundle), methods for accurately determining its localization are constantly being improved.
On the ECG, the location of the Kent beam is usually determined by the direction of the initial moment vector of ventricular depolarization (the first 0.02–0.04 s), which corresponds to the time of formation of the abnormal D-wave. In those leads whose active electrodes are located directly above the area of the myocardium that is abnormally excited by the Kent beam, a negative D-wave is recorded. This indicates the spread of early abnormal excitation away from the active electrode of this lead.
Of particular practical interest are the capabilities of the spatial vector electrocardiography method, which makes it possible to accurately determine the localization of additional conduction pathways.
More detailed, compared to ECG data, information about the location of additional conduction pathways can be obtained using magnetocardiography.
However, the most reliable and accurate methods are intracardiac EPI, in particular endocardial (preoperative) and epicardial (intraoperative) mapping. In this case, using a complex technique, the area of the earliest activation (pre-excitation) of the ventricular myocardium is determined, which corresponds to the localization of the additional abnormal bundle.
Treatment
In patients with asymptomatic PPV, treatment is usually not required. Exceptions include individuals with a family history of sudden death, athletes, and those whose work involves danger to themselves and others (for example, divers and pilots).
In the presence of paroxysms of supraventricular tachycardia, treatment consists of stopping attacks and preventing them using various medicinal and non-medicinal methods. In this case, the nature of the arrhythmia (ortho-, antidromic tachycardia, AF), its subjective and objective tolerability, heart rate, as well as the presence of concomitant organic heart diseases are important.
With orthodromic reciprocal supraventricular tachycardia, the excitation impulse is conducted antegrade in the normal way, so its treatment should be aimed at suppressing conduction and blocking impulses in the atrioventricular node. For this purpose, reflex vagal tests are used, which are most effective when applied as early as possible.
The first-line drug for stopping orthodromic reciprocal supraventricular tachycardia is considered to be adenosine, the potential disadvantage of which is a transient increase in atrial excitability, which can provoke their extrasystole and fibrillation immediately after stopping the paroxysm of such tachycardia. Verapamil is considered to be another drug of choice for stopping orthodromic tachycardia in the absence of severe arterial hypotension and severe systolic heart failure. β-blockers are usually used as second-line drugs.
If these drugs are ineffective, procainamide is used to block conduction through the accessory atrioventricular pathway. Due to its safety and effectiveness, novocainamide is the drug of choice in the treatment of tachycardia with wide QRS complexes, when the diagnosis of orthodromic reciprocal supraventricular tachycardia is in doubt.
Reserve drugs are amiodarone, sotalol and class 1C antiarrhythmic drugs (AAPs): propafenone or flecainide.
In case of antidromic reciprocal supraventricular tachycardia, the impulse is conducted retrogradely through the atrioventricular node, therefore the use of verapamil, diltiazem, lidocaine and cardiac glycosides for its relief is contraindicated due to the ability of these drugs to accelerate antegrade conduction along the accessory pathway and thereby increase heart rate. The use of these drugs, as well as adenosine, can provoke the transition of antidromic supraventricular tachycardia to AF. The drug of choice for stopping such tachycardia is procainamide; if it is ineffective, amiodarone or class 1C AAP are used.
When paroxysmal AF occurs, the main goal of drug therapy is to control the ventricular rate and slow down conduction simultaneously along the accessory tract and the AV node. The drug of choice in such cases is also novocainamide. Intravenous administration of amiodarone and class 1C AAP is also highly effective.
It should be noted that the use of verapamil, digoxin and beta-blockers in AF for the purpose of controlling heart rate in persons with PPV is contraindicated due to their ability to increase the conduction velocity along the accessory pathway. This can transfer fibrillation from the atria to the ventricles.
To prevent paroxysms of supraventricular tachyarrhythmias caused by the presence of additional conduction pathways, class IA, IC and III AAPs are used, which have the property of slowing down conduction along abnormal pathways.
Non-drug methods for stopping attacks of supraventricular tachyarrhythmias include transthoracic depolarization and atrial (transesophageal or endocardial) pacing, and for their prevention - catheter or surgical ablation of accessory pathways.
In patients with PPV, electrical cardioversion is used for all forms of tachycardia, which are accompanied by severe hemodynamic disturbances, as well as when drug therapy is ineffective and in cases where it causes a deterioration in the patient's condition.
Radiofrequency catheter ablation of accessory tracts is currently the main method of radical treatment of PPV. Indications for its implementation are a high risk of sudden death (primarily the presence of AF paroxysms), ineffectiveness or poor tolerability of drug therapy and prevention of attacks of supraventricular tachycardia, as well as the patient’s reluctance to take AAP. If a short effective refractory period of the abnormal tract is detected in individuals with rare and mild paroxysms of arrhythmia, the question of the advisability of ablation in order to prevent sudden death is decided individually.
Before catheter ablation, EPI is performed, the purpose of which is to confirm the presence of an additional conduction pathway, determine its electrophysiological characteristics and role in the formation of tachyarrhythmia.
The effectiveness of radiofrequency catheter ablation is high (reaches 95%), and the mortality associated with the procedure does not exceed 0.2%. The most common serious complications of this treatment method are complete atrioventricular block and cardiac tamponade. Recurrences of conduction along the accessory pathway occur in approximately 5–8% of cases. Repeated radiofrequency ablation usually completely eliminates conduction along additional pathways.
Currently, the scope of surgical destruction of accessory tracts has significantly narrowed. For the same indications as catheter ablation, surgical treatment is resorted to in cases where the latter is impossible to perform for technical reasons or is unsuccessful, as well as when open-heart surgery is necessary due to concomitant pathology.
Literature
- Sychev O.S. Heart rhythm disturbances // Guide to cardiology / Ed. V.N. Kovalenko. – K.: Morion, 2008. – P. 1059-1248, 1215-1218.
- ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation // Circulation. – 2006. – No. 114. – P. 257-354.
- ACC/AHA/ESC Guidelines for the management of patients with supraventricular arrhythmias – executive summary // JACC. – 2003. – No. 8. – R. 1493-1531.
- Griffin B., Topol E. Manual of Cardiovascular Medicine. – The Lippincott Williams & Wilkins, 2004. – P. 1248.
- Hanon S., Shapiro M., Schweitzer P. Early history of the preexcitation syndrome // Europace. – 2005. – No. 7. – P. 28-33.
- Keating L., Morris A., Brady W.O. Electocardiographic Features of Wolff–Parkinson–White syndrome // Emerg. Med. J. – 2003. – No. 20. – R.491-493.
N.T. Vatutin, N.V. Kalinkina, E.V. Yeshchenko.
Donetsk State Medical University. M. Gorky;
Institute of Emergency and Reconstructive Surgery named after. VC. Gusak of the Academy of Medical Sciences of Ukraine.
Ukrkardio
Symptoms
Clinical symptoms are observed only in the form of the disease that is accompanied by disturbances in the functioning of the cardiovascular system:
- loss of consciousness, fainting ;
- rhythm disturbances ( tachyarrhythmia , extrasystole , ventricular fibrillation );
- vagotonic, hyperamphotonic, tachycardial, dystrophic are formed under the influence of humoral factors on the hypothalamic-pituitary system;
- systolic and diastolic dysfunction of the heart caused by its hemodynamic disorders ( pulmonary edema , hypertensive crisis , shortness of breath , cardiogenic shock ).
Tests and diagnostics
The main changes are recorded precisely on the electrocardiogram. Some patients simultaneously experience clinical symptoms of cardiovascular diseases, but most often patients feel absolutely healthy and do not notice any changes.
Early ventricular reoplarization syndrome on ECG:
- elevation of the ST segment above the isoline;
- the convexity when raising the ST segment is directed downwards;
- an increase in the R wave with a parallel decrease in the S wave or its complete disappearance;
- point J is located above the isoline, at the level of the descending knee of the R wave;
- expansion of the QRS complex on the ECG;
- a “notch” is recorded on the descending limb of the R wave.
Early ventricular repolarization syndrome in children
The reasons for the development of early repolarization syndrome in children can be very different:
- lack of sleep and irregular daily routine;
- excessive emotional stress;
- physical overload;
- constant anxiety, stress or nervous fatigue;
- isolation, lack of healthy emotional contact with parents;
- hypothermia;
- poor quality and unbalanced nutrition.
A similar syndrome can be recorded on an ECG in any child who reacts too emotionally to the assessment of his knowledge at school, takes current events to heart, and is overloaded in extracurricular activities. Lack of proper rest and intensive training in sports clubs can negatively affect the child’s well-being.
Forecast. What is the danger of early ventricular repolarization syndrome?
Modern cardiologists work to prevent and prevent the development of pathology, which can lead to death. That is why patients with early ventricular repolarization syndrome should be regularly monitored by a cardiologist to monitor the dynamics of the ECG and to identify hidden symptoms of other pathologies. It is not the syndrome itself that is dangerous, but the consequences it can lead to in the absence of proper treatment of the causative disease.
Persons who play sports are recommended to undergo examination at specialized physical education clinics, assessing their condition before and after intensive training, as well as before competitions.
There is no clear data on the transition of SRGC to a serious pathology. The risk of death increases significantly with alcoholism , abuse of fatty foods and smoking. A timely and complete competent examination will help to identify or exclude the true cause and avoid problems in the future.