CC dossier
Savely Barger (MOSCOW),
cardiologist, candidate of medical sciences. In the 1980s, he was one of the first scientists in the USSR to develop a technique for diagnostic transesophageal cardiac pacing. Author of manuals on cardiology and electrocardiography. He is the author of several popular books devoted to various problems of modern medicine.
It is safe to say that beta-blockers are first-line drugs for the treatment of many diseases of the cardiovascular system.
Here are some clinical examples.
Patient B., 60 years old, suffered an acute myocardial infarction 4 years ago. Currently, he is bothered by characteristic compressive pain behind the sternum during light physical exertion (with a slow pace of walking he can walk no more than 1000 meters without pain). Along with other medications, he receives bisoprolol 5 mg morning and evening.
Patient R., 35 years old. At the appointment, he complains of constant headaches in the occipital region. Blood pressure 180/105 mm Hg. Art. Treatment with bisoprolol is carried out at a daily dosage of 5 mg.
Patient L., 42 years old, complained of interruptions in the work of the heart, a feeling of “fading” of the heart. During daily ECG recording, frequent ventricular extrasystoles and episodes of “jogs” of ventricular tachycardia were diagnosed. Treatment: sotalol 40 mg twice daily.
Patient S., 57 years old, suffers from shortness of breath at rest, attacks of cardiac asthma, decreased performance, and swelling in the lower extremities, which worsens in the evening. Ultrasound examination of the heart revealed diastolic dysfunction of the left ventricle. Therapy: metoprolol 100 mg twice a day.
In such diverse patients: coronary heart disease, hypertension, paroxysmal ventricular tachycardia, heart failure - drug treatment is carried out with drugs of the same class - beta-blockers.
Beta-adrenergic receptors and mechanisms of action of beta blockers
There are beta1-adrenergic receptors located mainly in the heart, intestines, kidney tissue, adipose tissue, and to a limited extent in the bronchi. Beta2-adrenergic receptors are found in the smooth muscles of blood vessels and bronchi, in the gastrointestinal tract, in the pancreas, and to a limited extent in the heart and coronary vessels. No tissue contains exclusively beta1 or beta2 adrenergic receptors. In the heart, the ratio of beta1- and beta2-adrenergic receptors is approximately 7:3.
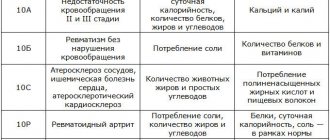
Table 1. Main indications for the use of beta-blockers
The mechanism of action of beta blockers is based on their structure, similar to catecholamines. Beta blockers act as competitive antagonists of catecholamines (adrenaline and norepinephrine). The therapeutic effect depends on the ratio of the concentration of the drug and catecholamines in the blood.
Blockade of beta1-adrenergic receptors leads to a decrease in heart rate, contractility and contraction speed of the heart muscle, while the myocardial oxygen demand decreases.
- Beta blockers cause depression of the 4th phase of diastolic depolarization of cells of the cardiac conduction system, which determines their antiarrhythmic effect. Beta blockers reduce the flow of impulses through the atrioventricular node and reduce the speed of impulses.
- Beta blockers reduce the activity of the renin-angiotensin system by reducing the release of renin from juxtaglomerular cells.
- Beta blockers affect the sympathetic activity of vasoconstrictor nerves. Prescription of beta blockers without intrinsic sympathomimetic activity leads to a decrease in cardiac output, peripheral resistance increases, but returns to normal with long-term use.
- Beta blockers inhibit catecholamine-induced cardiomyocyte apoptosis.
- Beta blockers stimulate the endothelial arginine/nitroxide system in endothelial cells, i.e., they turn on the main biochemical mechanism for dilation of vascular capillaries.
- Beta blockers block some calcium channels in cells and reduce calcium levels in heart muscle cells. This is probably due to a decrease in the strength of heart contractions and a negative inotropic effect.
Non-cardiological indications for the use of beta blockers
- anxiety states
- delirium delirium
- juxtaglomerular hyperplasia
- insulinoma
- glaucoma
- migraine (attack prevention)
- narcolepsy
- thyrotoxicosis (treatment of rhythm disturbances)
- portal hypertension
Table 2. Properties of beta-blockers: beneficial and side effects, contraindications
History of discovery
In 1948, the American Raymond Ahlquist established the importance of the participation of norepinephrine in the transmission of nerve impulses. By this time, two types of adrenergic receptors were also known: alpha, which are most often present in contractile tissues (smooth muscles) of the brain and liver, and beta, concentrated in the endocrine and exocrine glands, heart and kidneys.
In 1958, pharmacologist James Black from Scotland got a job as a young specialist at ICI Pharmaceuticals, choosing the most promising area - pharmacotherapy to improve blood supply to the myocardium. Thanks to Black, the first beta blocker, propranolol, came off the production line in 1968. For his discovery and development, James Black was awarded the Nobel Prize in 1988 in the field of physiology or medicine.
Over the course of history, about a hundred drugs have been synthesized, 30 of them are used in modern practice. The latest revolutionary drug of the new generation, nebivolol, was developed in 2001. It combines the developments of previous generations with a small addition - a vasodilating effect.
Clinical pharmacology
Treatment with beta blockers must be carried out in effective therapeutic dosages, the dose of the drug is titrated once the target heart rate is reached in the range of 50–60 min-1.
Only when the target heart rate is achieved can one judge the effectiveness or ineffectiveness of the drug in relation to the condition for which the drug is prescribed for correction: angina pectoris, hypertension, arrhythmia.
For example, when treating hypertension with a beta blocker, systolic blood pressure remains at 150–160 mmHg. Art. If the heart rate does not decrease below 70 min-1, you should not think about the ineffectiveness of the beta blocker and its replacement, but about increasing the daily dose until the heart rate reaches 60 min-1.
An increase in the duration of the PQ interval on the electrocardiogram and the development of first degree AV block when taking a beta blocker cannot serve as a reason for its discontinuation. However, the development of II and III degree AV block, especially in combination with the development of syncope (Morgagni-Adams-Stokes syndrome), serves as an absolute basis for discontinuing beta blockers.
The cardioprotective effect of beta blockers is more typical for lipophilic drugs than for hydrophilic ones. The ability of lipophilic beta blockers to accumulate in tissues and increase vagal activity is important. Lipophilic beta blockers penetrate the blood-brain barrier better and may have greater CNS side effects.
Randomized clinical trials have established cardioprotective doses of beta blockers, i.e. doses the use of which statistically significantly reduces the risk of death from cardiac causes, reduces the incidence of cardiac complications (myocardial infarction, severe arrhythmias), and increases life expectancy. Cardioprotective doses may differ from those that achieve control of hypertension and angina. If possible, beta blockers should be prescribed at a cardioprotective dose that is higher than the average therapeutic dose.
It should also be taken into account that not all beta blockers have shown cardioprotective effects in randomized studies; only the lipophilic metoprolol, propranolol, timolol and the amphiphilic bisoprolol and carvediol are able to increase life expectancy.
Increasing the dose of beta blockers above the cardioprotective dose is unjustified, since it does not lead to a positive result, increasing the risk of side effects.
Chronic obstructive pulmonary disease and bronchial asthma
While beta-blockers cause bronchospasm, beta-agonists (such as the beta2-agonist salbutamol) can cause an attack of angina. The use of selective beta blockers helps: cardioselective beta1 blockers bisoprolol and metoprolol in patients with coronary artery disease or hypertension in combination with chronic obstructive pulmonary disease (COPD) and bronchial asthma. In this case, it is necessary to take into account the external respiration function (ERF). In patients with mild impairment of respiratory function (forced expiratory volume more than 1.5 l), the use of cardioselective beta blockers is acceptable.
In case of moderate and severe chronic bronchitis and bronchial asthma, you should refrain from prescribing beta blockers, including cardioselective ones.
When choosing treatment tactics in patients with hypertension, angina pectoris or heart failure in combination with COPD, the priority is the treatment of cardiovascular pathology. In this case, it is necessary to individually assess whether the functional state of the bronchopulmonary system can be neglected and vice versa - to relieve bronchospasm with beta-adrenergic agonists.
Diabetes
When treating patients with diabetes mellitus taking beta-blockers, one should be prepared for the more frequent development of hypoglycemic conditions, while the clinical symptoms of hypoglycemia change. Beta blockers significantly eliminate the symptoms of hypoglycemia: tachycardia, tremor, hunger. Insulin-dependent diabetes with a tendency to hypoglycemia is a relative contraindication to the use of beta blockers.
Peripheral vascular diseases
If beta blockers are used for peripheral vascular pathology, then cardioselective atenolol and metoprolol are safer.
Atenolol does not worsen the course of peripheral vascular diseases, while captopril increases the incidence of amputations.
However, peripheral vascular diseases, including Raynaud's disease, are included in the relative contraindications for the prescription of beta blockers.
Heart failure
While beta blockers are widely used in the treatment of heart failure, they should not be prescribed for class IV heart failure with decompensation. Severe cardiomegaly is a contraindication to beta blockers. Beta blockers are not recommended for ejection fractions less than 20%.
Heart blocks and arrhythmias
Bradycardia with a heart rate less than 60 min-1 (initial heart rate before the prescription of drugs), atrioventricular block, especially of the second degree or more, are a contraindication to the use of beta blockers.
Disadvantages of reception
In recent years, there has been an opinion that β-blockers should not be the first choice drugs in the treatment of vascular diseases. Thus, experts identify the following disadvantages when using them:
- Contribute to insufficient reduction of risks in the development of cardiac and vascular pathologies.
- They do not affect the functional state of the arteries, thereby not stopping the progression of atherosclerotic processes.
- They have reduced protection, as they do not sufficiently protect target organs from destruction.
There is also a possibility that under their influence there is a violation of fat and carbohydrate metabolism. As a result, a hypertensive person develops type 2 diabetes mellitus or worsens its course.
Representatives of the old generation (non-selective) cause many complications, one of which is sexual dysfunction in men. They impair blood flow to the penis, which disrupts the production of hormones. However, the modern class does not affect potency, so men can take them without fear.
Beta blockers are an effective group of medications, but their use must be agreed with a specialist. Before starting therapy, it is necessary to conduct a thorough diagnosis of the condition in order to prevent complications and side effects. During pregnancy, it is recommended to stop taking this group; their use may be permitted in cases where the benefits outweigh the risks. Most experts agree that β-blockers are effective after a heart attack and for preventing another heart attack. For arterial hypertension, medications are selected individually based on the indications and preferences of the attending physician.
Personal experience
It is likely that each physician has his own pharmacotherapeutic formulary, reflecting his personal clinical experience with drugs, preferences and negative attitudes. The success of using the drug in the first one to three to ten patients ensures the doctor's addiction to it for many years, and literature data strengthens the opinion of its effectiveness. Here is a list of some modern beta blockers that I have experience with in clinical use.
Propranolol
The first of the beta blockers that I began to use in my practice. It seems that in the mid-70s of the last century, propranolol was almost the only beta blocker in the world and certainly the only one in the USSR. The drug is still one of the most frequently prescribed beta blockers and has more indications for use compared to other beta blockers. However, I cannot consider its use at present justified, since other beta blockers have much less pronounced side effects.
Propranolol can be recommended in the complex treatment of coronary heart disease; it is also effective in lowering blood pressure in hypertension. When prescribing propranolol, there is a risk of developing orthostatic collapse. Propranolol is prescribed with caution for heart failure; if the ejection fraction is less than 35%, the drug is contraindicated.
According to my observations, propranolol is effective in the treatment of mitral valve prolapse: a dosage of 20–40 mg per day is enough for the prolapse of the valves (usually the anterior one) to disappear or significantly decrease from the third or fourth degree to the first or zero.
Bisoprolol
The cardioprotective effect of beta blockers is achieved at a dosage that provides a heart rate of 50-60 per minute.
A highly selective beta1 blocker that has been shown to reduce mortality from myocardial infarction by 32%. A dose of 10 mg of bisoprolol is equivalent to 100 mg of atenolol, the drug is prescribed in a daily dosage of 5 to 20 mg. Bisoprolol can confidently be prescribed for a combination of hypertension (reduces arterial hypertension), coronary heart disease (reduces myocardial oxygen demand, reduces the frequency of angina attacks) and heart failure (reduces afterload).
Metoprolol
The drug belongs to beta1‑cardioselective beta blockers. In patients with COPD, metoprolol at doses up to 150 mg/day causes less severe bronchospasm compared to equivalent doses of non-selective beta blockers. Bronchospasm when taking metoprolol is effectively relieved by beta2-adrenergic agonists.
Metoprolol effectively reduces the frequency of ventricular tachycardia in acute myocardial infarction and has a pronounced cardioprotective effect, reducing the mortality rate of cardiac patients in randomized trials by 36%.
Currently, beta-blockers should be considered as first-line drugs in the treatment of coronary heart disease, hypertension, and heart failure. The excellent compatibility of beta blockers with diuretics, calcium channel blockers, and ACE inhibitors is undoubtedly an additional argument when prescribing them.
Indications for the use of beta-blockers
- angina pectoris,
- acute coronary syndrome,
- Hypertension and primary prevention of stroke and ischemic heart disease in patients with hypertension,
- prevention of ventricular and supraventricular arrhythmias,
- prevention of recurrent myocardial infarction,
- prevention of sudden death in patients with long QT interval syndrome,
- chronic heart failure (carvedilol, metoprolol, bisoprolol, nebivolol),
- systemic diseases with increased influence of the sympathetic nervous system,
- thyrotoxicosis,
- essential tremor,
- alcohol withdrawal,
- dissecting aortic aneurysm,
- hypertrophic cardiomyopathy,
- digitalis intoxication,
- mitral stenosis (tachysystolic form),
- mitral valve prolapse,
- tetralogy of Fallot.
Scroll
1. Non-cardioselective beta blockers:
A. Without internal sympathomimetic activity:
- propranolol (anaprilin, obzidan);
- nadolol (korgard);
- sotalol (sotahexal, tenzol);
- timolol (blocarden);
- nipradilol;
- flestrolol.
B. With internal sympathomimetic activity:
- oxprenolol (Trazicor);
- pindolol (wisken);
- alprenolol (aptin);
- penbutolol (betapressin, levatol);
- bopindolol (Sandorm);
- bucindolol;
- dilevalol;
- carteolol;
- labetalol.
2. Cardioselective beta blockers:
A. Without internal sympathomimetic activity:
- metoprolol (betaloc, betaloc zok, corvitol, metozok, metocard, metocor, serdol, egilok);
- atenolol (betacard, tenormin);
- betaxolol (betak, lokren, kerlon);
- esmolol (breviblok);
- bisoprolol (aritel, bidop, biol, biprol, bisogamma, bisomore, concor, corbis, cordinorm, coronal, nipperten, tirez);
- carvedilol (acridilol, bagodilol, vedicardol, dilatrend, carvedigamma, carvenal, coriol, recardium, tallitone);
- nebivolol (binelol, nebivator, nebikor, nebilan, nebilet, nebilong, nevotenz, od-neb).
B. With internal sympathomimetic activity:
- acebutalol (acecor, sectral);
- talinolol (cordanum);
- celiprolol;
- epanolol (vasacor).
3. Beta blockers with vasodilating properties:
A. Non-cardioselective:
- amozulalol;
- bucindolol;
- dilevalol;
- labetolol;
- medroxalol;
- nipradilol;
- pindolol.
B. Cardioselective:
- carvedilol;
- nebivolol;
- Celiprolol.
4. Long-acting beta blockers:
A. Non-cardioselective:
- bopindolol;
- nadolol;
- penbutolol;
- sotalol.
B. Cardioselective:
- atenolol;
- betaxolol;
- bisoprolol;
- epanolol.
5. Ultra-short-acting beta blockers, cardioselective:
- esmolol.
Withdrawal syndrome
If beta blockers are used for a long time in high dosages, then sudden cessation of treatment can provoke the so-called withdrawal syndrome. It is manifested by an increase in angina attacks, the occurrence of ventricular arrhythmias, and the development of myocardial infarction. In milder cases, withdrawal syndrome is accompanied by tachycardia and increased blood pressure. Withdrawal syndrome usually manifests itself a few days after stopping the use of beta blockers.
To avoid the development of withdrawal syndrome, you must follow the following rules:
- discontinue beta blockers slowly, over two weeks, gradually reducing the dosage per dose;
- during and after discontinuation of beta blockers, it is necessary to limit physical activity and, if necessary, increase the dosage of nitrates and other antianginal drugs, as well as medications that lower blood pressure.